Introduction: the global challenge
The global burden of retinoblastoma (Rb) is one in 15,000-18,000 live births, which equates to 8000 new cases worldwide each year. The global disparities in Rb outcome represent a paradigm of health inequality worldwide [1]. In high-income countries, Rb is considered a curable disease, with survival rates reaching nearly 100% and management focussing on eye salvage and saving vision [1,2].
However, these positive success rates embody less than a tenth of Rb cases worldwide. Low- and middle-income countries (LMICs), mainly in Asia, Africa and Latin America, comprise more than 80% of children with Rb, with survival rates reaching 50% or less in these regions [1,3].
The Global Retinoblastoma Study Group, led by Didi Fabian, has highlighted the key differences in survival outcomes between economic levels across the world, demonstrating a near 17-times difference in survival rates between high-income and low-income countries [1]. This considerable difference calls for worldwide action to try to achieve health equality and improve outcomes for these children [1,4].
Rb and the World Health Organization Global Initiative for Childhood Cancer
The World Health Organization (WHO) Global Initiative for Childhood Cancer, launched in September 2018, aims to achieve at least a 60% survival rate and reduce suffering for all children with cancer by 2030 [4]. Rb represents one of six so-called ‘tracer cancers’ in this global initiative, which in total characterises 50-60% of childhood cancers. The tracer cancers are global indicators, as well as catalysts, for worldwide healthcare transformation and progress [2,4].
The WHO CureAll Framework
Specifically, the CureAll framework guides nations on implementing the global initiative through four pillars:
- Centres of Excellence and Care Networks
- Universal Health Coverage
- Regimens and Roadmaps for diagnosis and management
- Evaluation and Monitoring.
This package is implemented at a country, regional and global level, incorporating combined efforts between WHO offices, government sectors, nonprofit organisations, advocacy groups, private entities and philanthropic foundations. The initial focus countries piloting the initiative have been chosen from each of the six WHO regions and all have committed to prioritising childhood cancer care by incorporating the CureAll framework into national healthcare policies.
Through serving as one of the six tracers of the global initiative, Rb survival outcomes are expected to improve. Retinoblastoma presents substantial yet preventable challenges to survival in LMICs, such as late and advanced presentation, shortage of healthcare specialists, treatment abandonment, lack of awareness and others [5] – the situation for children in India is discussed as an example in the next section.
Many of the barriers to care are reflected in other cancers, so Rb serves as a key model for emphasising global prioritisation, capacity strengthening and developing governmental strategies [4]. Specifically, expansion of care networks and universal health coverage will promote early presentation and diagnosis of Rb, as well as increased disease awareness. The establishment of further Centres of Excellence, as well as the construction of treatment roadmaps, will lead to specialist recruitment and better disease management. Altogether, with continuous monitoring and improved evaluation, worldwide disparities in Rb care will hopefully be mitigated, demonstrating better survival outcomes and reduced patient morbidity, especially among LMICs [3].
Progress of this important initiative will be monitored, and new strategies for reducing child mortality will be developed, transforming paediatric cancer care worldwide. With proper execution of this new endeavour, Rb can become a paradigm of achieving health equality worldwide.
The Global Rb Network
The Global Rb Network initiatives were established in 2017, led by Marcia Zondervan and the VISION 2020 LINKS & Networks Programme at the International Centre for Eye Health, London School of Hygiene & Tropical Medicine (LSHTM), as a response to the disparities in outcome of Rb treatment, with the aims of saving lives, preserving the eye and vision and giving care and compassion to affected children and families throughout the world.
The Global Rb Network is in two parts: (1) The Rb-NET is a core network of Rb treatment centres in 10 countries (Tanzania, Uganda, Malawi, Kenya, Nigeria, Zimbabwe, Cameroon, The Gambia, Ghana, Indonesia), who are linked with experts from specialist Rb centres in the UK, India, Israel, Europe and the USA [6-10]; and (2) the Global Retinoblastoma Research Group (GRRG) is a research collaboration of over 200 Rb treatment centres in more than 150 countries working together to collect and publish information to improve the management of children with Rb worldwide.
The objectives of the Rb-NET are to:
- Share knowledge on how to diagnose and best treat retinoblastoma.
- Agree and share guidelines and protocols for effective diagnosis and treatment of Rb.
- Develop meaningful long-term capacity-strengthening partnerships between high-, middle- and low-resource treatment centres.
- Develop national action plans to improve Rb services.
- Coordinate and conduct multicentre studies to improve retinoblastoma outcomes.
Some of the achievements of Rb-NET in capacity-strengthening include:
- Three Rb planning workshops, bringing together Rb stakeholders to agree a plan of action for establishing Rb national referral pathways and exchange knowledge on Rb management.
- Twelve whole-team training visits, delivering training in diagnosis and management of Rb, including the Nigeria-Israel partnership visit which helped to introduce intra-arterial chemotherapy to Nigeria in 2023 [10].
- A comprehensive Rb Toolkit resource manual.
- A special edition of the Community Eye Health Journal dedicated to Rb [11].
- Online multidisciplinary team (MDT) meetings, in which the management of children diagnosed with Rb are discussed and their care is optimised [8]; international experts giving their time and expertise
- A dedicated website set up to host MDTs (www.rb-net-mdt.org). Over 450 Rb specialists from 40 countries have registered on the website and can access the MDTs. This forms a permanent information and training resource.
The GRRG has to date produced about a dozen papers, including the Global Outcome Study, highlighting the major disparities in survival outcomes between geographic location and economic status, thereby providing a baseline dataset for the CureAll global initiative standardisation and action planning [3].
Challenges of Rb in India
India carries the highest global Rb burden, with more than 1400 of the 8000 global cases diagnosed each year [12]. With a burgeoning population and a literacy rate of 78%, there are five major hurdles. First: a lack of awareness, leading to a delay in diagnosis and subsequent treatment. Mean age at presentation was reported as 34.7 months [13] and 29 months [14], compared with Western data which shows the mean presenting age to be 18 months [15]. Even in patients with bilateral disease, the mean age of presentation was 24 months, showing the dearth of awareness about the heritable nature of the disease [14].
A consequence of delayed presentation is that children present with advanced disease, resulting in poor chances of globe salvage. A multicentre international epidemiological study showed that of 666 children from high-income countries (HICs), 99% had intraocular tumours and hence a favourable prognosis, while in LMICs, of the 3685 patients studied, 25% had tumour extension beyond the globe, indicating a poor prognosis [16]. There is also a potentially large cohort of patients who have not reported to an Rb treatment centre and who could have succumbed to the disease.
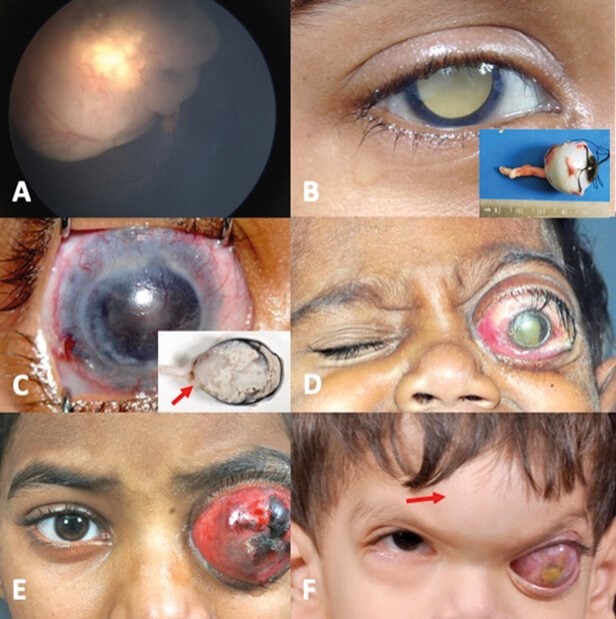
Figure 1: Stages of retinoblastoma disease. (A) Stage 0; (B) Stage I with no microscopic tumour residue; (C) Stage II with microscopic tumour residue due to extraocular tumour noted after enucleation (red arrow); (D) Stage III with optic nerve tumour extension; (E) Stage III with extraocular tumour extension; (F) Stage IV disease with bony metastasis (red arrow). S Kaliki with permission
While recent advances in Rb management become available at more and more Rb treatment centres, better globe salvage can be achieved only if the children present early. This requires efforts towards increasing awareness about Rb amongst the general public and medical practitioners. Early referral remains a key to improving globe salvage rates in India.
A second hurdle in India and LMICs is the increased lag time between the first symptom and treatment, being 3.2 times higher than in HICs [17]. Lag time of greater than six months is associated with metastases and mortality [17]. One of the factors noted to be associated with increased lag time was the increased number of primary health care visits, denoting the paucity of a strong referral system for Rb patients from primary care physicians to tertiary Rb treatment centres. Increased awareness about Rb at all levels of healthcare is of utmost importance to strengthen the referral system in India.
Thirdly, while no gender bias was seen in the study by Kaliki, et al. [14], Singh, et al. [13] found a male gender bias of 62% in seeking Rb care. This suggests an alarming possibility that health problems in female children are being ignored. Parents’ acceptance of gender equality in seeking Rb care needs to be improved to ensure improved outcomes irrespective of gender.
Fourthly, treatment for Rb becomes a financial burden with recurring treatment costs including travel, accommodation, and loss of parental wages. With low insurance coverage and few centres offering free treatment, this becomes a huge financial burden for the family. While the parents start the treatment without considering these factors, the reality hits them due to recurrent expenses, resulting in non-compliance to care and compromised outcomes.
The vast majority of patients either end up dropping out before completion of therapy or are forced to delay treatment until they find viable cost-effective options. Intra-arterial chemotherapy, commonly practiced in HICs, is often far beyond the paying capacity of the average Indian family. Government intervention in identifying Rb treatment as critical care and making critical health care available to all, free of cost, may benefit Rb children and parents. Affordability and accessibility to appropriate health care should remain the right of every child with Rb.
A fifth hurdle is refusal of enucleation (removal of the eye). While vision and globe salvage are desirable, saving life remains the primary goal. Despite best efforts for globe salvage, enucleation is required in certain scenarios. Social stigma surrounding enucleation is still prevalent in India, with Singh, et al. reporting an enucleation refusal rate of 21% [13]. The typical Indian ophthalmologist may be trying to persuade families to accept it by themselves in a busy clinic.
In contrast, in HICs, even though enucleation is less commonly needed, priority is given to counselling of parents regarding enucleation. There needs to be ‘buy in’ from the parents, which takes time and patience. The MDT comes to the fore and specialist nurses with experience in counselling spend many hours in discussion with the parents. The thought of enucleation terrifies parents, so photos of children who have had enucleations with good cosmesis are essential. The positive impact of support and counselling, including psychology input, on parents and children as they grow up has been reported in the UK [18]. Efforts should be made towards educating parents about the benefit of enucleation when required.
Hand in hand with this supportive approach for patients who require enucleation is the need for better understanding about which patients do not require eye removal. In the UK, 80% of children with Rb were enucleated in the 1990s. This reduced to 60% a decade ago and now is below 40%. With advanced Rb (Group E or cT3c), only 39% were shown to have High Risk Features after enucleation [19], which suggests that more than half of these patients are being primarily enucleated unnecessarily. Understanding tumour biology better may allow better globe salvage, which requires more collaborative research between high-, low- and middle-income countries.
Despite the hurdles, the results of an extensive longitudinal analysis comparing the data of Rb patients in three temporal groups (2000-2005, 2006-2010, and 2011-2015) offer a beacon of hope, with the age at presentation gradually decreasing for female children, a decreasing trend of occurrence of extraocular extension and rate of denial of treatment, an increase in the use of systemic chemotherapy and a reduced rate of primary enucleation [14]. With further efforts from parents, society, and the government, the outcomes of Rb children can further improve in India.
Summary
In summary, the last six years have seen huge progress in global collaboration to address the shameful disparity in outcome of children with Rb from richer and poorer countries. This should be celebrated at the same time as highlighting remaining challenges where further global collaboration can make a real difference.
References
1. Fabian ID, Abdallah E, Abdullahi SU, et al. Global Retinoblastoma Presentation and Analysis by National Income Level. JAMA Oncol 2020;6(5):685-95.
2. Lam CG. Retinoblastoma as a lens for correctable disparities worldwide. Lancet Glob Health 2022;10(8):e1074-5.
3. Fabian ID, Abdallah E, Abdullahi SU, et al. The Global Retinoblastoma Outcome Study: a prospective, cluster-based analysis of 4064 patients from 149 countries. Lancet Glob Health 2022;10(8):e1128-40.
4. World Health Organization. The Global Initiative for Childhood Cancer.
https://www.who.int/initiatives/
the-global-initiative-for-childhood-cancer
[last accessed August 2023]
5. Tomar AS, Finger PT, Gallie B, et al. Global Retinoblastoma Treatment Outcomes: Association with National Income Level. Ophthalmology 2021;128(5):740-53.
6. Williams P, Bowman R, Foster A, et al. Rb-NET: a network to save life and preserve vision in children in Africa. Eye News 2018;24(6):32-4.
7. Makan M, Reddy MA, Naeem Z, et al. Development of retinoblastoma services in Zimbabwe. Eye News 2020;27(1):22-5.
8. Fabian ID, Astbury N, Nkanga E, et al. The role of virtual Rb-NET Multidisciplinary Team meetings in the management of children with retinoblastoma in low- and middle-income countries. Eye News 2021;27(6):36-8.
9. Oktarima P, Kuntorini MW, Susanty A, et al. Development of retinoblastoma care in Indonesia and the role of multidisciplinary team meetings. Eye News 2021;28(2):36-8.
10. Arazi M, Bowman R, Fabian ID, et al. Establishing an intra-arterial chemotherapy service for children with retinoblastoma in Nigeria for the first time. Eye News 2023;29(6):32-6.
11. Retinoblastoma: a curable, rare and deadly blinding disease. Comm Eye Health 2018;31(101).
12. Usmanov RH, Kivelä T. Predicted trends in the incidence of retinoblastoma in the Asia-Pacific region. Asia Pac J Ophthalmol (Phila) 2014;3(3):151-7.
13. Singh U, Katoch D, Kaur S, et al. Retinoblastoma: A Sixteen-Year Review of the Presentation, Treatment, and Outcome from a Tertiary Care Institute in Northern India. Ocul Oncol Pathol 2017c;4(1):23-32.
14. Kaliki S, Patel A, Iram S, et al. Retinoblastoma in India: Clinical Presentation and Outcome in 1,457 Patients (2,074 Eyes). Retina 2019;39(2):379-91.
15. Shields JA, Shields CL. Retinoblastoma: introduction, genetics, clinical features, classification. In: Shields JA, Shields CL (Eds.). Intraocular Tumors: An Atlas and Textbook, 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:294-300.
16. Global Retinoblastoma Study Group. Global Retinoblastoma Presentation and Analysis by National Income Level. JAMA Oncology 2020;6(5):685-95.
17. Kaliki S, Ji X, Zou Y, et al. Lag Time between Onset of First Symptom and Treatment of Retinoblastoma: An International Collaborative Study of 692 Patients from 10 Countries. Cancers (Basel). 2021;13(8):1956.
18. Gibbs D, Reynolds L, Shea Yates T. Understanding the Experiences of Living With an Artificial Eye in Children With Retinoblastoma-Perspectives of Children and Their Parents. J Pediatr Hematol Oncol Nurs 2022;39(4):250-63.
19. Kaliki S, Srinivasan V, Gupta A, et al. Clinical features predictive of high-risk retinoblastoma in 403 Asian Indian patients: a case-control study. Ophthalmology 2015;122(6):1165-72.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME