Zimbabwe recognised the need for a paediatric ophthalmology service almost 20 years ago. The economic uncertainty in the country made it difficult to secure financial support, so initial funding came through local donors.
Equipment – including vision charts, ophthalmoscopes and a keratometer – was donated by the Alfred Beit Trust to the Ministry of Health in 2012. The first paediatric ophthalmology service in the country was thus born at the central referral eye unit in Harare, Sekuru Kaguvi Eye Unit, which is part of Parirenyatwa Hospital.
A VISION 2020 LINK was established in 2012 between the Sekuru Kaguvi Eye Unit and the Royal London Hospital led by Mayuri Makan in Harare and M Ashwin Reddy in London [1]. The LINK is part of the VISION 2020 LINKS Programme of the International Centre for Eye Health, London School of Hygiene & Tropical Medicine. Eye units in hospitals in the United Kingdom are linked to their counterpart units in low- and middle-income countries, especially in Africa.
“Caregivers play an important role in the treatment and recovery process. During the retinoblastoma clinic we include the caregivers in all discussions so that they are aware of the situation and we are there to offer knowledge and support”
Sister Lennety Tafirenyika, Sekuru Kaguvi Eye Unit, Harare.
Eye health care in Zimbabwe
In Zimbabwe patients are referred through the primary health care structure from the grassroots rural clinics to district then provincial level and through to the central referral hospital when necessary. The training of post-basic ophthalmic nurses has provided increasing access to ophthalmic care up to district level over the last 15 years. Travel to access care is usually the rate-limiting step; patients will come but cannot always afford to travel sufficiently quickly. The government subsidises all care for patients under the age of five years and families that are referred are well counselled by referring practitioners and tend to accept the treatments offered when they arrive.
Development of paediatric ophthalmology services
Through the LINK, Ashwin Reddy put together a team with the appropriate skills to make training visits to Harare. Initially two ophthalmologists and nurses with post-basic training in ophthalmology were trained. The nurses were trained by orthoptists in paediatric visual acuity assessment across various age groups. We acknowledge Professor Gordon Dutton for his donation of the first Cardiff Acuity and contrast tests to the clinic. Dedicated child- friendly services, both for inpatients and outpatients were now offered. Continuity of care from a small team resulted in better monitoring and visual outcomes. Visits were also made by the Harare team to the Royal London Hospital, Barts Health NHS Trust.
Two surgeons were trained in paediatric surgery by Ashwin Reddy and Richard Bowman. The paediatric service started with squint and cataract surgery. Mr Reddy helped to structure the Rb service and Himanshu Patel led the teaching of screening for retinopathy of prematurity.

Visit of the Harare team to LV Prasad Eye Institute, India.
‘Seeing is Believing’ funding
In 2015, Standard Chartered [2], through its ‘Seeing is Believing’ initiative, provided support to the paediatric service and it grew to offer services to the north eastern part of Zimbabwe. It also became the training ground for the ophthalmologist who is now at the second paediatric ophthalmology service in Bulawayo, serving the south western part of the country. In Harare the clinic was renovated to specifications requested by the local team after their exchange visit to the Royal London. Workflows were observed there and adjusted to the local situation. This support also brought training in low vision as well as a clinic coordinator.
Case Study 1: Reflections on the training visit
to Sekuru Kaguvi Eye Unit, Harare in January 2020
Zishan Naeem, Senior Orthoptist, Royal London Hospital
It was clear that the nurses who had visited the Royal London in August 2019 had implemented a number of changes to their practice since their visit. They now use a range of toys to assess visual behaviour in Rb patients as well as low vision patients. They also now have access to a range of visual acuity tests, funded by Christian Blind Mission (CBM). The accuracy of visual acuity assessment has greatly improved. I was impressed with the variety of low vision aids available at Sekuru Kaguvi.
Following on from August 2019, the nurses had produced a proforma which was completed for each patient to record the results of all relevant assessments as well as advice relating to classroom placement at school, enlarging of print and so on. The form had however made the assessments lengthy and time-consuming, and patients often lost interest. During the visit the nurses asked for help in reducing the length of the form and the assessment time. We worked together to develop more specific lifestyle questions in order to understand which areas of their day-to-day life they needed help with using low vision aids. The new format greatly shortened the assessment time.
It was highlighted during the visit that monocular vision information for parents / school needed to be clearer and more concise too. We brainstormed ideas and revised the monocular vision advice form to a more concise version. This has since been introduced to the Royal London too.
Case Study 2: Retinoblastoma
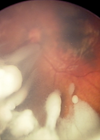
PM, a 10-month-old girl, presented to a private eye clinic in a small town outside Harare. Both parents were present and gave a history of seeing ‘something white’ in the left eye occasionally, usually early morning or in the evening. They had initially presented to their local clinic and were prescribed an ointment for what they were told was likely to be an infection.
Upon dilation at the eye clinic, the leukocoria was apparent and the need for further evaluation at the referral Children’s Eye Clinic was emphasised. The family presented the next day and B-scan examination was used to show the tumour. The parents were willing to allow ophthalmic nurses from other provinces who were participating in a retinoblastoma training workshop to examine their daughter. This training was the first in a series to improve detection and referral to the appropriate paediatric ophthalmic centre. The importance of a high index of suspicion and a dilated examination with the Arclight, a low-cost direct ophthalmoscope, was emphasised. After an examination under anaesthesia, which was scheduled for the next day, the parents were informed of the diagnosis. They were counselled for enucleation of the affected eye and booked for the first cycle of chemotherapy.
Not all families take up the treatment options offered after the first visit. The trauma of being informed of the diagnosis and the need for enucleation in the initial visit has been recognised. It is thought to be the reason that families disappear and look for other treatment options before coming back with advanced disease. Because of this, chemoreduction is emphasised as the first option of treatment. Enucleation is then discussed after the examination under anaesthesia.
Retinoblastoma Network, Rb-NET
The Retinoblastoma Network (Rb‑NET), began in 2017 with initially seven institutions in Kenya, Tanzania and Uganda in partnership with two institutions in India (LV Prasad Eye Institute, Hyderabad and Sankara Nethralaya, Chennai) and two in the UK (Royal London and Birmingham Children’s Hospital) [3]. Thanks to funding from the Queen Elizabeth Diamond Jubilee Trust [4], exchange training and capacity-building visits focusing on enhancing detection and management of retinoblastoma (Rb) were undertaken between the centres in Africa, India and the UK. Within the UK the number of Rb cases presenting late is extremely low but the centres in India see a higher proportion presenting late and therefore have vital experience to share with partners in Africa.
XOVA Award
XOVA is an award programme sponsored by Novartis Pharma AG. The objective of XOVA is to provide funding, in the form of a grant, for non-profit initiatives and projects that are expected to have a positive impact on improving the quality of eye care. In 2018 the VISION 2020 LINK between Harare and the Royal London won one of the awards, enabling the Harare team to join Rb-NET and benefit from Rb training visits alongside teams from Kenya, Tanzania and Uganda.

Visit of the Harare team to the Royal London Hospital.
In 2019 a core team of two ophthalmologists and four ophthalmic nurses from Zimbabwe visited the retinoblastoma services in London and at LV Prasad Eye Institute, Hyderabad, India. This has resulted in the first subspecialty clinic in paediatric ophthalmology focusing on retinoblastoma in Harare.
The most recent visit in this tripartite training was by the UK team to Zimbabwe in January 2020. Ashwin Reddy focused on the importance of regular examinations under anaesthesia for affected patients and those at risk. He also led a ‘train the trainers’ workshop in assessing babies for leukocoria with the Arclight, a low-cost ophthalmoscope. We acknowledge the contribution of the loupes and the Arclights that were donated.
The importance of counselling was emphasised by Gemma Melisi, the Healthcare Play Specialist at the Royal London. As a result, a structured system which is culturally appropriate is being set up with a local psychiatrist and psychologist in Harare.


Zishan Naeem with patients and staff of the paediatric ophthalmology service, Harare.
Zishan Naeem, Specialist Orthoptist in the retinoblastoma service at the Royal London, updated the staff on visual acuity testing. He also assisted in refining the rehabilitation plan for children with monocular vision that was created by the local team.
Zimbabwe has made remarkable progress in paediatric ophthalmology in the last eight years. The persistence and determination of a handful of individuals committed to the cause has resulted in the country meeting the World Health Organization (WHO)-recommended level of paediatric ophthalmology services for the size of the population. Paediatric ophthalmology is now incorporated in teaching both in the Masters in Medicine (Ophthalmology) programme as well as the post-basic ophthalmic nursing. The Ministry of Health continues to support this service as reflected in the National Eye Health Strategy.
As part of awareness of paediatric eye conditions and in particular Rb, the next step is to equip the district ophthalmic nurses with the Arclight to do dilated fundoscopy in children with leukocoria and to counsel and refer appropriately. Strengthening the Rb clinic will improve outcomes for the patients and reduce mortality. Early identification, appropriate referral and timely intervention are critical in achieving good outcomes.
References
1. Zondervan M, Hampejsková L, Abuh S, et al. VISION 2020 LINKS: Retinoblastoma in Africa. Eye News 2015;22(3):32-5.
2. Standard Chartered:
https://www.sc.com/uk/
3. Williams P, Bowman R, Foster A, et al. Rb-NET: a network to save life and preserve vision in children in Africa. Eye News 2018;24(6):32-4.
4. The Queen Elizabeth Diamond Jubilee Trust:
https://www.jubileetribute.org/
COMMENTS ARE WELCOME