Responding to need is a key element underpinning the VISION 2020 LINKS Programme [1]. It is embedded in the process through which LINKS are established, with institutions in low- and middle-income countries (LMICs) first defining their priority areas of training need and then being matched with a UK institution with the relevant capacity and expertise. Initial needs assessment visits to each institution ensure that the partners are keen to work together and that areas of need not originally identified as priorities are not overlooked.
Since 2004, when the VISION 2020 LINKS Programme was established, a need repeatedly identified has been assistance in the management of retinoblastoma (Rb). During the last year the VISION 2020 LINKS Programme has developed a new LINKS network to support and coordinate action on Rb within and between LINKS. This article explains the impact of Rb and the process of setting up a new network.
Why retinoblastoma?
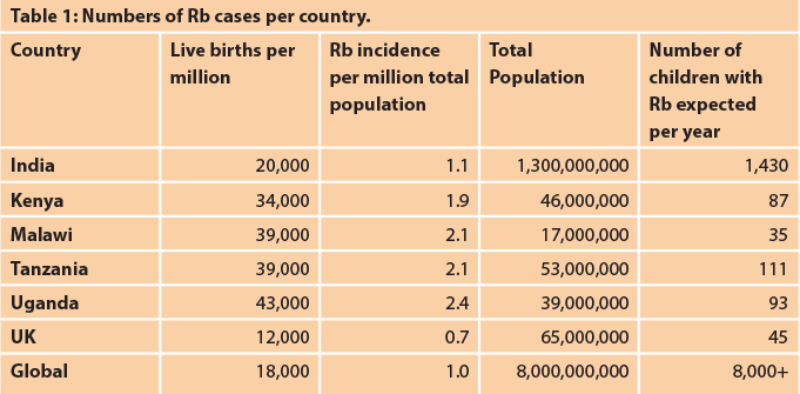
Retinoblastoma (Rb) is a rare but deadly cancer, which affects approximately 9000 children globally per year. It is the most common intraocular malignancy of childhood, with an incidence estimated at 1:18,000 live births. Rb can be bilateral or unilateral; all bilateral and about 15% of unilateral cases have germline mutations, so genetic counselling is important for families. There are no validated geographic, racial, gender or other population risk factors for the disease. The greatest disease burden is in large populations with high birth rates, which is also commonly a characteristic of LMICs. This means that the disease burden falls largely in LMICs. For example, in the US, 250 patients are diagnosed every year, and in the UK, approximately 50. In comparison, it is estimated that over 1000 cases occur in India each year, and a similar number in Africa. Retinoblastoma in sub-Saharan Africa was reviewed in Eye News in 2015 [2].
With Rb the first aim is to save life and then if possible the eye and sight. In recent years there has been a rapid evolution in the management of Rb, such that in high-income countries survival can be as high as 98%. In addition, in many cases where previous treatment would have included enucleation of the eye, there is now salvage of the eye and occasionally vision. Improvements in the management of Rb have also focused on the development of screening programmes for those at risk and on new treatment modalities. However, the associated improvement in outcomes is largely contained within high-income countries; tragically, in low-income countries most children still die from Rb [3].
Establishing a network: Rb-NET
Rb-NET follows the network model developed by the VISION 2020 LINKS Programme. The networks are a mechanism to facilitate the sharing of knowledge and coordination of action in a specific area that is a priority across several LINKS. To date, networks for diabetic retinopathy and leadership have been established [4-6].
Rb-NET began with seven institutions in Kenya, Tanzania and Uganda in partnership with two institutions in India (LV Prasad Eye Institute (LVPEI), Hyderabad and Sankara Nethralaya, Chennai) and two in the UK (Barts / Royal London and Birmingham). The institutions in India and the UK all provide Rb tertiary level services. The involvement of the centres from India shows how the LINKS model has evolved to draw on the most relevant expertise. Within the UK the number of Rb cases presenting late is extremely low but the centres in India see a higher proportion presenting late and therefore have vital experience to share with all the network partners in the UK, Africa and Asia.
The VISION 2020 LINKS programme is very grateful to have received funding from the Queen Elizabeth Diamond Jubilee Trust to establish the Rb-NET [7]. Institutions from Malawi, Zimbabwe and Indonesia have also joined the network through alternative funding sources.
Reviewing prosthetic eyes during the tour of LVPEI Rb services.
Setting priorities
An initial planning meeting was held in London in May 2017 and attended by participants from Kenya, Malawi, Tanzania, Uganda, India and the UK. The focus of the meeting was to prepare for the main stakeholder planning workshop, to be held in June 2017. It also provided an opportunity for participants to visit the Rb units in Birmingham and London.
The purpose of Rb-NET was defined as to improve:
- the survival of children with Rb
- the salvage of the eye and vision of children with Rb
- the quality of life of children with Rb
Plenary sessions were held in order to share best practice and working groups were held to review and discuss the outcome of a baseline needs assessment questionnaire.
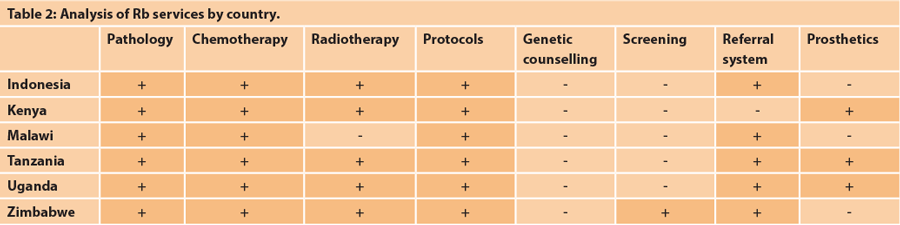
The results of the questionnaire, completed by each centre prior to attending, showed two main findings. Firstly the number of cases per live births was very similar across the centres, indicating that most children with Rb are seen by medical services (although this is often very late in the disease progression). Secondly the results suggested that different protocols were in use in different countries.

Participants in the Rb-NET workshop in Hyderabad in June 2017.
Working group sessions were also held to ascertain the expectations and needs of the participating centres and countries. From this discussion it was defined that the aim was to establish a sustainable network, in which all members aimed to:
- develop a national strategy on Rb for each country
- decide on a common classification for use across the network
- review existing protocols and work towards common protocols
- identify measurable outcomes
This activity fed into setting the agenda for the main June workshop.
Sharing knowledge and creating guidelines
The main stakeholder workshop was held from 9-11 June 2017. The meeting was hosted by the LVPEI, Hyderabad, India. The meeting was attended by 64 participants from India, Indonesia, Kenya, Malawi, Uganda, Tanzania and the UK. As with many diseases, a multidisciplinary team is involved in the management of Rb. As such, attendees included ophthalmologists, paediatricians, oncologists, pathologists, nurses and policy makers - Ministry of Health representatives with responsibility for Eye Health and Maternal and Child Health.
The objectives of the meeting were threefold:
- to share knowledge
- to develop partnerships and mentorships
- to decide how to evaluate the network’s activities in order to improve
The workshop began with a visit to LVPEI, to observe their Rb services. The second and third days consisted of morning plenary sessions and afternoon working groups. Lectures covered epidemiology, health education and early identification, classification – clinical and pathological, management of Rb (intraocular and extraocular), chemotherapy and radiotherapy. There were a number of case studies for discussion and country presentations on how Rb is managed. Technical working groups covered specific areas for the sharing of knowledge across partners – oncology, pathology and research – while country working groups developed action plans to tackle the specific priority needs for each country.
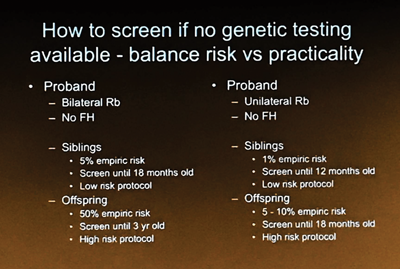
The presentations and discussions were collated in a detailed workshop report. A Resource Manual for Retinoblastoma Management in Low and Middle Resource Settings was created following the workshop. The manual covers guidelines for screening, pathology, staging, treatment and the provision of counselling for those affected by Rb.
As a result of discussions at the workshop, the members of the network agreed to report on monthly core indicators. These indicators will enable the network to monitor the presentation, treatment and outcomes of Rb across the network.
A slide from the workshop showing the practical approach to
management of Rb when genetic testing is not available.
Wider value of the network
Although this description of the network’s aims seems to be directed at improving clinical management, the network provides much more. It also provides support on a personal level for the health workers involved in the management of Rb. It provides health workers, who may work in small teams and see few Rb patients, with connections and motivation to improve their skills. Feedback from the workshop participants demonstrated the value of this element of the network:
“We know the difficulties in every country and we know from that, we’re not alone.”
“Now I am part of a network where I can consult colleagues and not work in isolation.”
“It has added value to my knowledge that Rb is curable once diagnosed and managed early….. It’s a life-saving workshop for the population of East Africa.”
Building an evidence base
As well as action to improve the treatment and outcomes for individuals with Rb, the network identified a need to construct the evidence base. Building a more complete picture of Rb can:
- provide a basis for improving treatment and management of Rb
- provide a basis for gaining future funding
- be used as a tool to influence decision makers
- influence funding and policies in respect to Rb management
It was agreed to establish a research working group for the network. The initial research project agreed by the group is focused on the presentation of Rb. As far as is known, there has never been a study on a global scale, in which data from centres in low- and high-income countries have been analysed and presented together. The study initially started with the 11 centres involved in the network. It has grown rapidly and, to date, 200 Rb centres from 120 countries from all continents have joined this global collaboration.
Addressing late presentation of Rb
The most significant factor influencing the outcome of a child with Rb is the presentation status. A child presenting with advanced extraocular disease (i.e. intracranial extension or distant metastases) is likely to die even in a well-equipped centre with state-of-the-art imaging and treatment.
There is a need for a screening programme that is suitable and scalable for low-income countries. The ‘Seeing is Believing’ grants programme of Standard Chartered Bank [8] is funding a pilot of two new technologies for use in screening. There is a need for a simple technique that can be used by non-eye-specialist health workers, specifically those who conduct under-five immunisation campaigns, as they come into frequent contact with babies and young children. Led by Richard Bowman, Consultant Paediatric Ophthalmologist at Great Ormond Street Hospital and Senior Lecturer at LSHTM, Rb-NET centres in Tanzania and Uganda are involved in the pilot. Malawi is also participating through funding from the Scottish Government via its Malawi Development Programme [9].
Looking ahead for the network
As evidenced in this article, the stakeholder workshop has already kick-started action in many areas across the network. Over the next year the LINK partners will also undertake reciprocal partnership training visits to develop and strengthen Rb services in each participating centre.
References
1. International Centre for Eye Health
http://iceh.lshtm.ac.uk/
2. Zondervan M, Hampejsková L, Abuh S, et al. VISION 2020 LINKS: Retinoblastoma in Africa. Eye News 2015;22(3);32-5.
3. Bowman RJ, Mafwiri M, Luthert P, et al. Outcome of retinoblastoma in east Africa. Pediatr Blood Cancer 2008;50:160-2.
4. Poore S, Foster A, Zondervan M, et al. Commonwealth nations join forces to prevent blindness from diabetes. Eye News 2015;21(5):33-6.
5. Astbury N, Burgess P, Foster A, et al. Tackling diabetic retinopathy globally through the VISION 2020 LINKS Diabetic Retinopathy Network. Eye News 2017;23(5):1‑4.
6. Williams P, Bailey M, Bascaran C, Zondervan M. VISION 2020 LINKS: collaborating across the Caribbean to tackle diabetic retinopathy. Eye News 2018;24(4):26-31.
7. The Queen Elizabeth Diamond Jubilee Trust
http://www.jubileetribute.org/
8. Standard Chartered Bank
https://www.sc.com/en/
9. Development assistance programmes. Scottish Government.
https://beta.gov.scot/policies/
international-development/
development-assistance-programmes/
(All links last accessed December 2017).
COMMENTS ARE WELCOME