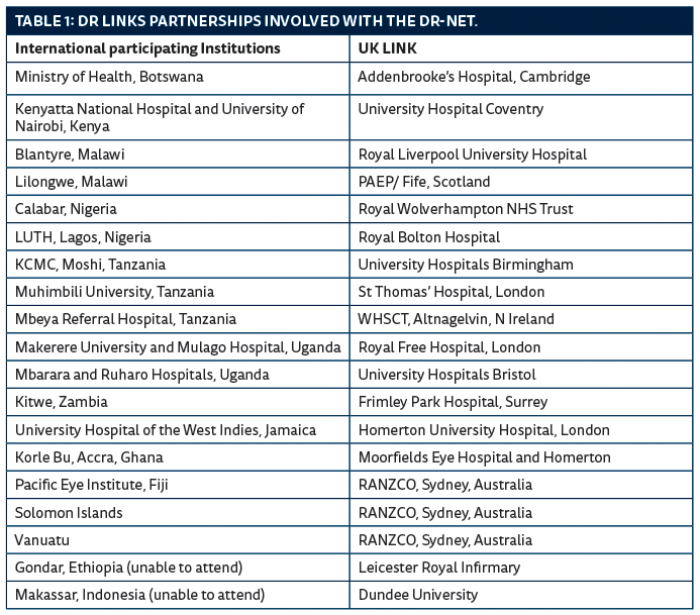
It is abundantly clear that the burden of diabetes is rapidly increasing, as there are now 415 million adults with diabetes in the world, with a projected rise to 642 million by 2040 [1]. This equates to 1 in 10 people. Approximately 10% of adults with diabetes will have sight-threatening diabetic retinopathy [2] requiring immediate treatment to prevent blindness. To combat this threat, the Diabetic Retinopathy Network (DR-NET) was established in 2014 and has now increased to 17 paired eye institutions, all part of the VISION 2020 LINKS Programme, with funding from the Queen Elizabeth Diamond Jubilee Trust.
At the inaugural workshop held in November 2014, each of 15 LINK teams developed a two-year action plan for their DR services, specific to their national or regional situation. In addition, the resolve was made by the 15 LINKS teams to increase their treatment outputs by at least one patient per week. Over the five years of the project this would equate to the prevention of 37,500 years of blindness.
Two years ago we reported on the newly formed DR-NET (‘Commonwealth nations join forces to prevent blindness from diabetes’ – Eye News February/March 2015) and last year described the situation in 11 countries that were all part of the DR-NET (‘Situation analysis of diabetic retinopathy services in 11 countries’ – Eye News December/January 2016). This October, almost halfway through the project, a DR-NET planning and review workshop was held in Durban, South Africa, alongside the Queen Elizabeth Diamond Jubilee Trust’s DR Advocacy Workshop.
This article describes that meeting, its aims, achievements and future plans for the DR-NET project and summarises the plenary sessions on epidemiology and advocacy.
The Botswana team – participants at the DR-NET planning workshop.
Intended outcomes
The intended outcomes of the DR-NET planning workshop in Durban were that each partner would:
- Review and build on the progress made in 2015 and 2016.
- Develop local and national activity plans for 2017-2019 using the DR Toolkit guide.
- Share learning so that practical improvements can be made in 2017-2019.
Each delegate was provided with a practical toolkit guide [3] to help develop their country’s DR services and was expected to contribute to an action plan specific for their LINK, including training visits over the next two years.
Some 70 invited participants from 17 individual institution-to-institution VISION 2020 LINKS partnerships (between Africa, Caribbean and Pacific countries and their UK partners) worked together to develop and implement their local and national plans for DR services.
The overall programme consisted of plenary sessions on the epidemiology of global diabetes and its control (Dr David Cavan and Professor Clare Gilbert) and effective advocacy for DR, based on experience from the work of the Public Health Foundation of India (Professor GVS Murthy).
Epidemiology of diabetic retinopathy
It is remarkable enough to realise that there will be a 50% increase in diabetes in the next 25 years but more amazing still is the fact that at least 50% of those people with diabetes are undiagnosed and have no idea they have the disease. This calls for strategies of primary prevention, secondary prevention of complications and tertiary prevention of sight loss. Successful strategies for reducing the incidence of diabetes include lifestyle programmes and legislation of foodstuffs so that individuals with diabetes can work towards achieving lower HbA1c levels and reducing their blood pressure. A 1% reduction in HbA1c can lead to a 37% reduction in microvascular complications [4]. Prof Clare Gilbert explained that a health systems approach is necessary as health systems function in the context of socio-economic, ecological, policy and cultural environments.
Services for DR are different from the “one-stop” model used for cataract and refractive error. They require services that involve patient participation in care, proactive case detection, responsive location and timing of services, and continuity of care from home to hospital. It is vital that services are equitable and do not impoverish individuals and families. Progress will require national policies, district level planning and co-ordination, capacity building, education and awareness of primary care providers, community engagement and integration of services into Non Communicable Disease (NCD) programmes.
The Indian perspective
Many useful lessons have been learnt from the work of the Public Health Foundation of India which has developed diabetes programmes in partnership with national government, state governments and Non Governmental Organisations (NGOs). A Ministry of Health (MoH) task force was an essential element, with integration of programmes into all levels of government health services. Expert groups gave technical advice and underpinning all the programmes was the generation and use of evidence for policy change and programme development.
Although there were regional differences there were common features which included 1. National guidelines, 2. Pilot programmes for control of diabetes, 3. Early detection and management of diabetic retinopathy, 4. Enhanced capacity health workforce and 5. Empowerment of patients and families.
In many countries ophthalmologists and diabetes physicians do not work together – to the detriment of their patients. In India it has been realised that acceptance of the philosophy of integration has been key to success. Not only doctors working together but also NGOs and government, and blindness programmes working with NCD programmes. This is especially relevant given the current prominence of NCDs in policy making. For those who like alliteration this piece of advice was considered essential for success: Persistence, Perseverance and Patience!
Effective advocacy – lessons from India
In India there are 70 million underserved people with diabetes where services are often excellent but fragmented. A situational analysis was performed over four months involving clinical gurus, the Public Health Foundation of India and the London School of Hygiene & Tropical Medicine (LSHTM). There was democratic and transparent consultation with stakeholders followed by a national summit, after which the Government convened a National Task Force to tackle the problem.
The Indian experience has shown that advocacy in addition to good communication can lead to changing attitudes and behaviour, but advocacy requires a process – there are goals to be identified, and there must be adequate capacity to deliver what is promised in order to give credibility. Integration is the key – ophthalmology, primary care and diabetes services and medical and MoH personnel.
Stages in the process are listed in Table 2.

Prof Murthy quoted the chronic disease ‘rule of halves’ as it is particularly relevant for diabetes and diabetic retinopathy and demonstrates how far we have to go to tackle the burden of diabetic eye disease:
- Half are not aware of disease (50%)
- Half are not engaging with services (25%)
- Half are getting treatment (12.5%)
- Half are treated to target (6.25%)
Manifesto
One output of the Trust’s advocacy meeting was an eight-point manifesto entitled ‘Preserving the sight of people with diabetes across the Commonwealth’ (Table 3). The intended audience is anyone whose actions or policies could affect the health of people with diabetes. The manifesto includes the principle that ophthalmology teams must integrate with other healthcare professionals to deliver an holistic service for people with diabetes, the prevention of which is key to preserving sight, as well as its many other complications.
Delegates for the DR-NET planning and review workshop and the Queen
Elizabeth Diamond Jubilee Trust’s DR Advocacy Workshop.
Country action plans: progress since 2014
At the start of the meeting the LINKS partners gave presentations on their progress since the start of the project in 2014.
Overall there has been an increase in numbers screened and treated and more health workers and allied professionals have been trained. ‘Task-shifting’ has enabled eye care personnel to be utilised more efficiently as members of a team. The DR-NET web platform has been used for sharing resources and housing a database for monthly statistics [5].
Issues included lack of suitably qualified screener / graders, malfunctioning equipment and insufficient anti-VEGF. However, there were positive reports of more partnerships between ophthalmologists and diabetologists and good models of district programmes that were being expanded to other districts. Botswana is the only country in the programme that currently has achieved a national screening programme.
Several learning points have emerged: It is important to have data collection and registries for organisation, planning and advocacy. Joint training of eye care and diabetes / NCD health workers has yielded many benefits and contributed towards programme staff having ‘ownership’ of their projects. Finally, patient empowerment and patient advocacy are important in ‘creating demand’ for services.
Summary of country progress
- Jamaica: excellent progress, increased equipment, treatment and awareness.
- Pacific: Fiji well established, Solomon Islands moving forwards, Vanuatu infrastructure set up.
- South and Central Africa: Model programmes developing well, moving to national programmes.
- East Africa: Focus on training centres and building up tertiary centres, beginning to expand to other districts.
- West Africa: Model programmes need to be implemented nationally – strengthening tertiary centres.
At the end of the workshop each LINKS institution had developed a two-year plan, each being different according to the local needs and priorities. In some situations there was a need for equipment, for example, a laser, in order to move forward with the programme. Other places were short of ophthalmologists or screener / graders. There were examples of advocacy resulting in resources being made available from ministries of health, LINKS or the World Diabetes Federation. On the same topic, delegates talked about trying to get an ‘ambassador’ in some form but it was not always clear what their role should be – creating awareness of diabetes and healthy eating, or advocating for eye care services with ministries of health. Countries where there has been good expansion of DR services demonstrated the importance of engaging with the MoH, the national eye care programme or with the NCD programme (or both).
One exciting development has been cooperation between diabetologists and the eye team. For the first time we heard evidence of patients being screened in the diabetes clinic. It has proved beneficial for patients and has enhanced the standing of diabetologists who have been able to offer a valuable service in their own clinics.
The need for better statistics was highlighted as this produces the evidence that is used for advocacy to acquire more resources – so there is a need for common management information systems – at least a common database system into which all members of the DR-NET can input their data.
At the conclusion of the meeting it was agreed to address some of the barriers to progress in the areas of equipment procurement, data sharing and training. Good quality low cost equipment can be sourced through the International Agency for the Prevention of Blindness (IAPB) ‘standard list’. It was resolved to improve the DR-NET website and create a forum for sharing knowledge and resources. The Commonwealth Eye Health Consortium (CEHC) fellowship programme can provide specialist training opportunities for ophthalmologists (medical retina) and technicians (equipment maintenance).
Conclusion
The DR-NET has proved an effective way of utilising VISION 2020 LINKS partnerships to share expertise and strategies and increase the provision of diabetic retinopathy services within the 12 countries. The programme has expanded to include Indonesia, Jamaica and the Pacific Islands, all places where the prevalence of diabetes is high. We look forward to further significant progress over the next two years of the DR-NET.
References
1. International Diabetes Federation. IDF Diabetes atlas. 7th Edition. 2015. International Diabetes Federation, Brussels.
http://www.idf.org/diabetesatlas/
Last accessed December 2016.
2. Yau JW, Rogers SL, Kawasaki R. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012;35(3):556-64.
3. VISION 2020 LINKS Diabetic Retinopathy Network Toolkit, 2016 available at:
https://www.dropbox.com/
s/xwl0kh0j1awyr6e/DR-NET%20
Toolkit%20-%202016%20all%20PDF.pdf?dl=0
Last accessed December 2016.
4. Stratton IM, Adler AI, Neil HA. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Br Med J 2000;321:405-12.
5. DR-NET
https://sites.google.com/site/drnetcomm/home
Last accessed December 2016.
COMMENTS ARE WELCOME