History
A 78-year-old female presented with bilateral, painless, progressive blurring of vision over five years, photophobia and increasing glare. Her past medical history included a known diagnosis of monoclonal gammopathy of undetermined significance (MGUS).
On examination, vision in the left eye was 6/36 and in the right 6/60. The cornea showed bilateral stromal opacities in irregular clusters mainly in the central to mid-peripheral posterior stroma. Anterior segment optical coherence tomography revealed band-like hyperreflective lesions in the posterior stoma / pre-Descemet’s membrane of both corneas.
The patient underwent a penetrating keratoplasty and the sample sent to the ophthalmic pathology department.

Figure 1a: H&E staining.
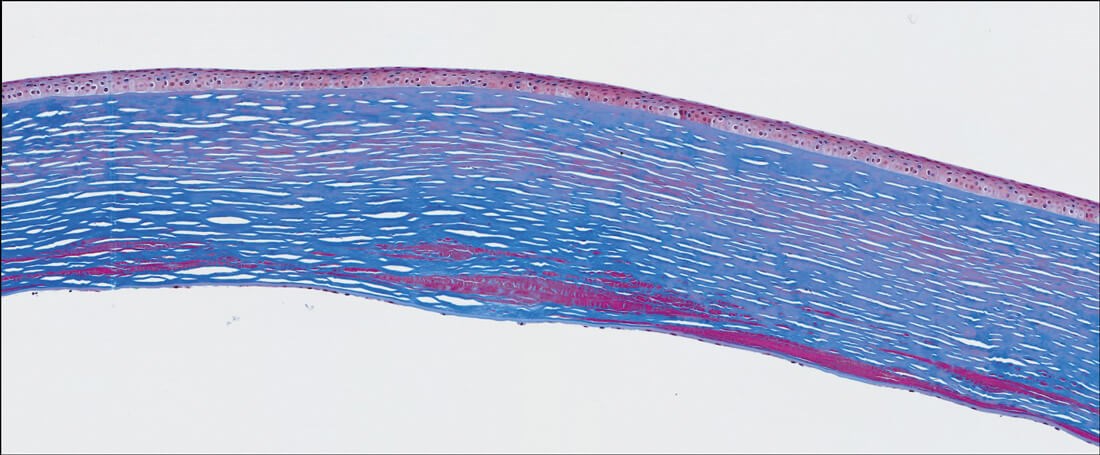
Figure 1b: Masson trichrome special stain.
Questions
- Figures 1 shows representative H+E (a) and Masson trichrome (b) stained sections of the corneal button. How can this be described?
- Considering the clinicopathological features, what is the diagnosis?
- What are the management options?
Answers
- Figures 1a and 1b demonstrate a penetrating keratoplasty with prominent posterior stromal and sub-Descemet’s membrane deposits of dense, amorphous and fusiform eosinophilic / red material, respectively. There is stromal oedema and scarring. Descemet’s membrane shows sparse endothelial cells. Immunohistochemistry for Kappa and Lambda were also performed (not shown). Kappa immunostaining was negative and unfortunately there were technical issues with Lambda immunostaining.
- The overall features are those of paraproteinemic keratopathy, secondary to the known clinical history of MGUS. Paraproteinemic keratopathy is a rare ocular disorder characterised by the accumulation of abnormal immunoglobulin proteins or paraproteins in the cornea. These paraproteins form deposits that appear as crystalline, nummular, patch- or lattice-like opacities in the corneal stroma, and can cause reduced / blurred vision, glare or photophobia. The condition is associated with systemic haematological diseases (monoclonal gammopathies / paraproteinemia) such as MGUS, multiple myeloma, or other plasma cell dyscrasias. Although rare in presentation, paraproteinemic keratopathy may be the first indication of an underlying potentially serious systemic disease and therefore warrants further investigation. It can often be misdiagnosed as a corneal dystrophy, crystalline keratopathy or scar lesion.
- Management includes systemic treatment for the underlying cause, which will likely involve haemato-oncology and a multidisciplinary approach. For clinically significant visual impairment, not responding to systemic treatment, options include phototherapeutic keratectomy, superficial keratectomy, deep anterior lamellar keratoplasty or penetrating keratoplasty (depending on depth of deposits), or keratoprosthesis. However, the paraproteinemic keratopathy can recur if blood paraprotein levels remain high.











