Held earlier this year, the 12th annual Moorfields International Glaucoma Symposium provided a forum for advanced clinical and scientific exchange in glaucoma management. The authors describe the key presentation themes and debates, highlighting specific topics of interest to glaucoma specialists.
The ocular surface
Professor Stephen Pflugfelder, Baylor College of Medicine, USA, and President of The Association for Research in Vision and Ophthalmology (ARVO), explored the science behind the symptoms of ocular surface disease (OSD). Unique features render the cornea sensitive to pain. Tear instability promotes corneal barrier disruption and nociceptor exposure, and dryness increases expression of neurosensitising inflammatory mediators.
There is an evolving understanding of cornea pain, which may become chronic and refractory to conventional therapy. Decreased nerve density with increased beading and tortuosity has been noted in eyes receiving preserved glaucoma treatments [1]. Initial therapy should be targeted to tear dysfunction if tear instability is present. Evidence suggests blood products promote corneal epithelial healing [2] and platelet rich plasma has been the most effective therapy in Professor Pflugfelder’s experience.
Reduced glaucoma-related quality of life (QoL) measures and benzalkonium chloride (BAK) exposure are predictive of OSD, the latter more common with increasing severity of glaucoma [3], explained Hari Jayaram. Ocular surface disease is important to glaucoma specialists because it leads to poor adherence with medications, is associated with a significant economic burden [4] and chronic conjunctival inflammation worsens surgical outcomes [5]. Reducing ocular surface inflammation improves trabeculectomy outcomes [6].

A cross-sectional study of glaucoma patients at Moorfields Eye Hospital (n=878) revealed a patient-reported prevalence (Ocular Surface Disease Index [OSDI]) of 58% (26% severe) (Table 1). Clinician-reported prevalence measures were 50% for tear break up time (TBUT) <10 seconds and 29% for abnormal Oxford Grading. Preliminary analyses suggest that increasing the number of drops is associated with worse OSDI scores and severity of blepharitis.
Dr Miriam Kolko, Copenhagen University Hospital, Denmark, explained that the physical properties of generic latanoprost ophthalmic solutions are not identical. Force requirements to extract drops, buffer capacity and pH values, viscosity (impacting corneal penetration), osmolarity and drop size vary significantly [7]. A review of available evidence found no clinically significant difference in intraocular pressure (IOP)-lowering effect or tolerability between generic prostaglandin analogues (PGAs) and the original formulation, but recommended further research to confirm equivalence [8].
Preservative-containing antiglaucomatous drops affect the viability and functions of conjunctival goblet cells, the latter essential for maintaining ocular surface homeostasis [9]. Prostaglandin analogues spare goblet cells more than other antiglaucoma drops and goblet cells may be a good predictor of surgical outcome after filtration surgery [9]. Preservatives cause and exacerbate OSD, reduce QoL, reduce adherence and reduce success of glaucoma surgery, added Dr Kolko.
Alex Shortt, Optegra Eye Health Care, emphasised the importance of managing OSD prior to glaucoma surgery. Two areas were emphasised: improving comfort and compliance (diverting some patients away from surgery) and improving outcomes of those who do have surgery (reduced surgical failure through scarring). Switching to preservative free glaucoma drops has been shown to reduce the need for lubricants [10], improve tear film quality [11,12] and improve IOP control in combined OSD and glaucoma [13]. Recommendations for breaking the OSD cycle pre / post-cataract or glaucoma surgery include: 1) remove preservatives; 2) new generation lubricants (sodium hyaluronate 0.1% to 0.3% and sodium hyaluronate plus trehalose; and 3) anti-inflammatory therapy using, for example, preservative free steroids, ciclosporine, essential fatty acids and doxycycline 100mg daily for four weeks (Figure 1).

Figure 1: Treatment algorithm: topical steroids are recommended at step 2 and step 4 in the TFOS DEWS II guidelines.
Source: Adapted from Jones L, et al. DEWS II Management and Therapy Report. Ocul Surf 2017;15(3):575-628.
Medical aspects of glaucoma
The art of using optical coherence tomography (OCT) in the real world is in systematic interpretation, emphasised David F Garway-Heath. Structure and function provide complementary information. It is important to maximise image quality during acquisition, assess images for segmentation errors and artifacts and systematically review the reports, in the context of other data. Clinicians also need to closely monitor for change.
Professor Tanuj Dada, RP Centre for Ophthalmic Sciences, India, shared study findings that meditation induces significant changes in trabecular meshwork (TM) gene expression in patients with primary open angle glaucoma (POAG) [14]. Results suggest that meditation can positively modulate cellular mechanisms involved in glaucoma pathogenesis by direct impact on ocular tissues [15].
Professor Pradeep Ramulu, Johns Hopkins Wilmer Eye Institute, USA, reviewed the impact of glaucoma on patients’ everyday activities, noting that the work of glaucoma specialists allows people to read, move about and remain active. It is critical to communicate these messages to stakeholders. Also, clinicians need to consider what they are doing about those who can’t be cured.
Professor Gary Holland, David Geffen School of Medicine at UCLA, USA, presented a uveitis specialist’s perspective on evaluation and treatment of uveitic glaucoma. Glaucoma / elevated IOP is a common complication of chronic anterior uveitis. The goal should be prevention of uveitic glaucoma by aggressive suppression of anterior segment inflammation. Corticosteroid treatment can contribute to control of elevated IOP in selected cases. The choice of medical or surgical treatments for elevated IOP in patients with uveitis may be different than in patients with age-related chronic open angle glaucoma. Close monitoring and follow-up is necessary, regardless of the treatment chosen, due to an increased risk of treatment failure. Table 2 summarises key considerations for managing uveitic glaucoma in children.

Trials and tribulations
Winnie Nolan noted the need for further randomised controlled trials (RCTs) of current medical treatments compared with surgery, particularly for people with severe glaucoma and in black ethnic groups. Glaucoma is the leading cause of irreversible visual loss and an increasing public health burden in Africa and Asia. Social deprivation is linked to glaucoma blindness. Glaucoma is treatable and blindness avoidable, but there is a need to optimise current care pathways. Further research is required into low-cost effective treatment and diagnosis in high-risk populations.
Professor Ramulu observed that there are many levels at which glaucoma outcomes can be assessed. For an interested young researcher there are multiple new opportunities, for example, to incorporate more detailed and more sensitive domain-specific outcomes into glaucoma treatment trials and develop measures to understand treatment success as a path, not a state [16].
Professor Gianni Virgili, University of Florence, Italy, discussed achievements and next steps in the Cochrane Eyes and Vision (CEV) collaboration. Cochrane Eyes and Vision has led 20 years of systematic reviewing, with more than 200 eyes and vision systematic reviews on the Cochrane Database of Systematic Reviews, at least half of which are up to date. But one quarter of reviews on important questions about common interventions contain no trials and many more are inconclusive. Intervention reviews and diagnostic test accuracy reviews on OCT are underway to support the ongoing update of the European Glaucoma Society guidelines. Further reviews of minimally invasive glaucoma surgery (MIGS) procedures for OAG as well as a review of non-contact methods for the detection of people at risk of primary angle closure glaucoma (PACG) are due this year.
Richard Wormald discussed ‘the long view’, explaining that the CEV collaboration has shown what can be achieved with proper analysis of synthesised evidence. He emphasised that reducing uncertainty is key. Priorities include: national survey of eye health and disease, linked to public awareness and access to services; how to identify the optic nerve at risk of pressure damage; core outcomes and better measures of function; key treatment trials focused on which treatments work best for which people especially those at greatest risk; user-friendly electronic patient records for artificial intelligence (AI) application; and glaucoma registers and Certificate of Visual Impairment data. Findings from the Treatment of Advanced Glaucoma Study (TAGS), expected soon, will shed new evidence on the optimal primary treatment for those presenting with advanced glaucoma and proper comparative effectiveness research evaluating MIGS devices will help fill evidence gaps.
DEBATE I: Trusty trabeculectomy or the new kid on the block
Pro: Trabeculectomy for me any day, argued Professor Dale Heuer, retired professor and Chair of Ophthalmology and Visual Sciences, Medical College of Wisconsin, USA, and past President of The American Glaucoma Society. Extensive literature, including long-term outcomes, supports tried-and-tested trabeculectomy. The preferred / consensus approach has been refined over decades of experience. New kids on the block are less invasive, less artisanal procedures and the initial postoperative course is more predictable. However, the cons are intraoperative conjunctival perforation, high needling rate and postoperative conjunctival erosion [17,18] and use conjunctiva superiorly. Moreover, MIGS techniques are still evolving, with limited short- / intermediate-term literature and no randomised studies vs. trabeculectomy.
Con: Microshunts for me, said Leon Au, Manchester Royal Eye Hospital. Trabeculectomy is good (in good hands), but it is an invasive procedure, time-consuming, difficult skill to master, involves delayed recovery and potential for complications. Modern glaucoma surgery requires less drops, earlier intervention to prevent damage, lower complication rates, shorter surgical time, easier surgery that is less skill dependent, universal results and better faster postoperative recovery. The microshunt postoperative regime involves no weekly visit to clinic, no bleb manipulation, lower risk of hypotony / leak, little postoperative restriction, generally minimal discomfort and the procedure combines well with phacoemulsification. A majority of glaucoma surgeons indicated they would prefer micro-invasive glaucoma surgery over traditional trabeculectomy or a glaucoma drainage device (GDD) as a primary glaucoma procedure [19].
DEBATE II: Oral supplements for glaucoma
Pro: Gimme all you got, I ain’t taking no chances, noted Professor Jonathan Crowston, Duke-NUS Medical School, Singapore National Eye Centre, Singapore. It is unreasonable to deny the use of supplements to certain POAG patients where conventional therapies are not sufficient and the lack of robust evidence does not mean something is not effective. While it is not known whether supplements do or do not alter the natural history of glaucoma [20], treating physicians should be able to guide patients to supplements with the best safety profiles and stronger biological plausibility. Supplements may not improve visual outcome in glaucoma but may offer hope and empower patients.
Con: I want the finest available evidence, here and now, argued Professor Virgili. Clinicians need translational research on oral supplements for glaucoma. Ongoing RCTs are evaluating the efficacy of citicoline eye drops in reducing progression of glaucoma, the effect of oral neurotidine® intake on QoL in patients with glaucoma and the antioxidant and neuroprotective effects of oral coenzyme Q10 (CoQ10) miniactives® in POAG patients. Rare side-effects also need consideration.
Cool science
Professor Crowston presented results of a recently completed prospective study of nicotinamide (NAM, amide of vitamin B3) supplementation in glaucoma. Photopic negative response (PhNR) improved after 12 weeks of NAM and a greater proportion had ≥1 dB improvement in visual field mean deviation (MD) on NAM compared with placebo. High-dose NAM can improve retinal function in a proportion (25%) of IOP-treated glaucoma patients and a larger study is being planned to determine whether short-term PhNR improvement predicts delayed progression with NAM.
Nicotinamide treatment is robustly protective in multiple models of glaucoma and clinical trials for NAM in glaucoma are underway, highlighting the importance of fully assessing NAM’s effect(s) on retinal ganglion cells (RGCs), noted Dr Pete Williams, Karolinska Institute, Sweden [21]. Nicotinamide has promising potential as a cost-effective, potent neuroprotective for glaucoma with limited side-effects and may be even more efficacious in combination with IOP-lowering strategies.
Dr Kate Keller, Casey Eye Institute, USA, reviewed TM cell culture and anterior segment organ culture, extracellular matrix modelling, targeting specific TM regions, TM cellular replacement and actin cytoskeleton. Cultured TM cells are a valuable model system to study the cellular mechanisms involved in the regulation of conventional outflow resistance and thus IOP and their dysfunction resulting in ocular hypertension [22]. Lasting restoration of IOP control through induced pluripotent stem cells (iPSC)-TM transplantation is possible and may represent a novel treatment approach for glaucoma [23]. Dr Keller also highlighted the significance of tunnelling nanotubes in the eye, which provide a direct mechanism of cellular communication that potentially may be used to deliver payloads of drugs or virus for example.
Findings examining the effect of ambient air pollution on glaucoma in UK Biobank participants were presented by Professor Paul Foster, on behalf of The UK Biobank Eye and Vision Consortium [24]. There was a significant association between higher current fine particulate matter (PM2.5) exposure and both a higher risk of self-reported glaucoma (6% higher odds) and thinner macular ganglion cell-inner plexiform layer (GC-IPL). The association appears independent of IOP. The effect of PM2.5 exposure on glaucoma is possibly mediated by a neurotoxic or vascular mechanism and further research is warranted into the effects of fine particulate air pollution on both RGC physiology and retinal vasculature.
Under the knife
Professor Heuer discussed the question of ‘new tubes for old’. Future aqueous shunt surgery challenges are achieving sufficiently low IOP [25], quickly and predictably, without supplemental ocular hypotensive medications, prevention of vision loss and minimising complications.
Professor Gus Gazzard explored the choice and timing of surgical glaucoma procedures, noting there is no zero-risk IOP control. There is a hierarchy of need and a hierarchy of risk, and it is question of balancing both. Risk and benefit both change over time, while benefits, harms and probability are perceived differently by different patients and doctors (e.g. confirmation bias). New devices, old tubes, new tools and techniques provide clinicians with a myriad of choices, but many lack supporting evidence from RCTs.
For PACG, the first-choice operation is early lens extraction. For POAG patients where selective laser trabeculoplasty (SLT) plus maximally tolerated medical therapy is insufficient, trabeculectomy for a sub-10mmHg IOP target is an appropriate option. Trabeculectomy with Mitomycin-C (MMC) achieved lower IOP with use of fewer glaucoma medications compared with tube shunt surgery after three years of follow-up in the Primary Tube Versus Trabeculectomy (PTVT) Study [26]. Microshunt implantation may be an option for high myope or uveitic patients. Other options, such as gonioscopy assisted transluminal trabeculotomy (GATT), Kahook, and ab interno canaloplasty, should only be considered as part of carefully monitored research with ethics approval for experimental procedures. “Finally, let’s always ask ourselves, what would we want if our grandmother had this?” concluded Professor Gazzard.
Leon Au highlighted the importance of achieving the right flow in glaucoma surgery. Case series data from Manchester demonstrate effective IOP lowering ‘down to Baerveldt (BVT) levels’ using the adjustable ‘fully titratable’ eyeWatch system. Successful retro eyeWatch rescue of refractory hypotony after BVT implantation has been reported [27].
Professor Dada observed the disparity between existing quality of evidence on effectiveness of MIGS and adoption by clinicians, with usage primarily governed by surgeon preference, training, experience and comfort. Sheheitli and colleagues argued that MIGS procedures are not likely to be effective if the surgical goal is a marked reduction in IOP or control of a very high IOP [28]. Gold standard glaucoma surgery is trabeculectomy with MMC, a high yield, high risk and high maintenance surgery shown to be cost-effective at a substantially lower cost per quality-adjusted life-years compared with tube insertion [29].
Paediatric ophthalmology in glaucoma
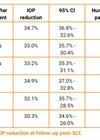
John Brookes, Moorfields Eye Hospital and Great Ormond Street Hospital for Children, explained that successful treatment of adults with childhood-onset glaucoma depends on their successful treatment in childhood and often requires more aggressive management due to the long-term nature of the disease and more advanced disc damage. Transition from goniotomy to 360° trabeculotomy for congenital glaucoma has revealed good outcomes through long-term follow-up, at Moorfields Eye Hospital. At 1 year follow-up (n=106 eyes), the rate of qualified success was 94.3% for trabeculotomy and 34.6% for goniotomy, with further surgery required in 7.4% and 63%, respectively. At final follow-up, qualified success was 85% for trabeculotomy vs. 37% for goniotomy.
Circumferential angle surgery approaches are likely being used more commonly in paediatric glaucoma, with very good to excellent outcomes, noted Professor Allen Beck, Redmond Professor and Chair, Emory University Department of Ophthalmology, USA [30]. Angle surgery of all types remains the treatment of choice for primary congenital glaucoma, with broader applications for other childhood and adult glaucomas. Conventional trabeculotomy combined with trabeculectomy (±MMC) offers potential for dual outflow; several studies have documented enhanced success of this procedure compared with goniotomy or trabeculotomy in countries where late presentation and familial cases are common.
Alessandra Martins reviewed paediatric trabeculectomies and tube shunt surgery. The aim of management, where possible, is to provide a lifetime of vision and surgery is the mainstay of treatment. Modern trabeculectomy can be an effective and safe procedure in infants, avoiding the complications of tubes. However, GDDs maintain a vital role for certain types of glaucoma including those refractory to other surgery.
References
1. Martone G, Frezzotti P, Tosi GM, et al. An in vivo confocal microscopy analysis of effects of topical antiglaucoma therapy with preservative on corneal innervation and morphology. Am J Ophthalmol 2009;147(4):725-35.
2. Soni NG, Jeng BH. Blood-derived topical therapy for ocular surface diseases. Br J Ophthalmol 2016;100(1):22-7.
3. Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol 2012;153(1):1-9.
4. Chan CC, Crowston JG, Tan R, et al. Burden of ocular surface disease in patients with glaucoma from Australia. Asia Pac J Ophthalmol (Phila) 2013;2(2):79-87.
5. Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol 1994;112(11):1446-54.
6. Breusegem C, Spielberg L, Van Ginderdeuren R, et al. Preoperative nonsteroidal anti-inflammatory drug or steroid and outcomes after trabeculectomy: a randomized controlled trial. Ophthalmology 2010;117(7):1324-30.
7. Kolko M, Koch Jensen P. The physical properties of generic latanoprost ophthalmic solutions are not identical. Acta Ophthalmol 2017;95(4):370-3.
8. Steensberg AT, Müllertz OO, Virgili G, et al. Evaluation of generic versus original prostaglandin analogues in the treatmentof glaucoma: a systematic review and meta-analysis. Ophthalmology Glaucoma 2020;3:51-9.
9. Tiedemann D, Mouhammad ZA, Utheim TP, et al. Conjunctival Goblet Cells, the Overlooked Cells in Glaucoma Treatment. J Glaucoma 2019;28(4):325-33.
10. Goldberg I, Graham SL, Crowston JG, et al. Clinical audit examining the impact of benzalkonium chloride-free anti-glaucoma medications on patients with symptoms of ocular surface disease. Clin Exp Ophthalmol 2015;43(3):214-20.
11. Kuppens EV, de Jong CA, Stolwijk TR, et al. Effect of timolol with and without preservative on the basal tearturnover in glaucoma. Br J Ophthalmol 1995;79(4):339-42.
12. de Jong C, Stolwijk T, Kuppens E, et al. Topical timolol with and without benzalkonium chloride: epithelial permeability and autofluorescence of the cornea in glaucoma. Graefes Arch Clin Exp Ophthalmol 1994;232(4):221-4.
13. Batra R, Tailor R, Mohamed S. Ocular surface disease exacerbated glaucoma: optimizing the ocular surface improves intraocular pressure control. J Glaucoma 2014;23(1):56-60.
14. Dada T, Bhai N, Gagrani M, et al. Meditation induces changes in trabecular meshwork gene expression in patients with primary open angle glaucoma. Presentation at the 2019 ARVO Annual Meeting, held in Vancouver, Canada, 28 April – 2 May 2019.
15. Dada T, Gagrani M. Mindfulness meditation can benefit glaucoma patients. J Curr Glaucoma Pract 2019;13(1):1-2.
16. Jones L, Garway-Heath DF, Azuara-Blanco A, et al; United Kingdom Glaucoma Treatment Study Investigators. Are patient self-reported outcome measures sensitive enough to be used as end points in clinical trials?: evidence from the United Kingdom Glaucoma Treatment Study. Ophthalmology 2019;126(5):682-9.
17. Arnould L, Theillac V, Moran S, et al. Recurrent exposure of XEN gel stent implant and conjunctival erosion. J Glaucoma 2019;28(3):e37-e40.
18. Arnljots TS, Economou MA. XEN Gel Stent exposure 7mo after primary implantation: a case report. Int J Ophthalmol 2019;12(4):689-91.
19. Chang TC, Vanner EA, Parrish RK 2nd. Glaucoma surgery preferences when the surgeon adopts the role of the patient. Eye (Lond). 2019;33(10):1577-1583.
20. Loskutova E, O’Brien C, Loskutov I, Loughman J. Nutritional supplementation in the treatment of glaucoma: A systematic review. Surv Ophthalmol 2019;64(2):195-216.
21. Nzoughet JK, de la Barca JM, Guehlouz K, et al. Nicotinamide deficiency in primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2019;60(7):2509-14.
22. Keller KE, Bhattacharya SK, Borrás T, et al. Consensus recommendations for trabecular meshwork cell isolation, characterization and culture. Exp Eye Res 2018;171:164-73.
23. Zhu W, Gramlich OW, Laboissonniere L, et al. Transplantation of iPSC-derived TM cells rescues glaucoma phenotypes in vivo. Proc Natl Acad Sci USA 2016;113(25):E3492-500.
24. Chua SYL, Khawaja AP, Morgan J, et al; UK Biobank Eye and Vision Consortium. The Relationship Between Ambient Atmospheric Fine Particulate Matter (PM2.5) and Glaucoma in a Large Community Cohort. Invest Ophthalmol Vis Sci 2019;60(14):4915-23.
25. Jung KI, Woo JE, Park CK. Effects of aqueous suppressants and prostaglandin analogues on early wound healing after glaucoma implant surgery. Sci Rep 2019;9(1):5251.
26. Gedde SJ, Feuer WJ, Lim KS, et al; Primary Tube Versus Trabeculectomy Study Group. Treatment outcomes in the Primary Tube Versus Trabeculectomy (PTVT) study after 3 years of follow-up. Ophthalmology 2020;127(3):333-45.
27. Elahi S, Bravetti GE, Gillmann K, et al. EyeWatch rescue of refractory hypotony after Baerveldt drainage device implantation: description of a new technique. J Glaucoma 2020;29(2):e7-e10.
28. Sheheitli H, Tirpack AR, Parrish RK 2nd. Which patients would most likely to benefit: MIGS or MEGS, which one is it? Asia Pac J Ophthalmol (Phila) 2019;8(6):436-40.
29. Kaplan RI, De Moraes CG, Cioffi GA, et al. Comparative cost-effectiveness of the Baerveldt implant, trabeculectomy with mitomycin, and medical treatment. JAMA Ophthalmol 2015;133(5):560-7.
30. Neustein RF, Beck AD. Circumferential trabeculotomy versus conventional angle surgery: comparing long-term surgical success and clinical outcomes in children with primary congenital glaucoma. Am J Ophthalmol 2017;183:17-24.
Declaration of competing interests: KB has received grants from AMO, New World Medical, Alcon, Merck, Allergan, Refocus; has participated on advisory boards for Alcon, Merck, Refocus, Ivantis, Kowa, Glaukos, Amakem, pH Pharma, EyeD Pharma and Laboratoires Thea; has received honoraria for lecturing from Allergan, Alcon, and Pfizer; has been a consultant for Alcon, Aquesys, Ivantis, Refocus, Carl Zeiss Meditec, Kowa, Santen, Radiance Therapeutics and Transcend Medical; and has stock in Aquesys, Vision Futures Ltd, London Claremont Clinic Ltd, Vision Medical Events Ltd and International Glaucoma Surgery Registry Ltd. KB also has had a patent issued related to Advanced Ophthalmic Innovations.
GG has received grants from Lumenis, Ellex, Ivantis and Thea; and personal fees from Allergan, Alcon, Glaukos, Santen, and Thea.
HJ declared consultant / advisory role with Allergan and honoraria from Santen, Allergan and Laboratoires Thea.
Acknowledgements: The 12th Moorfields International Glaucoma Symposium was supported by an educational grant from Thea Pharmaceuticals. Symposium chairs Keith Barton, Gus Gazzard and Hari Jayaram reviewed an initial draft manuscript summarising presentations and debates and approved the final article for journal submission. Medical writing support was provided by Rod McNeil Associates and was funded by Thea Pharmaceuticals. E: info@migs.org.uk
COMMENTS ARE WELCOME