Recently, there has been an interesting development in medical education and its ‘gamification’. Educators are constantly looking for new ways to engage their students by adding a friendly element of competition, as evidenced by the great success of online education games such as Kahoot.
Taking this further, some establishments have started to make use of the escape room as a form of teaching, team building and even assessment [1]. There were, however, no operating escape rooms in ophthalmology undergraduate teaching, until we made one.
Escape rooms have been in the public eye for many years. Wide reception of the premise was met when television shows such as The Crystal Maze became popular. A team of 10 would encounter various rooms which each held an obscure challenge. Those who completed the challenges were offered the chance to win cash prizes, whereas those who did not were locked away and left as their team continued. The latter, of course, is a little harsh for medical undergraduates!
Since the popular television show, there have been a great number of escape room experiences in the UK, each with multiple rooms and themes, and some even making use of virtual reality software. They are a great way to socialise, excellent for team building and generally good fun all around.
At some point though – it is not clear exactly when – the escape room package was translated to medical education and has since been shown to be an effective way of engaging students, and even assessing them. Looking at the wider field of view, the escape room premise is also being used in recruitment and human factors training [2,3]. Readers may be familiar with the premise of an escape room, but for those who aren’t, here’s a short summary.
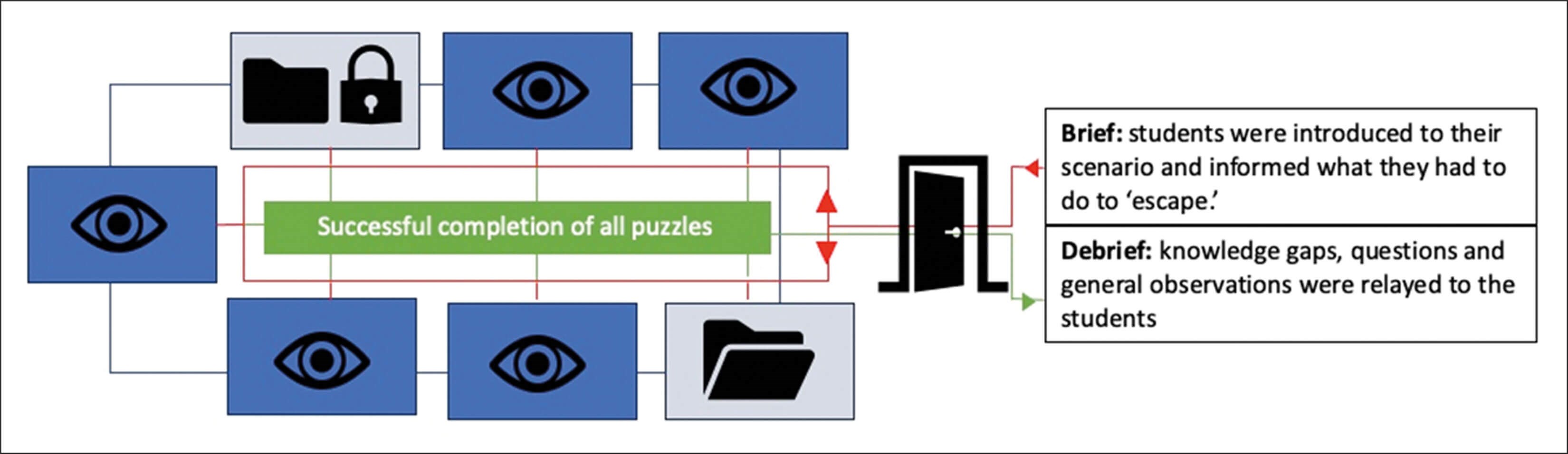
Figure 1: Diagram representing the ophthalmology escape room idea. Students are briefed and enter the room. Puzzles can be addressed in any order (indicated by red arrows and line), and all puzzles are linked to each other (represented by the blue line). Completion of each puzzle generates an answer, all of which are needed to ‘escape the room’. Students are then debriefed.
The experiences often start with a cryptic introduction over some form of audio-visual software which introduces the room and more importantly, how you get out of it once the doors close and you’re ‘locked’ in. Traditionally, these games make use of logic puzzles, very basic mathematics, play on words and a time limit designed to induce some form of pace to the game. Put them together and you have four or five people working together in ways that are incredibly interesting to watch, all with the aim of escaping the room and declaring themselves the winner! Now consider translating this to ophthalmology.
A quick literature search on PubMed reveals their popularity in the USA, mainly in emergency medicine [4,5]. In the UK, rooms have been designed for medical undergraduates in emergency medicine, elderly care and dermatology [2], and likely more that have not made it to publication / wider awareness yet. These rooms have been tried and tested on medical students, junior doctors, ranging from foundation year to senior registrar, and even management as a form of team building. Feedback in all publications showed a positive response from users to areas such as team building, knowledge consolidation and awareness of protocols. At the time of writing, there were no obvious publications on escape rooms in ophthalmology.
This presented an opportunity to design and create an ophthalmology escape room experience for medical undergraduates, making use of common ocular exams and presentations to emergency departments / inpatient encounters. Designing the room took a couple of hours, with integration taking a similar amount of time. The most difficult part of the design process was ensuring each puzzle had one outcome and that the puzzles could be approached in any order. After several test runs on colleagues, the room was ready.
On the teaching day, students were given material to read prior to attending, and the first few hours utilised a reverse classroom model to lay the foundations of the eye, core conditions and management, and practical examinations. They were told at the start of the day that there would be a very informal way of checking how much they’d taken on during the day. After many breaks and a long lunch, we returned and introduced the escape room as a form of knowledge consolidation and more importantly, a fun and new way to end a day of learning.
The games and puzzles were designed in such a way that each provided a code or clue to another. Students, once in the room, were able to start at any game and it would work out so that only one outcome could be reached. Successfully reaching the outcome ‘unlocked’ the room. To make it less clinical and more whimsical, a story was added to the pre-game brief. Students were told they were double agents on the run from The Consultancy. Their identities had been revealed and Consultancy Agents were rapidly closing in. Their daring escape hinged on finding a USB drive hidden in a 5-digit locked device. A series of games relating to their training awaited them. Consultancy Agents were only 20 minutes away. Finally, I added some copyright-free spy music and away we went.
So, the premise was set. Then, the students had the games to conquer. As mentioned, games could be approached in any order and would always lead to the final 5-digit code. On entering the room, students were met with five games spaced around the room, as well as a padlocked box and padlocked folder, each requiring a number code to open and an unlocked folder with further information inside. The games were as follows:
- Core conditions. A series of riddles were created which were all related to ophthalmic conditions and their workup. For example, “Aliens take me, and I’ll do the same. Name my innervation to continue your game.” Students utilised lateral thinking (aliens take me = abduction) and taught knowledge (abduction = lateral rectus = LR6 SO4 A03 = CN6 Abducens). Another example: “You test my vision without my aids. You ask me to read and it’s all in vain. Reduce peripheral light to help me see. With this tool a diagnosis you seek.’” Answer: pin hole. The unlocked folder in the room had a document in it with a list of ocular conditions, devices and anatomical terms on them, each with a number next to them. Students work their way through the seven riddles and therefore generate seven numbers which are used later in the room.
- Practical examinations. Students saw a handover document from the on-call doctor, next to a model eye. It explained certain parts of an eye examination which have been done for a contact lens wearer who presents with a painful red eye. Unfortunately, key parts of the exam were missed but not highlighted. Students needed to identify that a visual acuity had not been performed, and that the cornea had not been viewed under cobalt blue. On the wall was a Snellen chart with line 6/12 highlighted in green. This was a 4-digit code. Depending on staff levels, at this point any examination could be performed on a facilitator who would remain silent unless the exam was performed to an OSCE pass standard.
The code opened the padlocked box and granted access to a direct ophthalmoscope, a smaller locked box requiring a 4-digit colour code, and a folder containing five distorted images, each numbered. Students were now able to view the model eye with the cobalt blue filter. They saw another 4-digit code on the model cornea which was invisible under normal light. - Visual fields. On a wall, students saw three diagrams of the visual pathway labelled 1, 2 and 3, each with a single black line somewhere in the pathway. These represented visual field defects. The diagrams related back to the images found in puzzle two. Two of the five images were distractors and did not correspond to the diagrams. The correct identification and organisation of the corresponding photos would reveal a 3-digit code. This 3-digit code opened the padlock on the folder which was visible when the students entered the room. Within the folder was a series of red or green numbered cards with ophthalmic conditions, investigations and management plans on them. There was also a series of 5x5 printed square grids containing numbers and letters, and four of the squares on each grid were coloured. A simple instruction accompanied them: “Arrange 4 by 5.”
- Diagnosis and management. The cards from puzzle four needed to be arranged four by five. Students knew which order was correct as each card read into the next below it. For example, card one would read “AACG is”; card two would describe AACG; card three would list the investigations; and card four would explain the management. It is imperative that the creator of the room leaves no ambiguity. Completion of all the columns showed several cards with a red background and one in each column with a green background. All cards were numbered. Students needed to realise the green card numbers from left to right are the code for the 5-digit lock found in game five.
- Logic (none were ophthalmology related). This game was designed to promote the team building aspect of the room. The outcome of game one, if completed, generated seven numbers. Students had now discovered a series of grids with numbers in each square. Identifying the correct numbers from the core condition game to the grid with the corresponding numbers was key. This correct grid had four numbers highlighted to match the colours of the padlock from game three. Unlocking the colour-coded padlock revealed the USB stick which had a 5-digit lock. The code to the 5-digit lock was derived from successful completion of game four.
Of course, not all students will have the same level of knowledge, enthusiasm or confidence. Therefore, a ‘clue’ must be available on demand, in case players go off on tangents. To keep this cost free, I simply stayed in the room as an observer and asked the players to knock twice on any surface for a hint to be given. This was also included to offer students the opportunity to ‘ask for help’ if stuck, which is a key skill as a junior doctor. This method allows the observer to cater clues to the gameplay and the level of difficulty of the clue after having observed players. Having a facilitator in the room also makes the debrief more informative as they have been able to observe the students.
The feedback for this project was very promising. A total of 20 students, in groups of four, volunteered and completed the room. The fastest escape was 14 minutes and the longest took 31 minutes. Students were debriefed and any knowledge gaps were addressed. The debrief allowed any problems with the game to be ironed out, and the next room could be adjusted.One hundred percent of students stated the experience helped to consolidate knowledge and reinforce teaching from the morning taught session. Moving forward, the room has already been replicated to include ENT and dermatology-related puzzles, with an updated run time of 45 minutes and successfully tested on 16 students. At the time of writing, the project was being modified for orthoptic students at the University of Sheffield. Specifically related to ophthalmology, the project hopes to make use of high-fidelity simulation such as EyeSi and increase its demographic to include trainee ophthalmologists.
References
1. Akatsu H, Shiima Y, Gomi H, et al. Teaching “medical interview and physical examination” from the very beginning of medical school and using “escape rooms” during the final assessment: achievements and educational impact in Japan. BMC Med Edu 2022;22(1):1–9.
2. Guckian J, Sridhar A, Meggitt SJ. Exploring the perspectives of dermatology undergraduates with an escape room game. Clin Exp Dermatol 2020;45(2):153–8.
3. Backhouse A, Malik M. Escape into patient safety: bringing human factors to life for medical students. BMJ Open Qual 2019;8(1):e000548.
4. Gue S, Ray J, Ganti L. Gamification of graduate medical education in an emergency medicine residency program. Int J Emerg Med 2022;15(1):1–7.
5. Cantwell C, Saadat S, Sakaria S, et al. Escape box and puzzle design as educational methods for engagement and satisfaction of medical student learners in emergency medicine: survey study. BMC Med Edu 2022;22(1):518.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME










