The authors ask whether e-learning can help to address the current lack of ophthalmology teaching in the undergraduate curriculum.
Studies among the United Kingdom, Australasian, Canadian and Asian medical schools have found that students on average spent just over a week in ophthalmology teaching. This number was considerably less in some medical schools who only provided two to three days of ophthalmic education. Based on a five-year course, this equates to around 0.2% of the entire undergraduate curriculum. With the COVID-19 pandemic, ophthalmology teaching has been further impacted, with other specialties being prioritised.
This is concerning given the rise in ophthalmic problems on a background of the ageing population. It is imperative for junior doctors to have a strong knowledge base of common ophthalmic problems, given these may be encountered in various settings across both primary and secondary care. With the increased use and reliance on digital resources due to COVID-19, one approach to increasing the amount of ophthalmic education is through utilising e-learning. We established ‘EyeEd’, an online webinar series, to deliver teaching on common ophthalmology topics.
The aim of this series was to identify gaps in the medical undergraduate curriculum, to provide a basic knowledge base for medical students and junior doctors, and to assess the effectiveness of such webinars in fulfilling their educational needs.
Methods
The EyeEd webinar series ran from August 2020 to October 2020. This comprised of nine sessions, each being at least one hour in duration. All webinars were conducted using the Zoom platform. The series covered ophthalmology history taking, eye infections, red eye, loss of vision, getting into ophthalmology training, diabetic retinopathy, glaucoma, age-related macular degeneration and neuro-ophthalmology. These sessions were led by ophthalmology specialty trainees.
Prior to the commencement of the webinar series, a baseline questionnaire was sent out for completion to all attendees, which captured data relating to demographics and ophthalmology teaching in their respective medical schools. After each webinar, attendees were asked to complete a questionnaire pertaining to feedback about the session. Statistical analyses were carried out using Microsoft Excel.
Results
The webinar series was attended by at least 133 unique medical students and junior doctors nationally (n=119) and internationally (n=14). The largest number of national students were from the University of Birmingham (n=22). Among the attendees, 71% were female and the median age was 23 years. Nearly half of the attendees (45%) were interested in pursuing ophthalmology as a career.
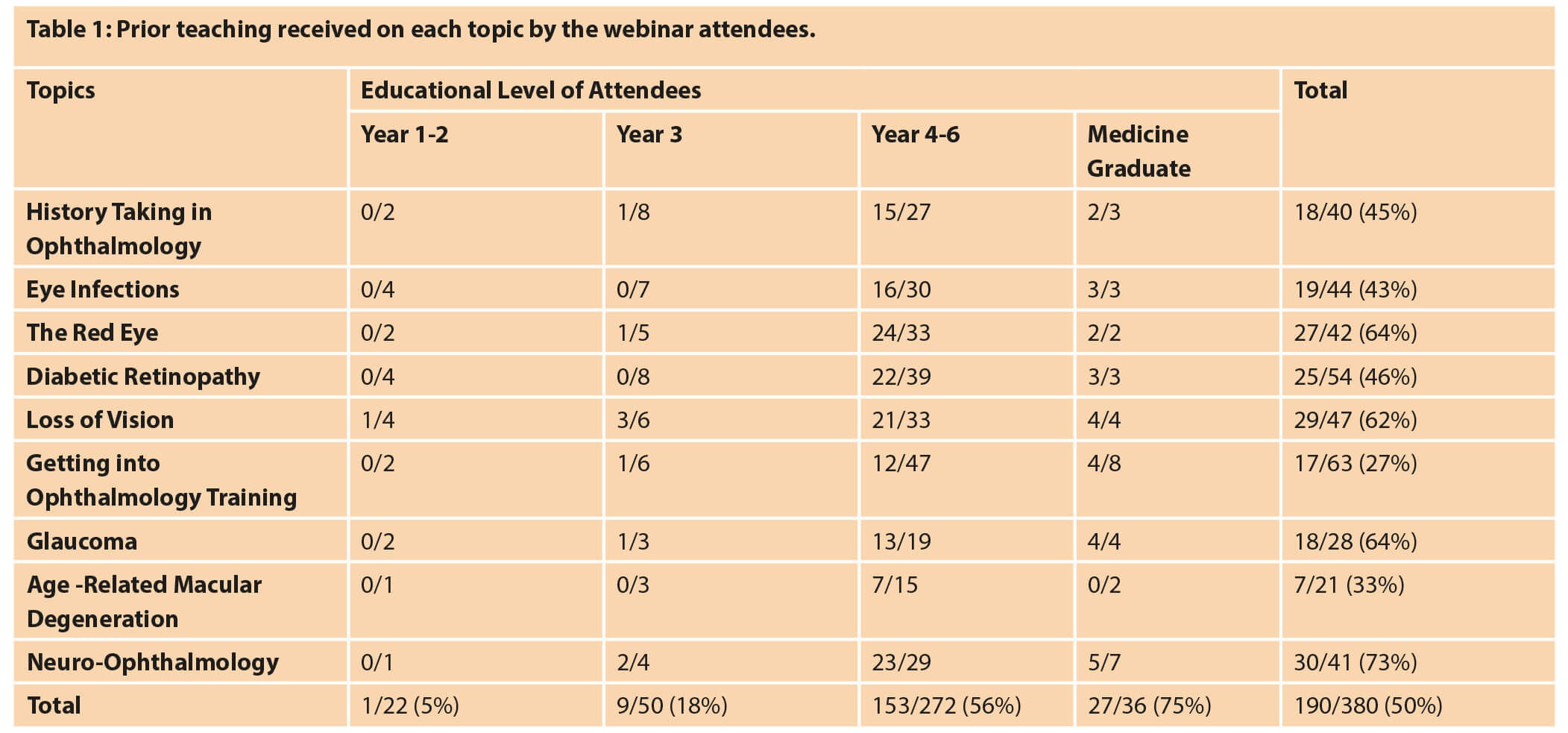
With regards to ophthalmology education in medical school, 11% of respondents agreed that the level of teaching was adequate. Table 1 details any prior teaching received by attendees for each session. Neuro-ophthalmology (73%), glaucoma (64%), the red eye (64%) and loss of vision (62%) had a high proportion of candidates who had been taught previously on the subject. In contrast, getting into ophthalmology training (27%) and age-related macular degeneration (33%) had the lowest number.

Figure 1: Evaluation of post-attendance feedback by individuals for each session.
Figure 1 illustrates the attendees’ feedback for each session. Overall, between 83% and 100% of individuals had an increase in knowledge from attending the e-learning sessions. Moreover, between 95% and 100% recommended the online webinar series depending on the session attended.
Conclusions
Less than a tenth of the attendees thought that ophthalmology teaching provided in medical school was sufficient. This is a worrying number given that junior doctors will almost certainly encounter patients with eye complaints during their training years. Moreover, some areas of ophthalmology are not being covered as well as others in the undergraduate curriculum. Despite this, medical schools may find it difficult to include more ophthalmology content given the oversaturation of the medical curriculum. One way to increase ophthalmology undergraduate teaching is through utilising e-learning.
“Less than a tenth of the attendees thought that ophthalmology teaching provided in medical school was sufficient”
We held a comprehensive ophthalmology webinar series covering various areas relevant to the undergraduate curriculum and foundation training. There were a high proportion of individuals who had a gain in knowledge after attending the online sessions and almost all who would recommend the webinar to others. Such a course, if implemented nationally as part of the undergraduate curriculum, will allow ophthalmology education to be standardised nationwide and ensure that all graduating medical students have a basic knowledge base. It also has the added advantage that students will be able use this as a resource in their own time. While it is understood that this method of learning would not allow for practical learning, it would ensure a good theoretical knowledge base for individuals to apply in clinical practice. Hence, e-learning should be considered as a useful aid to educating future doctors on areas that are underrepresented in the undergraduate curriculum such as ophthalmology.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME







