
Dr Alexander Strother reflects on his time designing and delivering a classroom-based programme to ensure that medical students know how to take comprehensive ophthalmic histories from patients.
Working as a clinical teaching fellow, in 2021 I had the great privilege of being invited to design and deliver a weekly teaching programme to all of University of Leeds’ third-year undergraduate medical students rotating through Leeds Teaching Hospitals Trust (LTHT) for the 2021/2022 academic year.
After recently handing over this teaching to the new ophthalmology junior doctors, I have since been reflecting on my experiences in the hope of informing my future ophthalmology teaching practice. I hope some of these reflections and the lessons I have learned along the way may prove helpful for others delivering or designing similar sessions.
Background
At Leeds Medical School, all third-year students complete a one-week ophthalmology placement. Previously central to this experience, for those rotating through LTHT, had been a busy afternoon in eye casualty focusing on history-taking. However, due to the ophthalmology registrars now being required to attend mandatory training at this time, it became necessary to instead design a classroom-based session that would retain this crucial history-taking focus.
Session Outline
The new two-hour session would consist of three parts. Part one saw the students and I spend 20 minutes outlining a history-taking structure and the key questions that are particularly relevant to an ophthalmic history. With many students familiar with the SOCRATES acronym and other similar structures by year three, our discussion instead largely revolved around ‘positive’ and ‘negative’ visual associated symptoms, while also encouraging them to remember to ask about contact lens use, previous surgeries, and driving, for example.
“I was keen to ensure this teaching was as undaunting as possible.”
Part two lasted for 30 minutes and saw us generate differential diagnoses for the presenting complaints of (a) red eye, (b) acute loss of vision, and (c) chronic loss of vision. When listing their differentials, students were challenged to state the main features of each condition at a year-three level. Though pathophysiology and management were often briefly explored, the primary focus was always firmly clinical; primarily, learners are encouraged to recognise which signs or symptoms make a particular diagnosis more or less likely. Below are images of work produced by the students during this part of our final session:
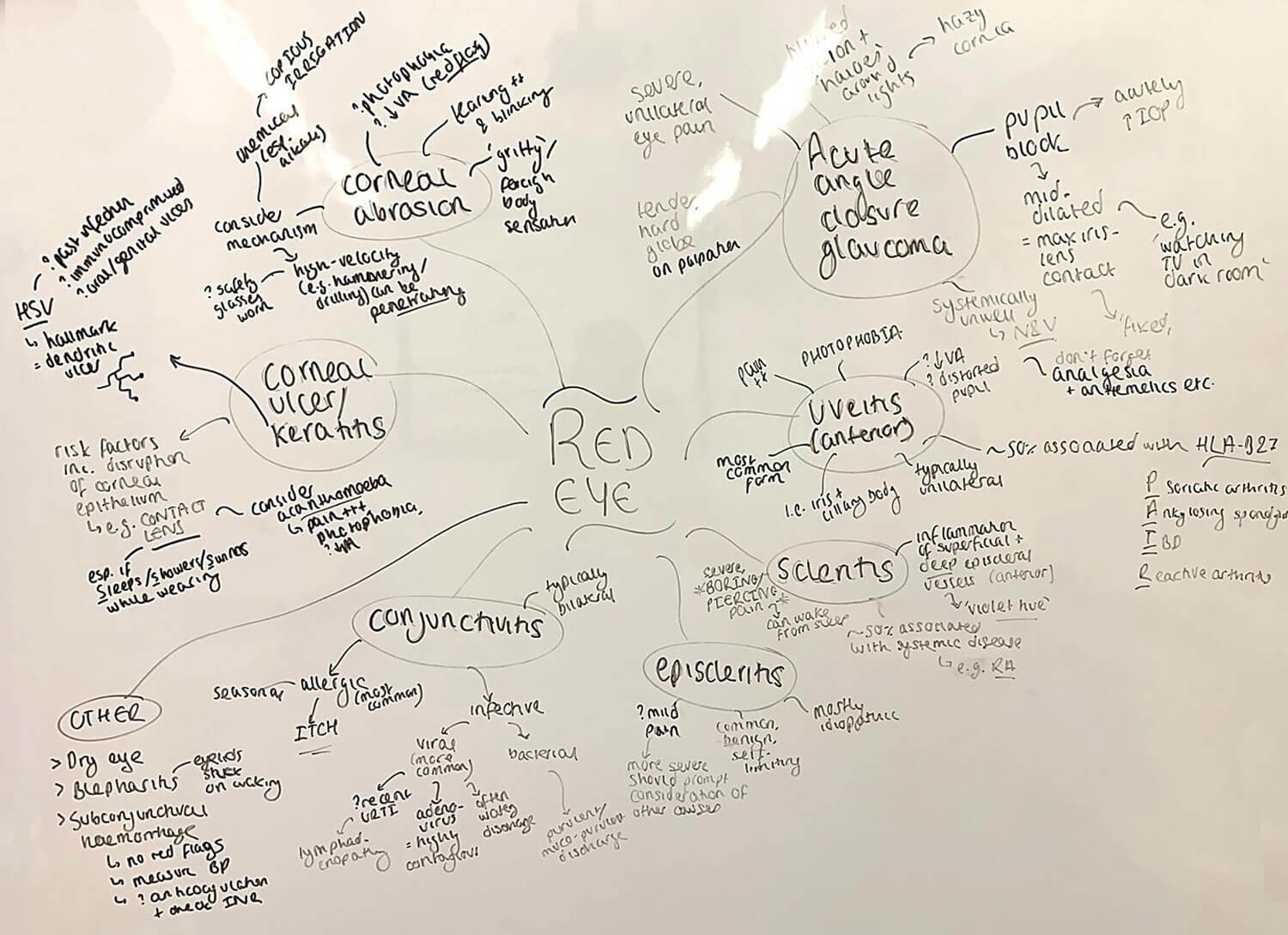
Differential diagnoses for red eye.
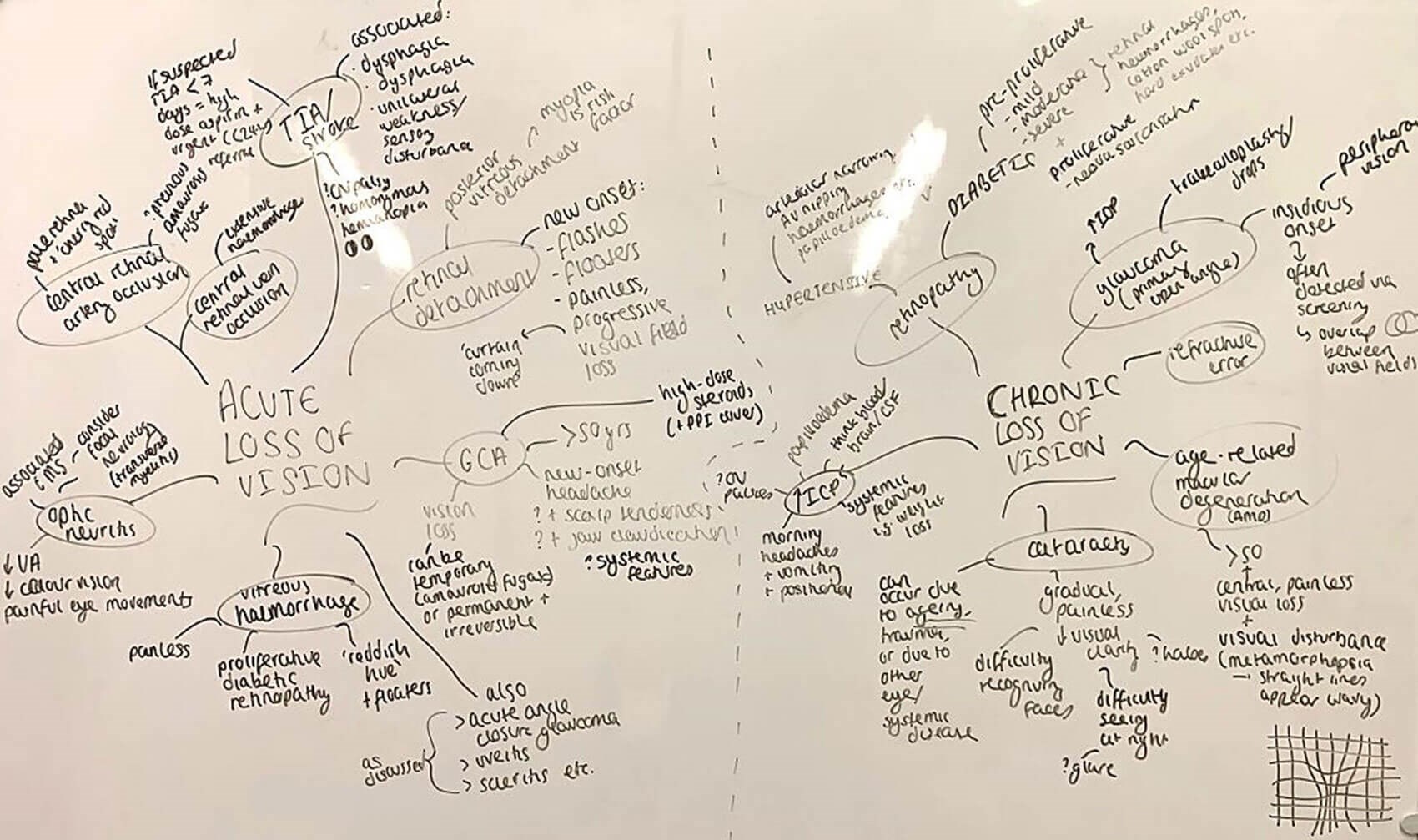
Differential diagnoses for acute and chronic loss of vision.
Finally, after a short break, students returned for part three. Centred on the principle of assessment for learning, the final 50 minutes allowed students the opportunity to immediately put into practice everything they had learned by completing a Mock Objective Structured Clinical Examination (MOSCE). Here, students worked in pairs and alternated between the roles of the candidate and patient / examiner. The MOSCE involved three stations, each with prior reading time for candidates and patients to study their briefs. All timings mirrored those of the students’ end-of-year summative examinations.
The first two stations instructed learners to take a comprehensive history from patients presenting with a painful, red eye and acute loss of vision, respectively. The briefs corresponded to ‘textbook’ cases of acute angle closure glaucoma and retinal detachment; both are underlined as ‘core conditions’ in the students’ year-three study guide. The third station focused on prescribing and was introduced in response to feedback after the first session; opportunities for students to practice can be scarce in the clinical environment. After being presented with a clinical vignette, students were asked to define the most likely diagnosis – in this case, orbital cellulitis, another emergency in their ‘core conditions’ list – before prescribing in pairs on laminated prescription charts according to LTHT guidelines.
During the stations, I rotated around the room and listened to each student, making notes for feedback. After each case, students were given six minutes to discuss the mark scheme and provide feedback. Finally, before moving on, I briefly discussed any points relevant to each candidate that hadn’t yet been remarked upon.
Reflections
Reviewing the wealth of anonymous feedback, the students were incredibly kind with their comments. With an average engagement score of 9.9/10, it is clear students appreciated the range of opportunities to get involved in each of the sessions’ three main elements. While nothing can ever truly replicate the invaluable experience of taking histories first-hand from patients in the clinical environment, the learners nevertheless relished the chance to develop and practice their history-taking skills. Expanding on this further, I would like to discuss what I believe to be two key themes behind why I think the session went well, and one area that offers definite scope for improvement going forward.
The first of the former is the concept of curriculum mapping and blueprinting. Ophthalmology can be daunting for medical students and an increasing number now graduate lacking confidence in their ophthalmic skills and knowledge [7]. This was repeatedly highlighted to me by informal discussions with the students – while many were familiar with common conditions such as hypertension and had practised taking histories on chest pain in the early years of their training, conditions such as uveitis and macular degeneration were entirely alien to them. I was keen to ensure this teaching was as undaunting as possible. By closely studying the third-year study guide and its list of core conditions, I ensured all discussions, cases, and more crucially, assessments were appropriately targeted to their level.
On a similar theme, the use of assessment for learning (i.e., formative assessment) proved a huge success in this teaching. MOSCEs offer a convenient, evidence-based means to employ the above and are specifically mentioned in Chadha and Gooding’s Twelve tips for teaching ophthalmology in the undergraduate curriculum [3]. Looking more broadly at the literature, reassuringly, students appear to learn not only through adopting the role of the doctor but also as the patient or examiner [2,6]. Furthermore, another point often raised is the importance of simulating summative assessment – through strict timings, use of genuine trust guidelines, and the writing of realistic stations and mark schemes, I was determined to provide an authentic learning experience [4].
“I have since been reflecting on my experiences in the hope of informing my future ophthalmology teaching practice.”
Conversely, one concept which I believe might enhance this teaching is the “flipped classroom” (FC). Indeed, this model has received particular attention in Scantling-Birch’s recent review of the current state of UK undergraduate ophthalmology teaching [7]. Here, as opposed to students first being exposed to content during the session, the FC allows part of this exposure to take place before the session, for example via well-prepared resources such as online handouts or lectures. This in turn frees up limited classroom time to focus on deeper learning, with learners applying their new-found knowledge to more challenging endeavours in a collaborative environment [6]. Considering Bloom’s taxonomy, this equates to more time addressing the higher cognitive domains, notably application, analysis, evaluation, and synthesis [1]. Theory aside however, in the case of this session, the FC would enable students to learn how to take an ophthalmic history in their own time and at their own pace. Relatively straightforward example MOSCE stations could even be provided beforehand, allowing the classroom-based teaching to instead include a greater number of stations focused upon more challenging concepts.
Conclusion
Overall, this experience was one of the most enjoyable and rewarding of my teaching career. While I of course appreciate that many of these reflections may not have direct application to much of the excellent ad-hoc teaching delivered by ophthalmologists in the clinical environment, I hope that some of the broader concepts touched upon, including the importance of learner-centred education, assessment for learning, awareness of the student curriculum, and the FC may be helpful for all. The outstanding teaching I received and the brilliant people I met in my one week ophthalmology placement as a third-year University of Leeds medical student inspired me to one day become an ophthalmologist, and I hope to play my part in teaching and inspiring the next generation.
References
1. Bloom BS. Taxonomy of Educational Objectives, Handbook I: The Cognitive Domain. New York, USA; David McKay; 1956.
2. Burgess A, Clark T, Chapman R, Mellis C. Medical student experience as simulated patients in the OSCE. The Clinical Teacher 2013;10(4):246-50.
3. Chadha, N, Gooding H. Twelve tips for teaching ophthalmology in the undergraduate curriculum. Medical Teacher 2020;43(1):80-85.
4. Gilani S, Pankhania K, Aruketty M, et al. Twelve tips to organise a mock OSCE. Medical Teacher 2021;44(1):26-31.
5. Lee C, Madrazo L, Khan U, et al. A student-initiated objective structured clinical examination as a sustainable cost-effective learning experience. Medical Education Online 2018;23(1):1440111.
6. Ramnanan C, Pound L. Advances in medical education and practice: student perceptions of the flipped classroom. Advances in Medical Education and Practice 2017;8:63-73.
7. Scantling-Birch Y, et al. Is undergraduate ophthalmology teaching in the United Kingdom still fit for purpose? Eye (Nature) 2021;36(2):343-345.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






