Click here for Part 2 on this topic, and here for Part 3
The Arclight Project is a mix of frugal design, manufacturing, distribution, teaching, research, and advocacy, all wrapped up in a social enterprise based at the University of St Andrews. The project is driven by the high burden of needless blindness (as well as deafness) in the poorer regions of the world, where access to training and diagnostic tools is least.
In low- and middle-income countries (LMICs) traditional instruments such as ophthalmoscopes are impractically expensive and often needlessly complex. Few hospital-based health workers have access to them and almost none at the mid or community level. A broken bulb or flat battery often consigns devices to the ‘graveyard’ bottom drawer – the Arclight was consequently designed to be robust and to not need ongoing consumables or servicing. It is unique in being the only truly portable and solar-powered ophthalmoscope, otoscope and loupe in the world. Clever modern frugal engineering brings a highly effective tool to the masses at low cost (Figure 1).

Figure 1: The highly portable Arclight device – an affordable yet effective replacement for traditional tools.
With the initial support of John Sandford-Smith, Sandy Holt-Wilson and Richard Le Mesurier, funding was secured from the Fred Hollows Foundation for William J Williams to create the first version of the Arclight (Figure 2). The project has now expanded to encompass a range of frugal low-cost training and diagnostic tools as well as teaching materials including a binocular indirect ophthalmoscope (BIO), simulation eyes, videos and mobile apps, all designed to strengthen eye and ear healthcare.

Figure 2: Evolution of the Arclight device.
Implementation of the package can help those working in primary care health centres, district hospitals and tertiary referral centres to deliver primary eyecare as well as comprehensive examinations to confidently diagnose and decide on the management of eye (and ear) disease. For these reasons we are not an eyecare service provider ourselves, but instead facilitate those already delivering services and training such as non-governmental organisations (NGOs), governments, and educational institutions.
Frugal engineering
Frugal engineering underpins our approach, which advocates for simplicity and economy, echoing the ‘less is more’ philosophy. William of Ockham’s [1] principle that simplicity often yields the best solution is not always instinctive; instead, designers often trend towards complexity in problem-solving. Yet, the merits of frugality are evident in many widely adopted interventions in resource poor settings, where necessity is the mother of invention. Our approach, embracing this necessity with clear focus, can spark innovative solutions.
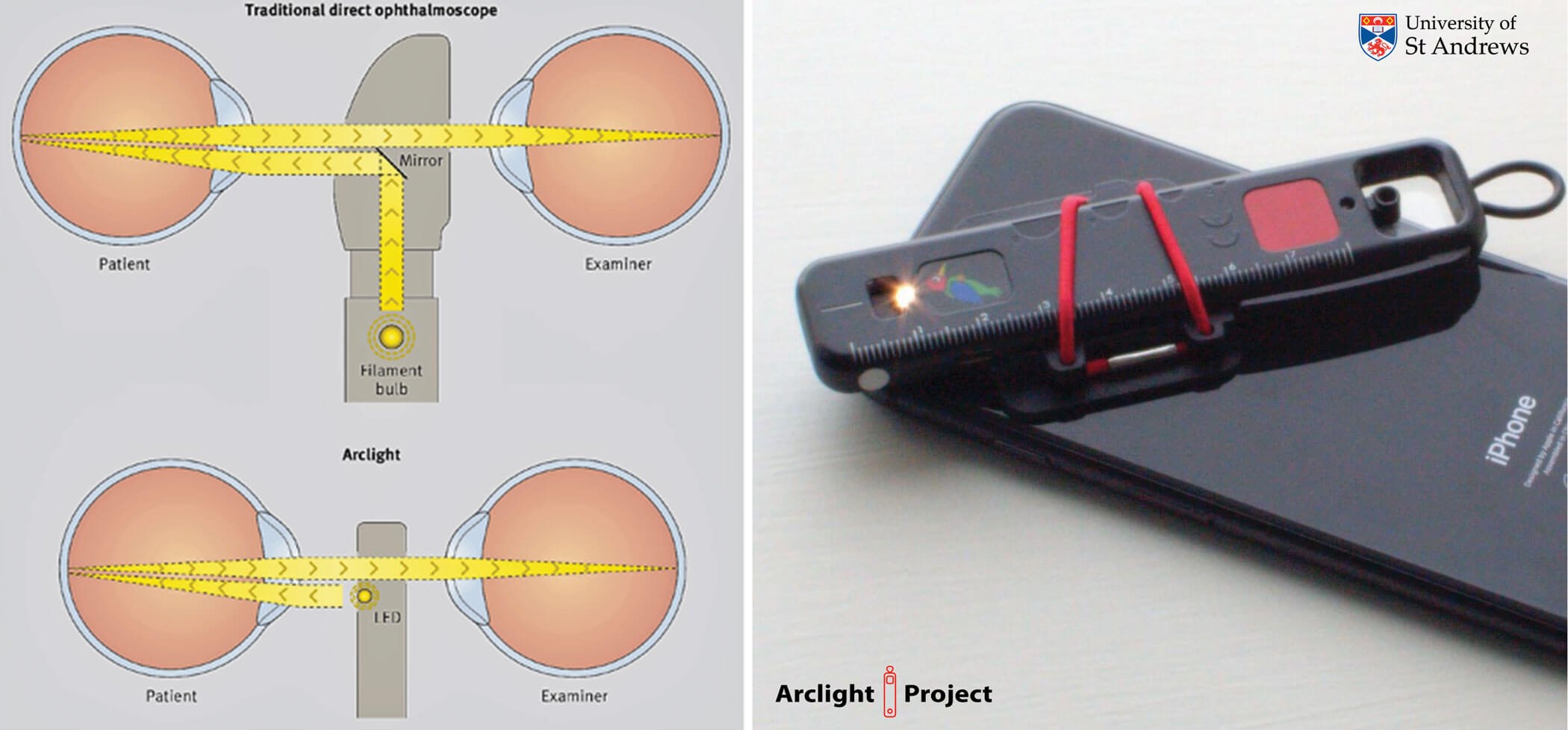
Figure 3: Frugal engineering: LED on front surface, contrasting with traditional design
reduces cost and size expanding functionality with the camera of a mobile phone.
In design, minimising part count and multifunctional sub-assemblies leads to lighter, more efficient products. Design is a balance of trade-offs, where the goal is optimised harmony. Prioritising affordability from the start prompts minimalistic specifications or inventive simplifications. Designers must always weigh needless ‘feature creep’ against genuinely useful enhancements. For instance, the Arclight device, by placing a small LED on the surface of the device just below the optics free sight hole, simplifies the design without loss of functionality (Figure 3). The LED can be driven by a slim rechargeable battery charged by a surface-mounted solar panel. This frugal engineering approach has reaped several advantages: it’s simple to use, can be attached to the camera of a mobile phone [2] for teaching and recording video, is highly portable as well as durable for use in unforgiving rural settings, and, importantly, is independent of consumables such as replacement batteries and bulbs. These are not just hard to find in resource poor settings but often expensive.
Scientific evidence base
Despite its no-frills design, the Arclight has been shown to perform, just as well, and in several ways even better than more expensive orthodox devices. Studies show there is little difference when examining the optic nerve and retina [3–5] or in identifying fundal ‘red’ reflex abnormalities to traditional tools [6]. This has also been demonstrated in the field in both Tanzania [7] and in pathology-rich clinics in India [8]. In Tanzania the effectiveness of fundal ‘red’ reflex examination in early detection of paediatric cataract and other ocular media disorders was examined. The study compared the diagnostic accuracy of different screening tools and evaluated the feasibility of community-based screenings by non-specialist nurses using the Arclight device. This work revealed that the Arclight and an expensive prototype infrared camera had similar and higher sensitivity than a pen torch for paediatric eye screening, however users preferred the simplicity and speed of using the Arclight.
This led the research team to choose Arclight in a scaled community-based feasibility study. This work was an important addition to the literature as it reported encouraging results from wide-scale, primary-care, nurse-delivered screening using Arclight for the first time. This, along with other published research, has supported a change in World Health Organization (WHO) guidelines [9], recommending for the first time the fundal ‘red’ reflex test to be performed routinely in LMICs using the Arclight device.
This goes for the otoscope function, too, where a study in the UK [10] and Malawi [11] demonstrated the otoscope function to be no different from traditional, more expensive tools. This research has led to implementation work, as well as advocacy amongst the global health ENT community, and established the Arclight otoscope as an illustrated recommended device in the WHO ENT manual [12].
The importance of binocular indirect ophthalmoscopy
In many developing areas of the world, two significant causes of blindness are on the rise. These are due to the increasing number of people with type 2 diabetes [13] and the higher survival rates of premature babies [14]. Paradoxically, these issues are partly a result of economic growth and advancements in healthcare. Consequently, two new types of blindness are emerging, adding to existing challenges: diabetic retinopathy (DR) [15] and retinopathy of prematurity (ROP) [14].
In many wealthy nations, loss of sight from DR [16] and ROP [17] is uncommon due to well-established screening programmes. The growth of DR and ROP blindness in emerging nations is, however, in large part due to a critical shortage of trained and equipped eyecare specialists. This primary challenge is compounded by many additional underlying inter-related factors including general economic constraints, geographical barriers, insufficient healthcare infrastructure, and a lack of public awareness and education about eye health.
To combat the lack of screening, we have developed an affordable binocular indirect ophthalmoscope (BIO) and innovative wide-field hemispherical retinal simulation training tools. The Arclight BIO is as effective for key eye examinations as more costly devices [18], with further research being conducted in Kenya and Indonesia to explore its effectiveness in training mid-level eyecare workers.

Figure 4: The Arclight binocular indirect ophthalmoscope and
simulation eyes for DR and ROP training workshops.
The training and assessment tools include a simulation that uses advanced algorithms to convert detailed 2D images into 180-degree curved simulation eyes. These simulations cover all stages of ROP and the complete Early Treatment Diabetic Retinopathy Study (ETDRS) images. We are currently integrating a range of glaucomatous optic nerves into these eyes to broaden their training potential. These eyes have become an indispensable part of interactive training and assessment workshops (Figure 4). They are also useful for coaching in the use of therapeutic lasers [19], further enhancing the skills of eyecare professionals.
The ‘copy and paste pitfall’: the imperative of contextualisation in diabetic retinopathy screening
We see these new tools as a means to contextualise screening to suit the reality of resource-poor regions. By doing so we aim to overcome the ‘copy and paste pitfalls’ of simply applying what is done successfully in wealthy countries to poorer regions of the world. For example, although there are many publications on digital camera screening for diabetic retinopathy in LMICs and its potential feasibility, there are few if any publications on successful scaled implementation [20].
The implementation of DR screening in LMICs face numerous obstacles, from patient identification and engagement to finding transport and meeting both direct and indirect costs. Fragmented services, lack of consolidated databases, and limited communication complicates patient outreach, while logistical and financial barriers hinder access to screening facilities. This is compounded by infrastructure deficiencies, such as unreliable internet and electricity, crucial for successfully running orthodox screening programmes.
The direct transfer of high-resource screening practices to LMICs without considering their unique socio-economic and infrastructural contexts is clearly proving to be impractical. Tailored approaches, acknowledging each LMIC’s health system realities and resource limitations, are essential to avoid the ‘copy and paste pitfall’.
A new model for DR screening using the BIO
An alternative approach utilising a BIO shows promise. Affordable and suitable for use by mid-level eyecare professionals, the BIO can screen for DR on-site in non-communicable disease clinics, reducing ungradable exams and facilitating the detection of other common blinding but also treatable eye conditions [21,22]. This method aligns with the goal of making DR screening accessible and effective in LMICs, potentially transforming patient outcomes and at the same time making advances against other causes of preventable blindness. Further research is needed to validate this approach with the frugal Arclight BIO, but the potential benefits for LMICs are considerable, offering a scalable and economically feasible screening process that invests skill and equipment in the current human resource which can be used across the full spectrum of blinding eye disease, not just DR.

Figure 5: Affordable intraocular pressure assessment: The ‘Newton’ about to start evaluation in Uganda.
Future developments
Other areas that we are working on include evaluation of a 50-pence tonometer called the Newton in Uganda (Figure 5). This uses the same principle as the Goldmann device but instead uses different weights and gravity to generate the Newtonian force upon the cornea. In time we also aim to broaden the functionality of the BIO by adding a camera and a therapeutic laser. To address uncorrected refractive error we have plans for a retinoscope and trial lenses in the same frugal style as the Arclight device. Most recently we have been working on a slit-lamp that can be handheld or corner table mounted. Bringing all this work together is Alan, an AI helper driven by a super prompt that constrains the power of GPT4 to offer teaching and support in history, examination, differential diagnosis, and management to generalists working in remote, resource-poor settings.
In the next two articles in this series we will expand on how best to use the Arclight device to examine and image eyes as well as our work with NGOs in the delivery of primary eyecare in LMICs.
References
1. Wikipedia. William of Ockham (2024).
https://en.wikipedia.org/wiki/
William_of_Ockham
2. Staniszewski B, Atukunda I, Kousha O, et al. A new technique for teaching the fundal reflex test and fundoscopy: ‘screen casting’ with the Arclight direct ophthalmoscope attached to the camera of a mobile phone. Eye (Lond) 2023. doi: 10.1038/s41433-023-02858-5 [ePub ahead of print]
3. Lowe J, Cleland CR, Mgaya E, et al. The Arclight Ophthalmoscope: A Reliable Low-Cost Alternative to the Standard Direct Ophthalmoscope. J Ophthalmol 2015;2015:743263.
4. Irfan A, Moin M, Chaudhry A, et al. Teaching ophthalmoscopy with direct versus Arclight ophthalmoscope in non-ophthalmology residents. Pak Postgrad Med J 2019;30(2):69–73.
5. Blundell R, Roberts D, Fioratou E, et al. Comparative evaluation of a novel solar powered low-cost ophthalmoscope (Arclight) by eye healthcare workers in Malawi. BMJ Innov 2018;4(2):98–102.
6. Dooley E, Kousha O, Msosa J, et al. Comparative evaluation of a low cost direct ophthalmoscope (Arclight) for red reflex assessment among healthcare workers in Malawi. BMJ Innovations 2020;6:113–6.
7. Mndeme FG, Mmbaga BT, Kim MJ, et al. Red reflex examination in reproductive and child health clinics for early detection of paediatric cataract and ocular media disorders: cross-sectional diagnostic accuracy and feasibility studies from Kilimanjaro, Tanzania. Eye (Lond) 2021;35(5):1347–53.
8. Tuteja SY, Blaikie A, Kekunnaya R. Identification of amblyogenic risk factors with the Brückner reflex test using the low-cost Arclight direct ophthalmoscope. Eye (Lond) 2021;35(11):3007–11.
9. World Health Organization. WHO recommendations on maternal and newborn care for a positive postnatal experience (2022).
https://www.who.int/publications/
i/item/9789240045989
10. Hey SY, Buckley JC, Shahsavari S, et al. A mixed methods comparative evaluation of a low cost otoscope (Arclight) with a traditional device in twenty-one clinicians. Clin Otolaryngol 2019;44(6):1101–4.
11. Balfour K, McCarthy A, Hey SY, et al. Comparative evaluation of a low-cost solar powered otoscope with a traditional device among health care workers in Malawi. Laryngoscope Investig Otolaryngol 2021;6(4):839–43.
12. World Health Organization. Primary ear and hearing care training manual (2023).
https://www.who.int/publications/
i/item/9789240069152
13. Nsabimana P, Sombié OO, Pauwels NS, et al. Association between urbanization and metabolic syndrome in low- and middle-income countries: A systematic review and meta-analysis. Nutr Metab Cardiovasc Dis 2024:34(2):235–50.
14. Wang S, Liu J, Zhang X, et al. Global, regional and national burden of retinopathy of prematurity among childhood and adolescent: a spatiotemporal analysis based on the Global Burden of Disease Study 2019. BMJ Paediatr Open 2024;8(1):e002267.
15. Bourne RRA, Steinmetz JD, Saylan M, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e144–60.
16. Hall HN, Chinn DJ, Sinclair A, Styles CJ. Epidemiology of blindness attributable to diabetes in Scotland: Change over 20 years in a defined population. Diabet Med 2013;30(11):1349–54.
17. Royal College of Paediatrics and Child Health. UK screening of retinopathy of prematurity guideline: Summary of recommendations (2022).
https://www.rcpch.ac.uk/resources/screening
-retinopathy-prematurity-rop-clinical-guideline
18. Kousha O, Ganesananthan S, Shahin B, et al. Comparative evaluation of a new frugal binocular indirect ophthalmoscope. Eye (Lond) 2023;37(1):160–2.
19. Kousha O, Staniszewski B, Ulloa JL, et al. Frugal retinal laser training simulation eyes. Eye (Lond) 2022;36(5):1129–30.
20. Curran K, Piyasena P, Congdon N, et al. Inclusion of diabetic retinopathy screening strategies in national-level diabetes care planning in low- and middle-income countries: a scoping review. Health Res Policy Syst 2023;21(1):2.
21. Namperumalsamy P, Nirmalan PK, Ramasamy K. Developing a Screening Program to Detect Sight-Threatening Diabetic Retinopathy in South India. Diabetes Care 2003;26(6):1831–5.
22. Malerbi FK, Morales PH, Farah ME, et al. Comparison between binocular indirect ophthalmoscopy and digital retinography for diabetic retinopathy screening: The multicenter Brazilian Type 1 Diabetes Study. Diabetol Metab Syndr 2015;7(1).
[All links last accessed February 2024]
Declaration of competing interests:
Andrew Blaikie is a part-time employee of the University of St Andrews. The University own a subsidiary social enterprise that sells Arclight Project tools in the UK. Profits from these sales are used to support distribution of Arclight Project tools at cost price to resource poor countries. Andrew Blaikie has no direct financial benefit from sales.
COMMENTS ARE WELCOME