In this three-part series (Click here for Part 1 and here for Part 3) Andrew Blaikie and his team explore the role and application of the Arclight Device in Imaging of the Eye.
There are many different types of ophthalmic imaging tools; from simply taking a photograph of the front of the eye with a mobile phone camera to looking in fine detail at the structure and function of the retina with optical coherence tomography (OCT).
In low-resource settings access to ophthalmic imaging devices is largely restricted to tertiary referral hospital or private facilities [1]. Many devices are not fully functional and, access to spare parts or an engineer can be limited and expensive.
Role of the Arclight device in imaging of the eye
Smart phone ownership amongst healthcare workers in lower- to middle-income countries (LMICs) is increasing [2]. To make the most of this opportunity, a dedicated clip can be used to align either end of the Arclight device (anterior segment loupe or direct ophthalmoscope) to the camera of most mobile phones [3].

Figures 1A–F: (A) arclight, phone and clip; (B) remove paper from sticker; (C) align tip of arrow with centre of lens and stick to phone; (D) remove the black arrow; (E) switch Arclight on and attach using the elastic; (F) slide Arclight toward camera aligning sight hole to lens.
The clip can be attached to either the body of the phone or phone case (Figure 1) by removing the yellow paper to reveal a sticky surface. Line up the tip of the arrow to the centre of the lens that acquires video. In this position carefully stick the clip to either the body of the phone or a plastic cover. Once aligned and stuck down, remove the arrow. The clip is now at the correct distance from the lens of the camera to allow both sight holes of the Arclight to be aligned accurately and easily for imaging. To image with the Arclight, switch it on and place it in the clip, facing outwards. Stretch the elastic over the device and secure. Slide the Arclight toward the camera until it stops in the correct position, aligned with the centre of the lens.
To acquire video of an examination, open the usual camera application on the phone. Turn off the flash setting of the camera as we will be using the CE-accredited LED of the Arclight. Examine with the Arclight as normal but use the screen of the phone to observe the clinical signs. Videos on how to use the Arclight to examine the eye are found at www.https://medicine.st-andrews.ac.uk/arclight/ This approach offers the opportunity to capture video and select still images of both the anterior and posterior segment of the eye and all associated clinical signs (Figure 2).

Figures 2A–C: (A) examine as normal; (B) anterior segment; (C) posterior segment.
Benefits of imaging
There are several benefits to being able to image the eye.
- A ‘baseline’ image allows observation of response to treatment, especially helpful in infectious keratitis and optic disc cupping.
- Capturing video of clinical signs in otherwise hard to examine, uncooperative children for later review can be invaluable.
- Sharing an image with a remote colleague for a second opinion to help make a diagnosis and management plan (especially useful in planning for trauma cases) can improve patient care.
- Patient communication can be enriched by presenting an image of ‘the problem’ to the patient or carer.
- Training students and trainees using clinical videos is an engaging means to enhance their education especially if ‘casting’ is also employed [3].
General tips on imaging
- Ensure you have consent to capture and share images.
- The lens rack on the Arclight should be set to the highest position where there is no lens power, just a pinhole.
- On the camera, open the usual video app and select the highest resolution and frames per second setting. Once imaging, maximise zoom to fill the screen with the area of interest. Reviewing the captured video will allow you to screen grab the most illustrative image.
- Anterior Segment imaging should be performed in a well-illuminated room or better, outside with lots of light.
- Fundal ‘red’ reflex and posterior segment capture is best done in a dim room using manual ‘pro’ mode control with autofocus, auto-brightness and camera flashlight switched off. This permits selection of the preferred focal plane, creates clearer, more stable imaging of the structures you want to see, and reduces over-exposure of paler structures such as the optic nerve.

Figures 3A–H (adult anterior segment): (A) bacterial keratitis and hypopyon; (B) herpes simplex keratitis; (C) infiltrate with sectorial injection; (D) pterygium; (E) ocular surface neoplasia; (F) peripheral ulcerative keratitis with iris prolapse; (G) Blunt trauma with globe rupture; (H) Penetrating Injury , iris prolapse and traumatic cataract.

Figures 4A–H (paediatric anterior segment images using both the loupe and the direct ophthalmoscope for the fundal reflex): (A) limbal dermoid; (B) corneal scar and anterior polar cataract; (C) posterior polar cataract; (D) xerophthalmia; (E) keratoconus; (F) molluscum contagiosum; (G) coloboma; (H) retinoblastoma.
Anterior segment imaging
The anterior segment loupe of the Arclight has a 14D lens giving a working distance of around 6cm and a magnification of 6x. Using either the bright white or blue LED (with addition of fluorescein), all the important anterior segment disorders of adults (Figure 3) as well as children (Figure 4) can be seen and acquired.
Uncooperative child
Capturing a short video of the anterior segment examination can be especially useful in an uncooperative child. The blue / white flashing light setting is especially intriguing to young children. They find it hard to resist looking at the lights. This can be helpful in chemical injuries or trauma where exclusion of a more serious or penetrating injury is important. Reviewing the video in slow motion can allow clinical signs to be seen that would otherwise be hard to identify or confirm. They also offer an opportunity to discuss findings with parents and carers.

Figures 5A–H (cataract images using both the loupe and the direct ophthalmoscope for the fundal reflex): (A) dislocated mature cataract; (B) mature cataract dislocated into the anterior chamber; (C) well-centred intraocular lens (IOL); (D) IOL displaced superiorly; (E) IOL displaced inferiorly; (F) IOL and capsular bag displaced inferiorly; (G) anterior chamber IOL and peripheral iridotomy; (H) posterior capsule opacification.
Cataract
We have found the Arclight to be exceptionally useful in high-volume cataract camps. Assessment of patients preoperatively as well as reviewing large numbers postoperatively can be done rapidly and reliably. By using a combination of the anterior segment loupe and the direct ophthalmoscope an overall sense of the type of cataract can be gained allowing quick and reliable decisions to be made (Figure 5). The device is also increasingly finding an important role in busy phacoemulsification services. A brief pre-op examination when saying hello to patients can identify those that will be needing pupil expansion devices or ‘trypan blue’ to pre-empt the nursing team.
The fundal reflex test
The fundal reflex test is routinely performed in all newborns and infants in the UK. A positive test can lead to early identification of cataract, retinoblastoma, and congenital eye disease leading to better outcomes. With some practice, it is also possible to use the pattern of distribution of colour between and within the pupil space to recognise refractive error or squint. This level of interpretation is called the Bruckner reflex test (Figure 4, 6).
World Health Organization (WHO) recommendations
The World Health Organization (WHO) has, for the first time, now also recommended for this test to be performed on all newborns and infants in LMICs [4]. This is in part a result of the evidence base that has developed demonstrating the Arclight to work as effectively as more expensive traditional devices, as well as advocacy work by the London School of Hygiene and Tropical Medicine.

Figures 6A–F (fundal reflex of children): (A) normal reflex black African infant; (B) normal reflex white European baby; (C) normal reflex Asian child; (D) left posterior polar cataract; (E) myopic reflex; (F) right exotropia.
A racially equitable term; the fundal reflex test
Recent growing acknowledgment of the varied and non-red appearance of the ‘red’ reflex test in those with skin of different pigmentation (Figure 6) is leading to a shift towards using a more equitable anatomical term, such as the fundal reflex test [5].
Optic nerve
When performing fundoscopy, follow the horizontal 15-degree temporal ‘flight path’ to bring the optic nerve into view. The small field but high magnification of direct ophthalmoscope allows for detailed imaging of the disc. This is essential when assessing any patient with visual disturbance or headache. The range of optic nerve signs that can be imaged is illustrated in Figure 7.

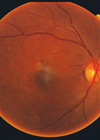
Figures 7A–H (optic nerves): (A) normal; (B) grossly swollen with haemorrhage and exudate; (C) advanced glaucomatous cupping; (D) diffuse atrophy; (E) temporal atrophy; (F) new vessels at disc; (G) gross hypoplasia; (H) myelinated nerve fibres.
Retina
After having viewed the optic nerve, moving temporally, toward the ear, or by asking the patient to “look at the bright light” (of the Arclight), the macula and fovea will be brought into view. It is important for patients to be dilated in order to examine the macula. If not dilated the pupil will constrict and the view is lost. After examining the macula, directing the Arclight along the major arcade vessels can reveal many other signs as shown in Figure 8.

Figures 8A–H (retina): (A) diabetic maculopathy; (B) retinitis pigmentosa; (C) coloboma; (D) retinal detachment; (E) arteriolar ghost vessels; (F) macular star; (G) toxoplasmosis; (H) full thickness macular hole.
Future work
We have started working on several computer science initiatives related to the image capture potential of the Arclight. These include stitching frames from video together to create a wider field image [6], segmentation of the disc for cupping, artificial intelligence analysis of images, and telemedicine opportunities with several of the recognised commercial platforms.
In the next article we will expand on our work with eyecare Non governmental organization (NGOs) in training and equipping in resource-poor regions of the world.
References
1. Patel D, Mercer E, Mason I. Ophthalmic equipment survey 2010: preliminary results. CEHJ 2010;23(73):1–3.
2. The State of Mobile Internet Connectivity Report 2023 (2023). Global System for Mobile Communications Association.
https://www.gsma.com/r/somic/
3. Staniszewski B, Atukunda I, Kousha O, et al. A new technique for teaching the fundal reflex test and fundoscopy: ‘screen casting’ with the Arclight direct ophthalmoscope attached to the camera of a mobile phone. Eye (Lond) 2023.
https://pubmed.ncbi.nlm.nih.gov/38081937/
[ePub ahead of print].
4. WHO recommendations on maternal and newborn care for a positive postnatal experience (2022). World Health Organization.
https://www.who.int/publications/i/
item/9789240045989
5. Examination of the Eyes and Vision – OSCE Guide (2024). Geeky Medics.
https://geekymedics.com/
eye-examination-osce-guide/
6. Viquez KDC, Arandjelović O, Blaikie A, Hwang IA. Synthesising Wider Field Images from Narrow-Field Retinal Video Acquired Using a Low-Cost Direct Ophthalmoscope (Arclight) Attached to a Smartphone (2018). Proceedings - 2017 IEEE International Conference on Computer Vision Workshops, ICCVW 2017.
[All links last accessed April 2024]
Declaration of competing interests: Andrew Blaikie is a part-time employee of the University of St Andrews. The University own a subsidiary social enterprise that sells Arclight Project tools in the UK. Profits from these sales are used to support distribution of Arclight Project tools at cost price to resource poor countries. Andrew Blaikie has no direct financial benefit from sales.
COMMENTS ARE WELCOME