Malawi’s population is mostly rural; the government and Christian Health Association of Malawi (CHAM) together deliver about 80% of healthcare services through local district and community health facilities [1]. However, ophthalmology specialist services are only concentrated in the central hospitals.
Thus, mid-level eyecare workers serve in most of the public and CHAM health facilities and constitute a majority of the ophthalmic workforce in Malawi [2]. The Malawi Standard Treatment Guidelines for eye health were developed to assist these eye health workers in managing common ophthalmic conditions in the community [3]. Treatment guidelines promote consistent use of treatment protocols ensuring quality standardised care for all. However, healthcare workers find it difficult to access, search and navigate these guidelines.
A survey of mid-level eye health workers in Malawi reported that 44% had no access to these guidelines and had never been able to use them. Budget constraints for printing prevent wide-scale distribution.
The survey also reported that 88% of respondents thought enhanced availability of the guidelines through an app would be extremely useful, as the majority of mid-level eye healthcare workers have access to a smartphone. Smartphones are already used to inform clinical decisions via WhatsApp groups that are used to facilitate patient referrals, remote consultations and document sharing.
Apart from the inconsistent use of treatment guidelines, the eye health workforce faces limited access to training and CPD, particularly for rural health workers who have long distances to travel to organised meetings. In addition, they are often the only eye health specialists in their area, making it difficult for them to take time away from the workplace.
There has been a partnership between Kamuzu University of Health Sciences (KUHeS) Malawi, NHS Scotland and the International Centre for Eye Health (ICEH) for 20 years. This partnership has worked together to strengthen paediatric ophthalmology [4], management of diabetic eye disease and research [5]. The aim of this project was to make the guidelines universally available to healthcare workers. The Partnership came together to convert the eye diseases section of the Malawi Standard Treatment Guidelines (MSTG) into an online and offline mobile application to provide accessible, evidence-based protocols and CPD capabilities for the entire eyecare workforce in Malawi.
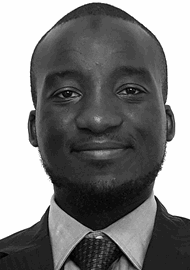
Figures 1a–c: Snap shots from the Malawi Eye Care app.
The need for this project was identified through consultations with key stakeholders, including the Ministry of Health, Kamuzu University of Health Sciences, the Ophthalmological Society of Malawi, and front-line eye health professionals. The partnership for this project built on the complementary expertise of the long-standing partners in the UK and Malawi. Kamuzu University of Health Sciences, Department of Ophthalmology, brought a deep understanding of local eye health needs and healthcare systems and collaborated with the University of Malawi (UNIMA) and Ministry of Health on digital application development in this programme. The UK-based ICEH, supported by the NHS Fife Department of Ophthalmology, contributed expertise in guideline development, advanced clinical practices, and digital health innovations.
The Ministry of Health CPD department and Medical Council of Malawi, alongside the Ophthalmological Society of Malawi all contributed expertise in development, moderation and validation of the CPD content. Leveraging this existing local and international expertise made the goal achievable within the specified timeline and resources. This collaboration aimed to strengthen Malawi’s capacity for standardised eye care delivery while enhancing the UK partners’ experience in treatment guideline development and implementation of digital health solutions in different healthcare settings.

Figure 2: Team photo from the Malawi Eye Care App Dissemination Workshop.
Aims
To create the Malawi Eye Care Mobile Application, which is available online and offline, for daily use to access the Malawi standard treatment guidelines to improve eye care and enhance education and access to CPD.
Methods
An expert taskforce was convened to review the MSTG eye disease section and prepare for a content workshop which adapted existing MSTG guidelines into a mobile-friendly format and identified the technical features required for the mobile application. The app was developed locally by the University of Malawi’s Computer Science Department. There were weekly zoom meetings during the app content creation / adaptation stage. After feedback following beta testing in six clinical facilities by optometrists and ophthalmic clinical officers, the app was finalised.
The app developed three sections on the home page. Firstly, a clinical guidelines tab which enables the user to choose specific eye conditions such as keratitis, retinoblastoma and diabetic retinopathy and access the MSTG for this specific condition. Sections were created for symptoms and signs, investigations, and treatment and patient information for each condition so that the healthcare worker can check that the condition they have diagnosed matches with the patient’s history and examination. They can then access the guideline treatment for this condition including drops and dose and give the patient advice on self-management. There is also a series of multiple choice questions (MCQs) at the end of some of these conditions to allow the healthcare worker to study more about the condition and obtain some CPD if they complete the questionnaire successfully.
The second option on the homepage allows the eye health worker to access the World Health Organization (WHO) primary eyecare clinical algorithms to aid in diagnosis of people with loss of vision, a red eye, swelling / lump on eye or abnormal lashes, trauma and children aged five years and under who present with an eye problem. The third section contains the CPD section. To create this there was a CPD content development workshop local team working with the UK NHS Partner and ICEH. This created 13 cases with clinical photographs followed by MCQs as well as four in-depth learning topics – one point was allocated to each successfully completed learning section and half a point for completing a case scenario section. The app aims to provide a maximum of 10 points per year (one third of CPD points required per year).
User testing of the mobile application was carried out. The digital health department, UNIMA, the Ministry of Health digital unit and the eye health workforce conducted training workshops. The app was created to have built-in analytics to monitor usage and impact, enable ongoing optimisation, CPD award integration and future creation of CPD. An android version of the app was prioritised after a survey showed that a large majority of secondary eye health workers have Android phones only. A workshop for secondary healthcare workers was held to launch the app and to skill up the health workers in the use of the app in August 2025.
Results
The project has delivered the Malawi Eye Care Mobile App. An android version of the app was developed and delivered for alpha and beta testing after four months from project inception.
The app was officially launched in Malawi on 25 August 2025 at Bingu International Conference Centre, Lilongwe Malawi. The guest of honour at the official launch was Secretary for Health Dr Samson Mndolo, who appreciated that the innovation was a step in the right direction and expressed hope that other groups in the medical sector will do the same to ensure standardisation of care across the country.
The launch was attended by 94 delegates comprising ophthalmic clinical officers, ophthalmic nurses, optometrists and ophthalmologists and ophthalmology residents. The majority were male (72%). At the workshop, an APK file format was available for download and installation on their android phones but the app became available on the Google Play Store by the end of August. Within three hours, 89 out of 90 were able to access the app on their phones at the app launching workshop.
The workshop taught the delegates to navigate the app, access the guidelines and WHO algorithms and how to use these in clinical situations. The delegates practised with the CPD section including completing a quiz, and obtaining and downloading a CPD certificate. The app can be accessed at all times offline and does not use data. Connection to Wi-Fi or data is chosen by the user so that they can synchronise completed quizzes and obtain CPD points and download certificates.
Following the training of the app, 98% responded that the app will be useful in clinical practice. Ninety-three percent of the participants were ophthalmic clinicians and optometrists. In addition, 93% of the participants were satisfied with the quality of the training in using the app. All workshop participants reported that the CPD aspect of the app will be useful.
The app was also presented at the COECSA Conference in Addis Ababa through a presentation at the Young Ophthalmology Forum session. The presentation was also shared during a plenary session to delegates from 11 different countries with an emphasis on this being an innovation suitable for countries in Africa facing similar challenges due to limited access to treatment guidelines.
Conclusion
This app allows all healthcare workers access to national guidelines and CPD. It represents an innovative use of a smart phone which is in the pockets of all secondary eye health workers and is the first example of this in sub-Saharan Africa.
Many primary healthcare workers have access to tablets as part of the child immunisation programme and could also use the WHO primary eyecare algorithms to aid diagnosis and referral of eye conditions. The availability of patient information aims to empower all healthcare workers to accurately educate their patients in self-management of eye conditions and better inform them of what to expect and encourage attendance if referral to an eye hospital is recommended. The engagement with content on continuous learning and development for eye healthcare workers can now be easily demonstrated with this app. Collaboration with the Ministry of Health and Medical Council of Malawi was very important in standardising the CPD content and awarding of points.
The reason that this initiative could be achieved in a few months was due to the long-standing partnerships in place between Malawi and the UK since 2005 as part of the VISION 2020 LINKS and Networks programme. It was also supported by the Global Health Partnership and Department of Health and Social Care. The existence of the MSTGs for eyecare was also very important in being able to launch the app swiftly because guideline creation can take a lot of time. While we were fortunate to have the MSTG, we were restricted to those conditions in the guidelines only. In the future we intend to expand the range of conditions on the app.
Malawi Samson Mndolo described the project as a milestone in digital health, saying that the “initiative demonstrates the power of partnerships in strengthening our health system. It will build capacity and improve service delivery particularly in underserved communities.” With the Ministry of Health’s endorsement, the successful implementation of this project offers the potential to scale it to all diseases in the MSTG, creating a long-term impact beyond eye health services.
TAKE HOME MESSAGES
-
Guidelines for eyecare are important to promote consistent management of eye care conditions.
-
The availability and use of smartphones is common in all healthcare settings and is already facilitating patient care.
-
A mobile app available offline enables all healthcare workers access to treatment guidelines and continuous professional development.
References
1. Mchenga M, Manthalu G, Chingwanda A, Chirwa E. Developing Malawi’s Universal Health Coverage Index. FrontHealth Serv 2022;1:786186.
2. Kayange P. Sub-specialization; Is it the way to go? JOECSA
https://joecsa.coecsa.org/index.php/
joecsa/article/view/150
3. https://extranet.who.int/ncdccs/
Data/MWI_D1_Malawi-Standard-Treatment
-Guidelines-Essential-Medicines-List-2015.pdf
4. Lavy T, Msukwa G, Mackinnon J, et al. Development of paediatric ophthalmology services in Malawi: the VISION 2020 LINK between Blantyre and Glasgow. Eye News 2020;27(2):32–3.
5. Annoh R, Msosa J, Styles C, et al. Building capacity for diabetic retinopathy services in Malawi. Eye News 2020;26(2):28–34.
[All links last accessed October 2025]