Toxic optic neuropathy are a group of conditions manifested by reduction of visual functions secondary to damage to the anterior visual pathways from exposure to a toxin. The implicated toxin could be work-based, food or drink related, or iatrogenic medication.
Signs and symptoms
The usual presentation is bilateral chronic progressive reduction of vision. This is usually painless and symmetrical associated with loss of colour vision and a central or cecocentral scotoma. Some patients might have slightly asymmetric presentation in the early stages of the condition.
This condition can affect all ages, races, and genders. The level of vision loss can vary from moderate loss to severe complete loss of vision. The loss of colour of vision is likely to be one of the early signs and is usually more pronounced compared to other symptoms.
Depending on the level of vision loss, the pupil reaction might become sluggish, but without a relative afferent pupillary defect (RAPD) as the condition is bilateral and symmetrical.
Fundus examination will reveal bilateral temporal optic nerve pallor with loss of the nerve fibre layer in the papillomacular bundle and loss of the ganglion cell layer corresponding to the level of vision loss. With the exception of amiodarone and methanol toxicity, TON doesn’t present with a swollen optic nerve.
Visual fields testing will show a central or cecocentral scotoma with minimal or no peripheral loss.
Aetiology
It is still not fully established what is the exact mechanism of action for this condition, but it is thought to be multifactorial with metabolic and vascular factors. Majority of patients will have a history of excessive alcohol or smoking. These patients will also have reduced levels of vitamins, especially vitamin B1, B12 and folic acid. These deficiencies can lead to accumulation of toxin by-products and neurotoxicity. This is in addition to the toxic effect of alcohol and its by-products. There is increasing evidence that toxin and nutritional optic neuropathies are caused by damage to the mitochondria in the ganglion cells in the retina.
Investigations
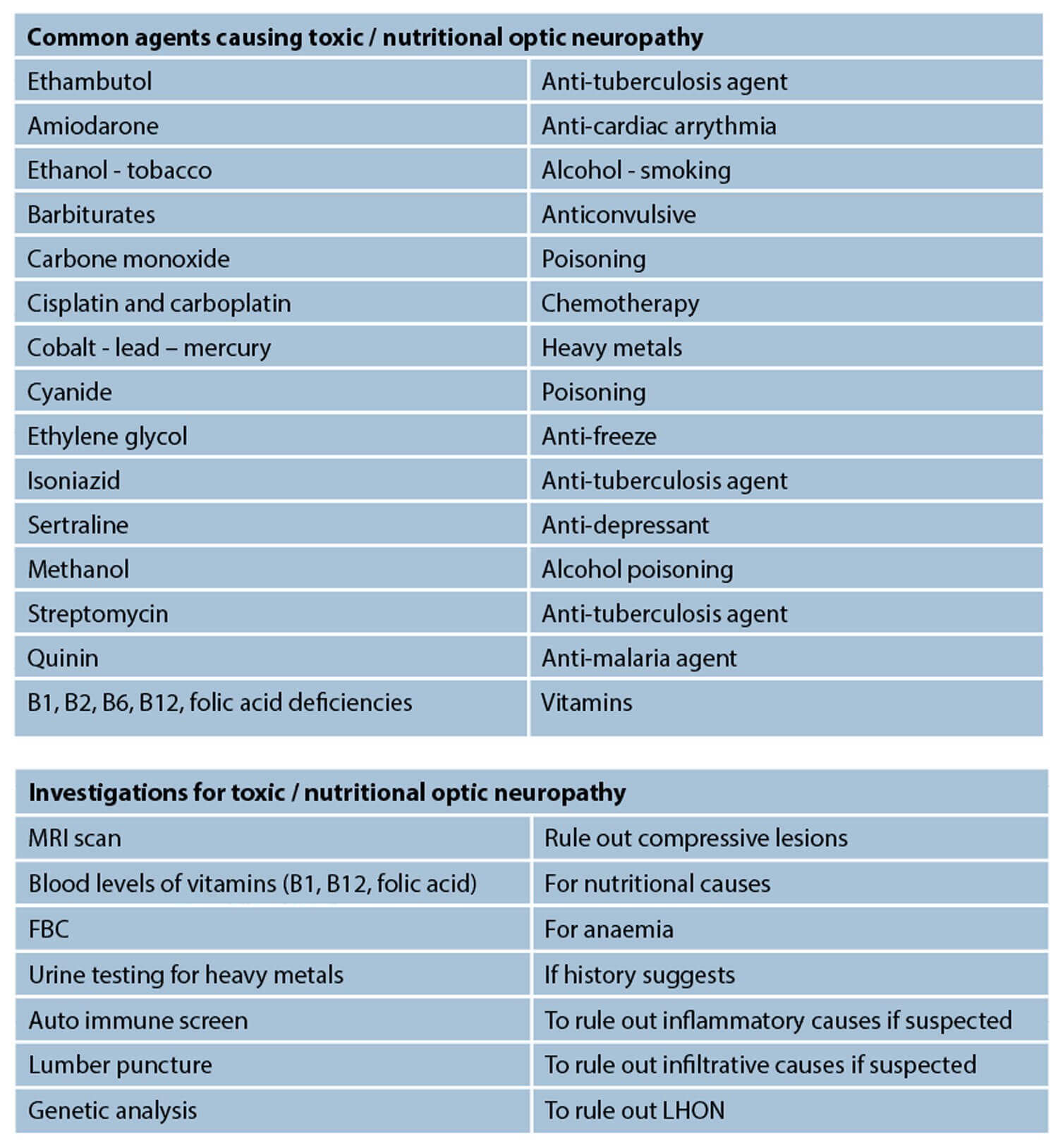
Following a full detailed history including social and professional history, patients will need full ophthalmic examination and fundus imaging to assess the structure of the retina and optic nerves. All patients will also require colour vision testing as well as fields testing. Blood tests including full blood count and vitamin levels (vit B1, B12, folic acid) and ferritin assay are necessary. Depending on clinical suspicion and history, blood tests for levels of heavy elements such as lead, or specific toxins can be done. All patients with pale optic nerves of unknown cause will require neuroimaging in the form of an MRI scan to assess the visual pathway structures and rule out other possible causes.
There is very little role for electrodiagnostic testing in these cases unless the loss of vision or the pallor are subtle. When performed it will show significant reduction in the amplitude of the visual evoked potential (VEP) with normal latency and normal electroretinogram (ERG).
Differential diagnosis
Other causes that can present like TON include chronic compressive optic neuropathy from an intracranial lesion or hereditary optic neuropathy, especially Leber’s hereditary optic neuropathy (LHON).
LHON can present with bilateral loss of vision, but it is usually sequential and is sudden onset compared to TON. In cases when this is suspected, genetic mapping can be done, especially for the three common mutations in the mitochondrial DNA.
Common causes of neurotoxicity
Alcohol and tobacco: these agents are commonly noted in patients with toxic and nutritional optic neuropathies. A combination of toxicity and reduced vitamin levels is usually the postulated mechanism.
Ethambutol: this is used commonly as treatment for tuberculosis. Toxicity is dose-dependent and is likely to be due to mitochondrial damage, and symptoms are usually gradual blurring of vision with nasal visual field defects. Stopping it will usually result in reversal of the signs unless severe optic atrophy has happened already.
Isoniazid: very similar to ethambutol and more of a concern if both medications are combined. Methanol: severely damaging toxic agent which can lead to acute loss of vision bilaterally, but the history clearly differentiates this.
Amiodarone: this anti-cardiac arrythmia medication is associated with a bilateral optic neuropathy that have similar features to anterior ischaemic optic neuropathy (NAION). It presents with reduced vision, a field defect, a RPAD (if unilateral or asymmetric), and a swollen optic nerve. However, there are several differentiating points as it usually causes bilateral simultaneous involvement with gradual onset and the swelling persists a lot longer than NAION.
Nutritional optic neuropathy: with reduced vitamins, especially thiamine (B1), vitamin B12 and folic acid. They usually have associated anaemia and possibly neurological deficits. It is important to ask relevant history questions regarding diet or gastrointestinal disease or any bariatric surgery which could help with the diagnosis. Blood tests checking for vitamin levels usually reveals the diagnosis and can be treated with replacement.
Heavy metals: examples would be lead or mercury. History of industrial exposure could help in the diagnosis and blood testing will reveal high levels.
References
1. Sharma P, Sharma R. Toxic optic neuropathy. Indian J Ophthalmol 2011;59(2):137-41.
2. Lee AG, Zubidi AN, Spitze A, Yalamanchili S. Questions and Answers in Neuro-Ophthalmology: A Case-Based Approach. Singapore; World Scientific Publishing; 2014:23-36.
3. Martin TJ, Corbett JJ. Practical Neuroophthalmology. New York, USA; McGraw Hill; 2013:122-4.
4. Schiefer U, Wilhelm H, Hart W. Clinical Neuro-Ophthalmology. New York, USA; Springer; 2007:223-32.
5. Smith SV, Lee AG, Brazis PW. Clinical Pathways in Neuro-Ophthalmology: An Evidence-Based Approach. New York, USA; Thieme; 2003:17-9.
COMMENTS ARE WELCOME