Introduction
Optic neuritis (ON) is an inflammatory process affecting the optic nerve. After glaucoma, it is the most common optic neuropathy affecting patients under the age of 50. The usual presentation of typical ON is unilateral subacute loss of vision preceded with some retrobulbar pain especially on eye movement. It most commonly affects young, otherwise healthy, females.
Although many autoimmune conditions such as sarcoidosis and systemic lupus erythematosus (SLE) can cause ON along with many infectious and para infectious and post vaccination causes have been recognised, the majority of ON can are secondary to demyelinating conditions. In adult patients, these include multiple sclerosis (MS), neuro myelitis optica (NMO) and myelin oligodendrocyte glycoprotein (MOG) related disease (MOGAD).
There have been many papers on optic neuritis, its aetiology, presentation and management. In this short article I will briefly discuss demyelinating optic neuritis presentation, its typical features and management plans.
Aetiology
Demyelinating conditions can affect the myelin sheath of the optic nerve leading to ON episode. This can be an isolated episode as in clinically isolated syndrome (CIS), MS related (MS-ON), NMO related (NMO-ON) or MOGAD. There are other rarer associations as well.
Presentation
Table 1 summarises features of typical ON presentation [1]. The more deviation from the typical presentation, the more atypical the ON is with increased need for more in depth investigations.
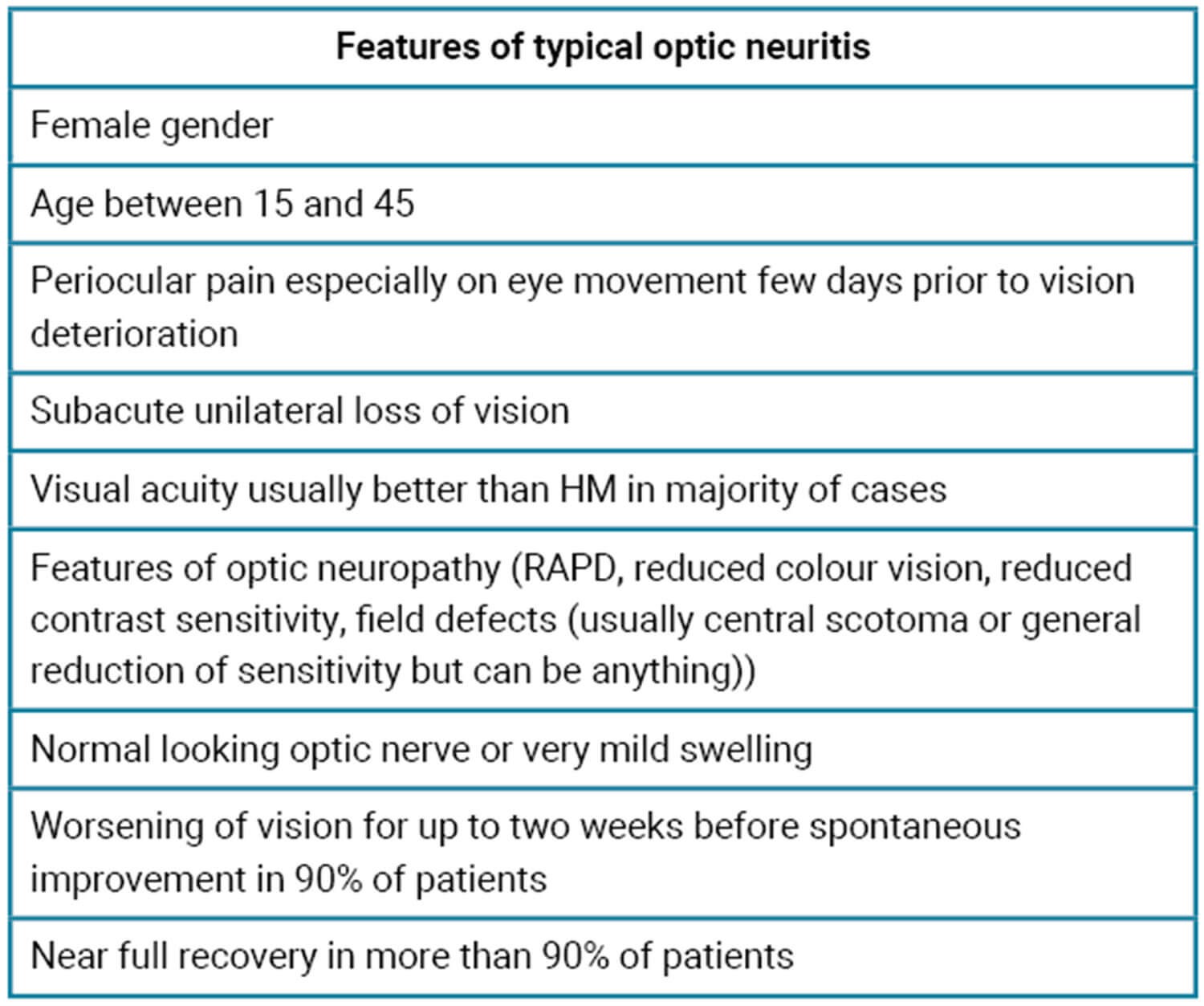
Table 1: Features of typical optic neuritis, adapted from Hoorbakht, et al [1].
Differential diagnosis
- Any other cause of inflammatory optic neuropathy
- Non-arteritic anterior ischaemic optic neuropathy (NAION)
- Compressive optic neuropathy
- Leber’s hereditary optic neuropathy (LHON).
Diagnosis criteria
There is no consensus on the criteria to diagnose ON. Majority of the diagnoses depends on clinical features as well as some laboratory and imaging investigations. A recent paper published in 2022 suggested some criteria to reduce misdiagnosis of ON based of the opinion of more than 100 experts in neuro ophthalmology [2].
Table 2 summarises clinical and investigation features needed to reach a diagnosis of ON.
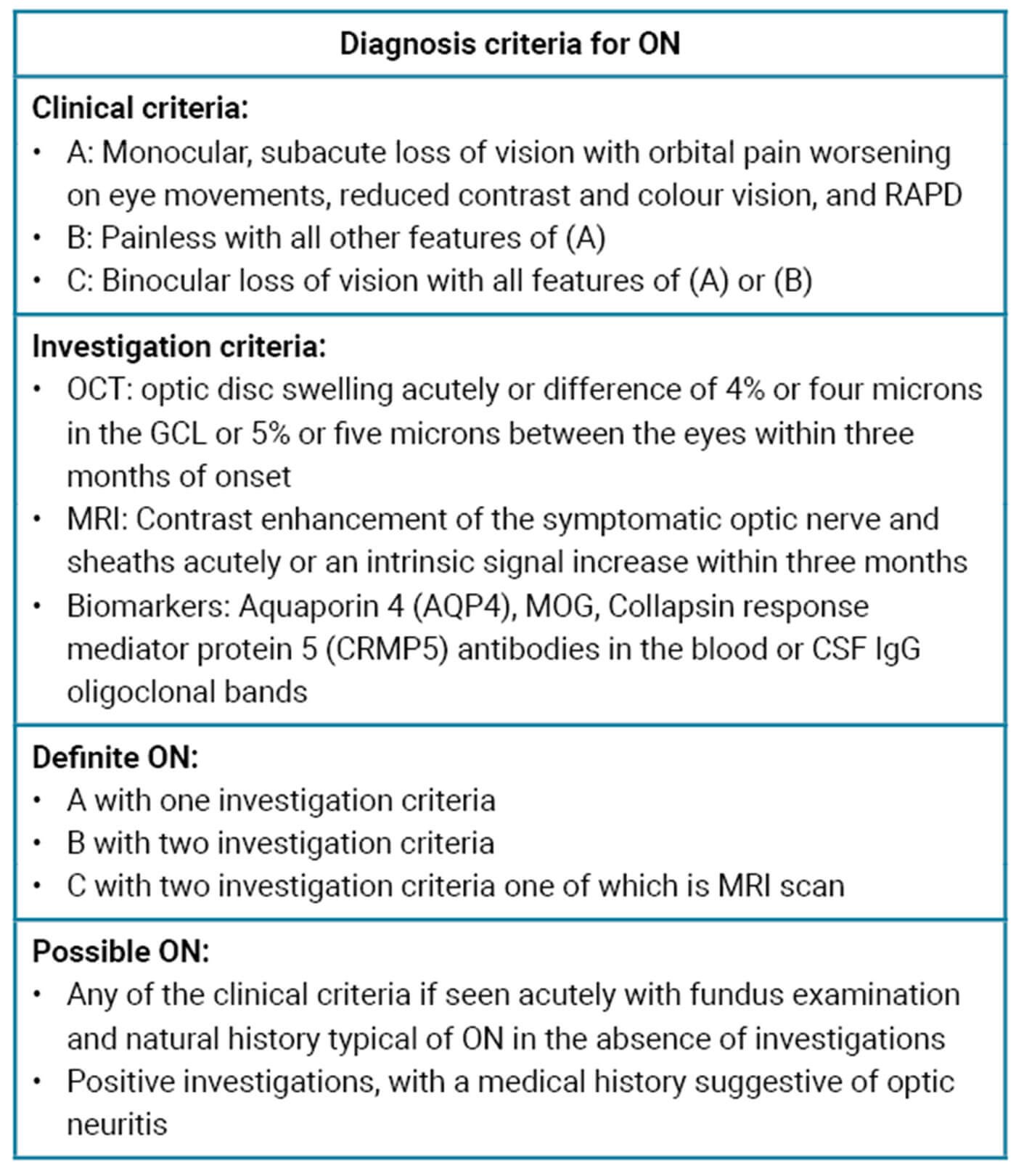
Table 2: Diagnosis criteria of optic neuritis, adapted from Petzold, et al [2].
Optic neuritis in MS, NMO and MOG conditions
Optic neuritis is usually part of the spectrum of presentations in these demyelinating conditions. It can be the first presenting feature which poses a dilemma and a challenge to the clinician on how to manage this ON case.
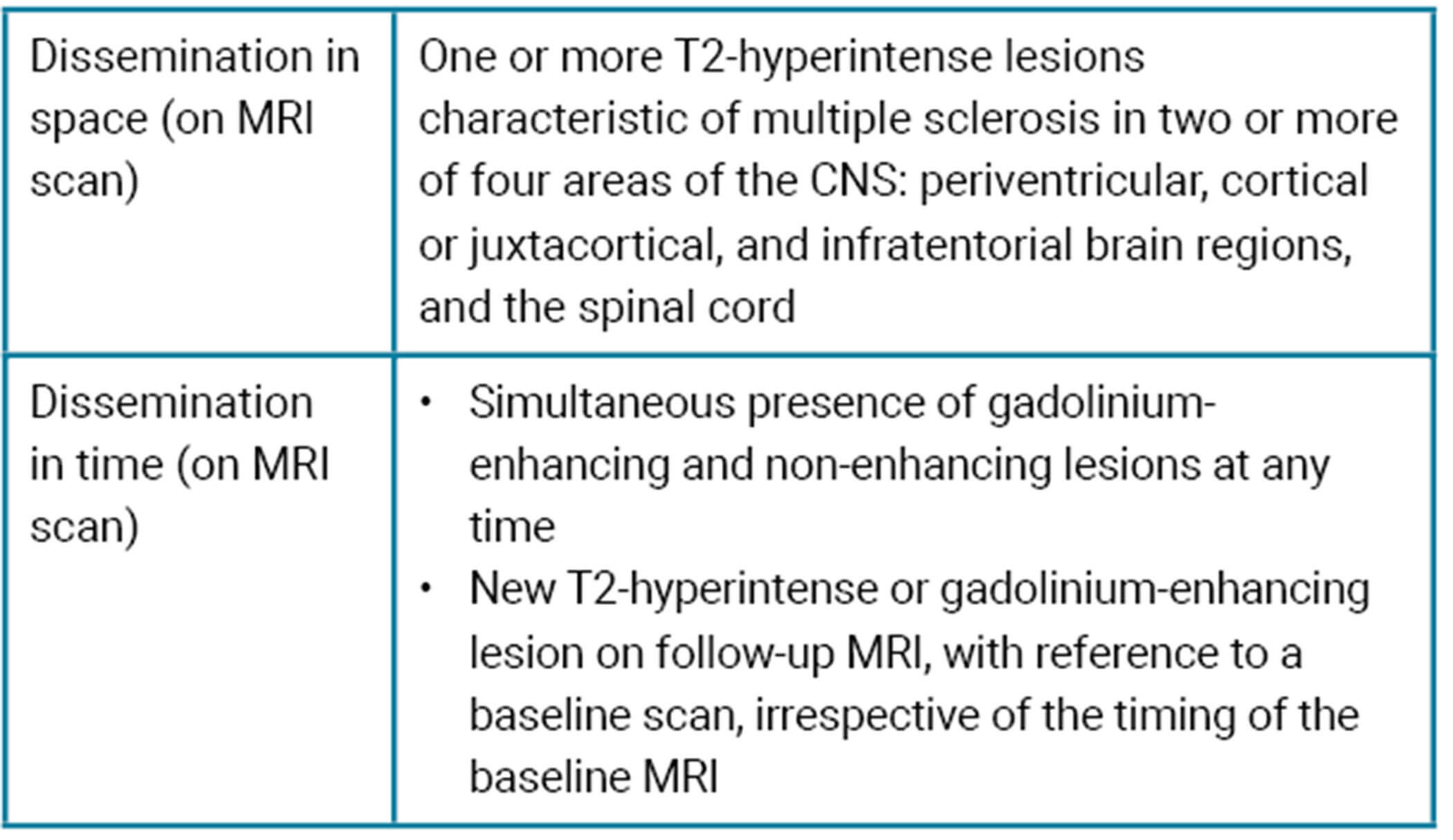
Table 3: Dissemination criteria for MS diagnosis, adapted from Thompson, et al [3].
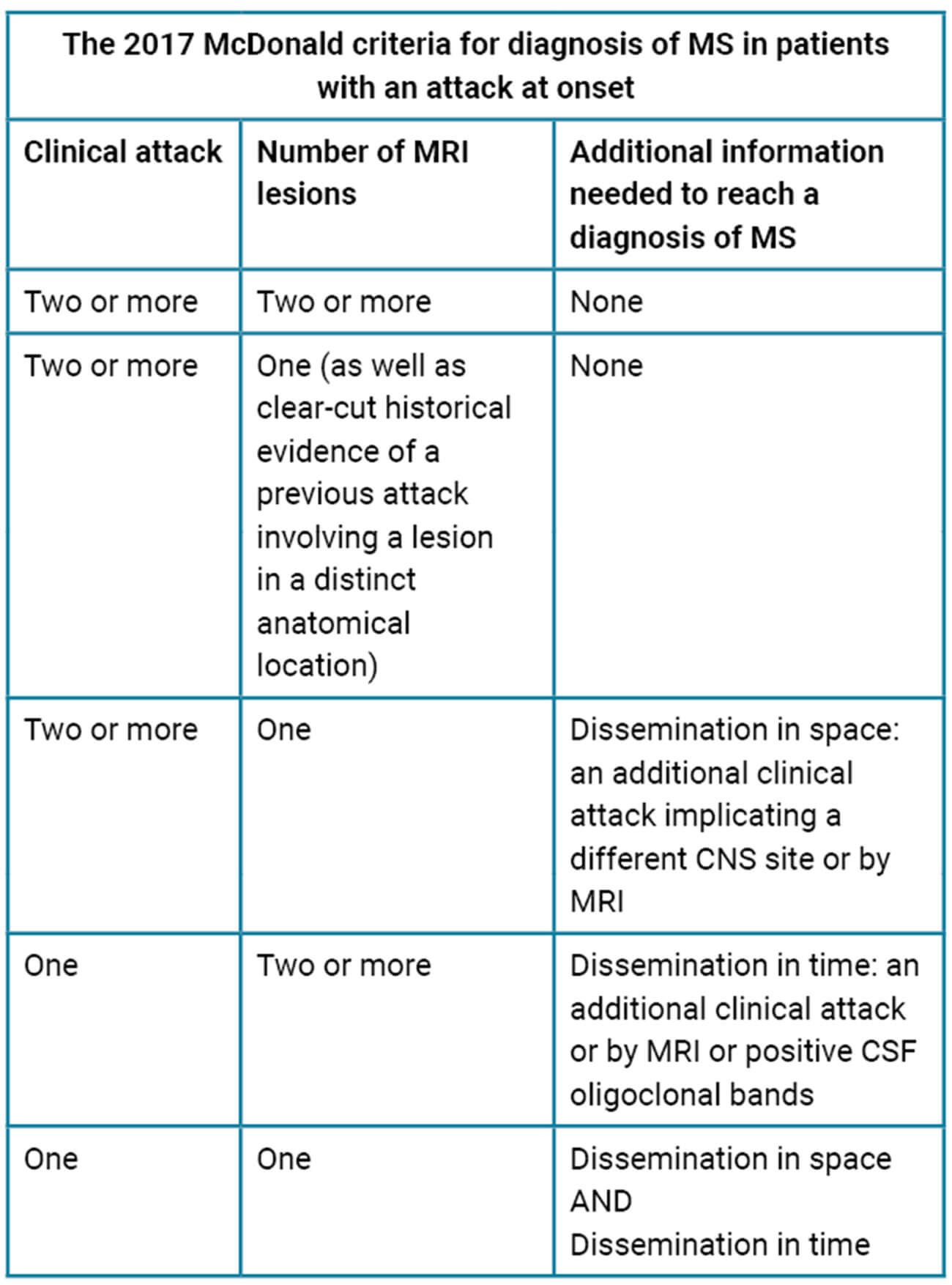
Table 4: McDonald criteria for MS diagnosis, adapted from Thompson, et al [3].
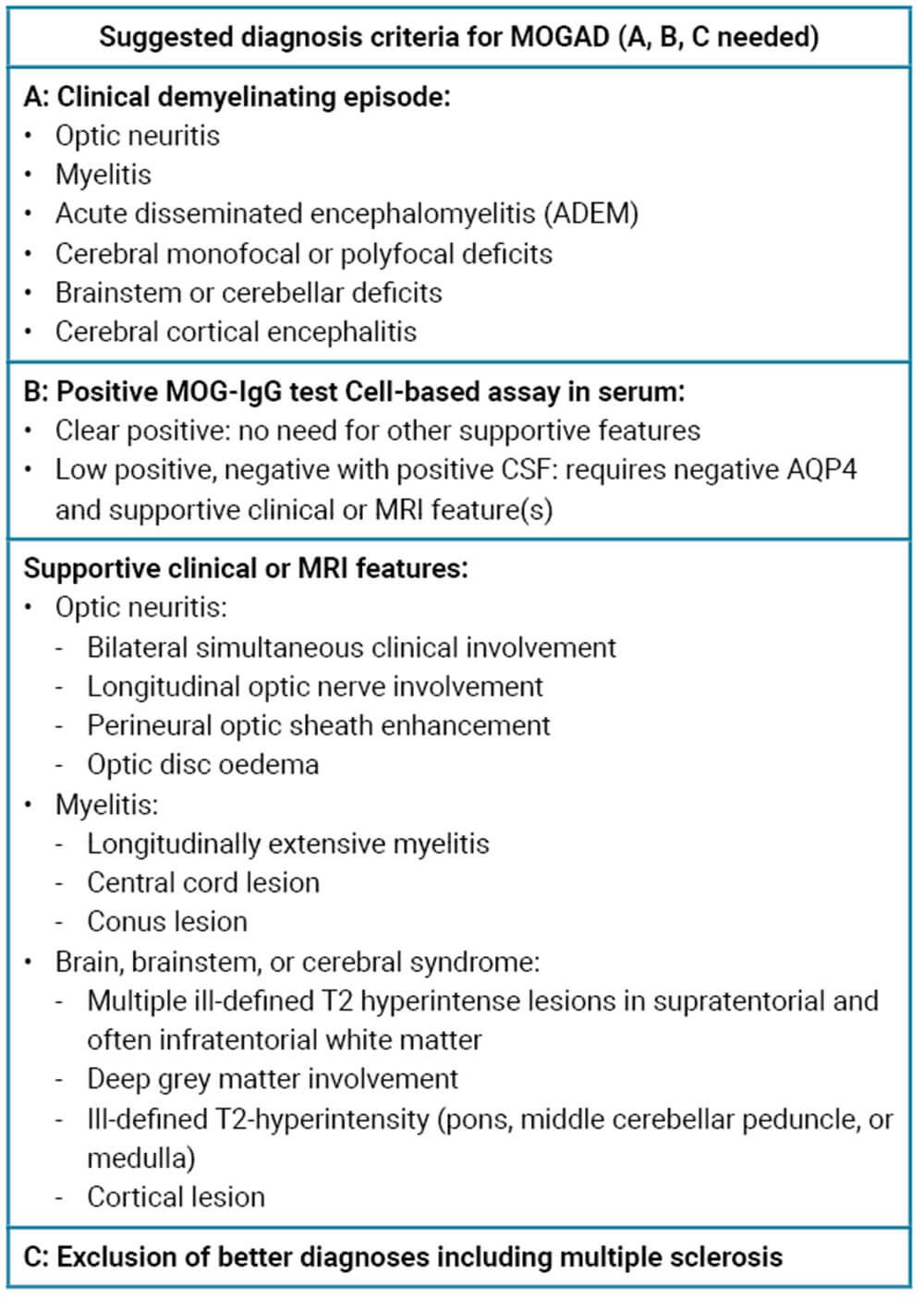
Table 5: Diagnosis criteria for MOGAD, adapted from Banwell, et al [4].
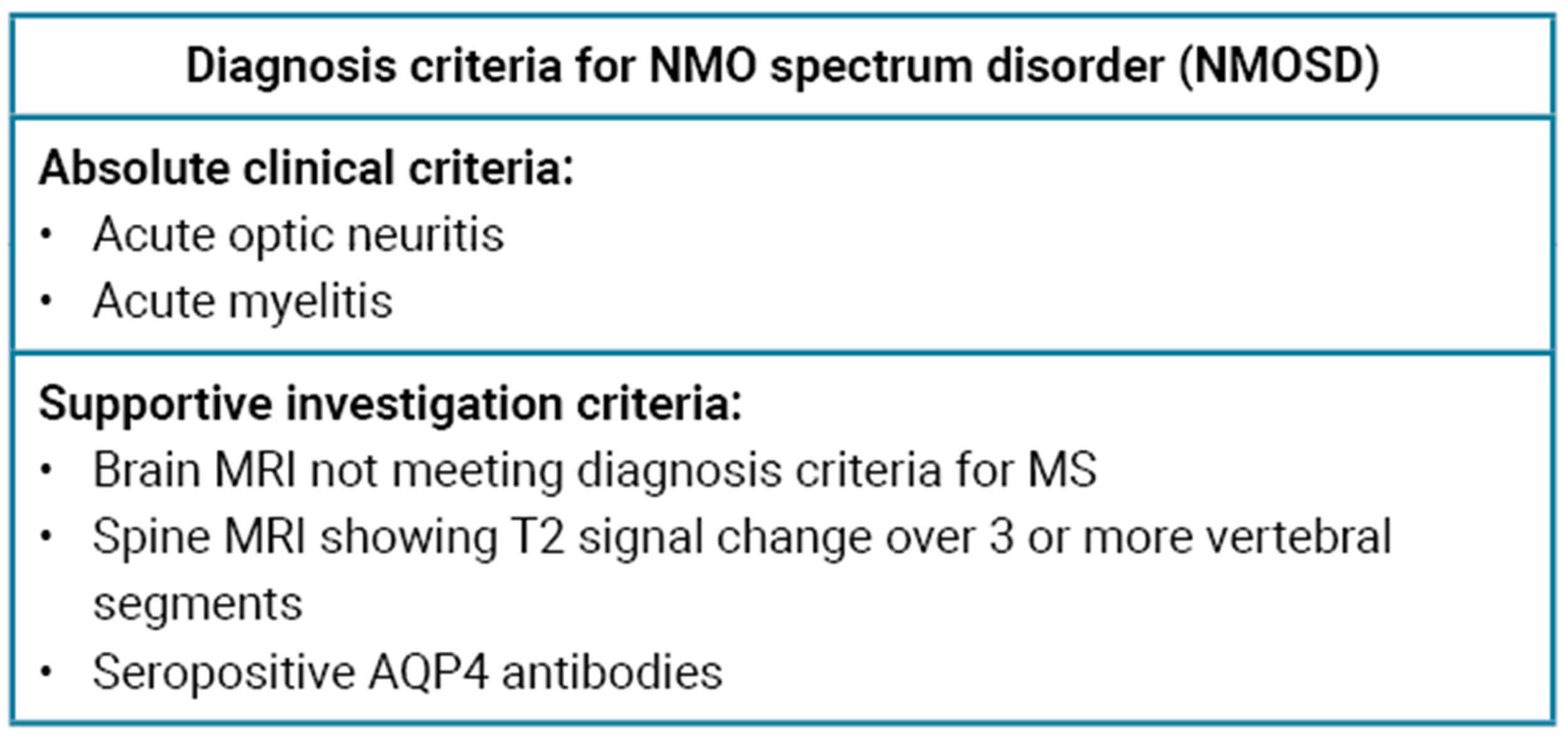
Table 6: Diagnosis criteria for NMOSD, adapted from Hoorbakht, et al [1].
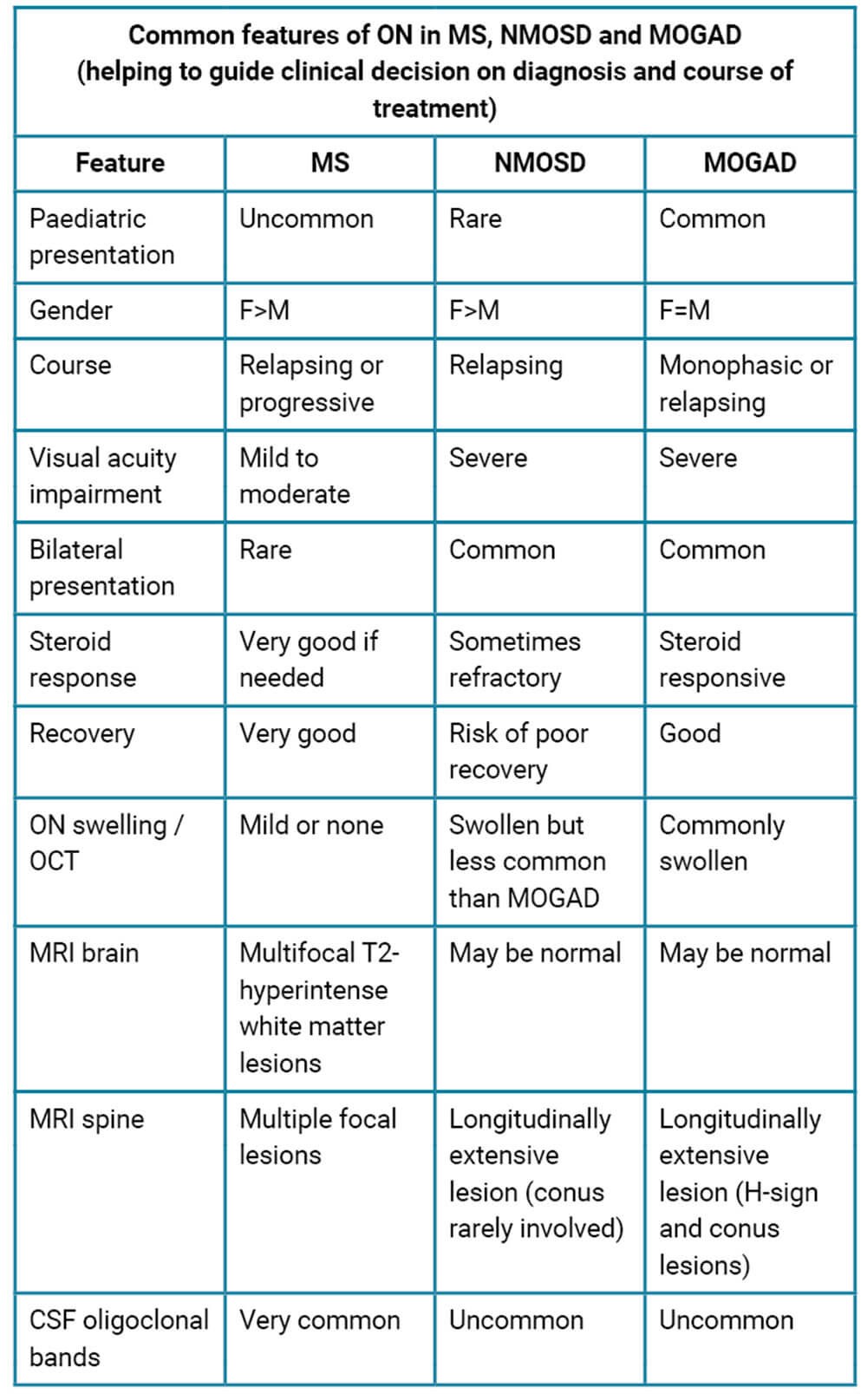
Table 7: Diagnosis criteria for NMOSD, adapted from Hoorbakht, et al [1] and Banwell, et al [4].
Treatment [1,2]
The optic nerve treatment trial (ONTT) is used as the gold standard guidance for treatment of optic neuritis. Most MS-related ON recover spontaneously, with recovery starting two to three weeks after onset and continuing for a year. The ONTT showed that intravenous methylprednisolone (IVMP) helped speed up the recovery of ON, but the final visual acuity was similar in treated and placebo given patients, although treatment group had better contrast sensitivity, colour vision and field tests than the placebo group. The ONTT also showed that the oral prednisolone group had a larger relapse rate compared to the IVMP group and the placebo group.
The current practice for treating suspected demyelinating optic neuritis varies between centres – the usual approach is to discuss with the patient the benefits and risks of steroid treatment and treat cases with severe visual loss with IVMP followed by oral prednisolone 60mg OD for 11 days and a short taper, based on the recommendations of the ONTT study. There are many discussions in the neuro ophthalmology societies about the limitations and the age of the ONTT study and the need for a new study to guide treatment, especially with more accurate assessments of visual functions and optic nerve structure via OCT scans. It is important to emphasise that MOGAD and NMO related ON are steroid responsive and early intervention with IVMP is crucial to preserve or improve visual functions.
There are many studies on the benefits of early treatment with immunosuppression for patients who are at high risk of developing MS. These include controlled high-risk subjects Avonex multiple sclerosis prevention study (CHAMPS), early treatment of MS study (ETOMS) and Betaferon in newly emerging multiple sclerosis for initial treatment (BENEFIT). They showed reduction of risk of developing MS with early treatment with disease modifying drugs (DMDs).
Conclusion
Optic neuritis is one of the most common optic neuropathies in young adults. In its most common form, it is caused by demyelination. It can be a feature of multiple sclerosis, neuro myelitis optica spectrum disorder or MOG-related disease. Early and accurate diagnosis is important, then depends on various clinical criteria as well as many investigations such as antibodies titres and neuro imaging. Treatment depends on the initial process and is currently guided by the ONTT study although there is a need for an up-to-date guidance.
References
1. Hoorbakht H, Bagherkashi F. Optic Neuritis, its Differential Diagnosis and Management. Open Ophthalmol J 2012;6:65-72.
2. Petzold A, Fraser CL, Abegg M, et al. Diagnosis and classification of optic neuritis. Lancet Neurol 2022;21:1120-34.
3. Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018;17(2):162-73.
4. Banwell B, Bennett JL, Marignier R, et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD Panel proposed criteria. Lancet Neurol 2023;22(3):268-82.
COMMENTS ARE WELCOME