Ophthalmology specialty trainees are required to pass the refraction certificate exam within the first two years of training. If one passes this exam before entering a training programme, this can add two points to the portfolio during applications. In this article, we will discuss the mistakes that most commonly occur during the refraction certificate exam which can easily be avoided if properly accounted for.
1. Running out of time
The commonest thing you hear exam candidates complain about is running out of time in the exam. This usually happens in the subjective sphere and subjective cylinder stations and less commonly with the retinoscopy stations. Subjective stations involve interacting with a patient and they usually take a bit more time to complete. If you have not been practising with a timer, time can truly fly when you enter the station, and you can find yourself unable to fill out all the answers at the end of it.
A good way to cut down on time is to consider the unaided visual acuity (VA) and have an expected prescription in your head before starting. For example: VA of 6/12 or +0.4 LogMAR should roughly have a mean equivalent sphere of 1D (each line being roughly 0.25). See Table 1 for more examples.
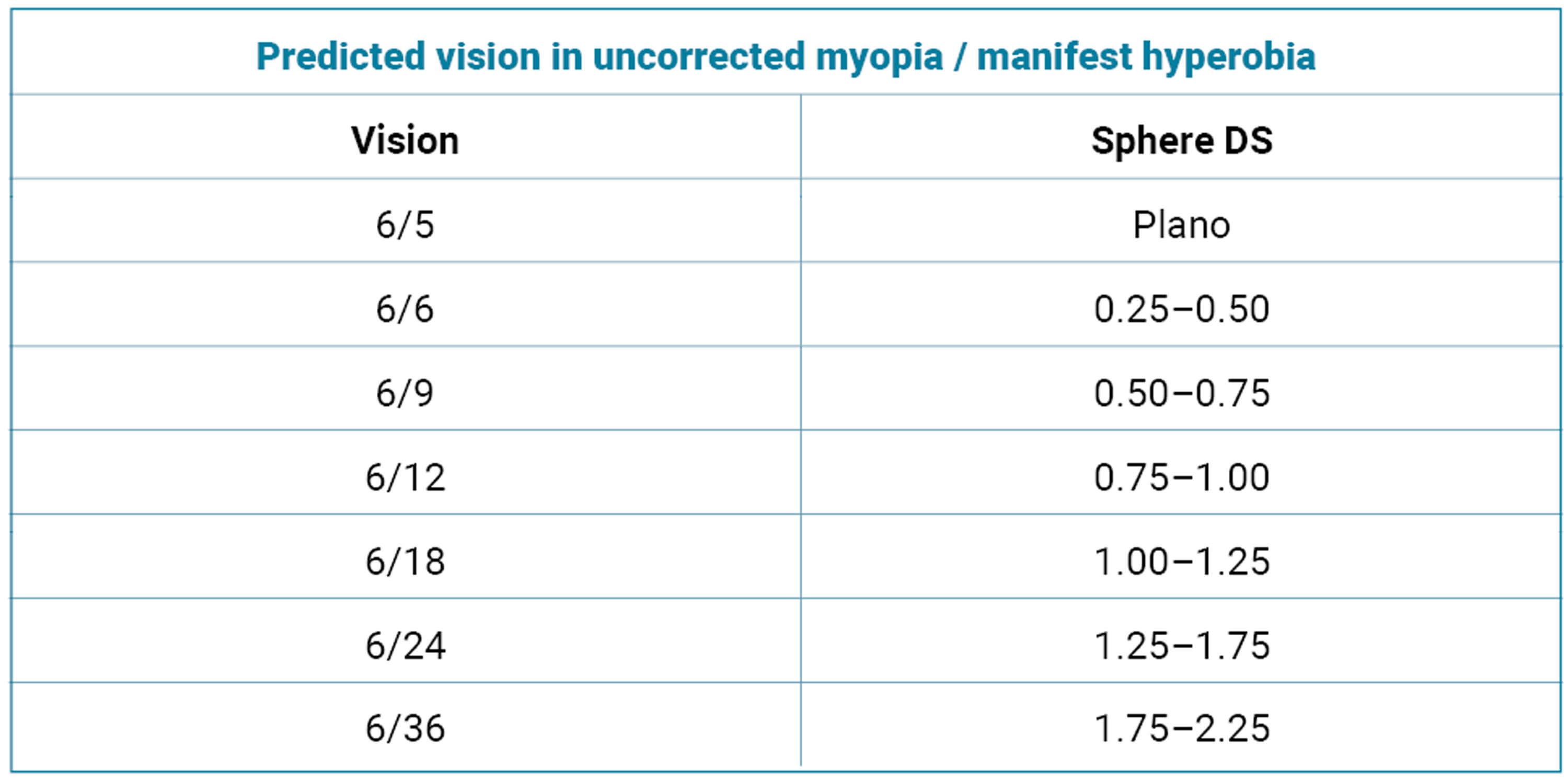
Table 1: Unaided vision and approximate refractive error.
Data sourced from https://www.opticianonline.net/cpd-archive/11 [2].
Another timewaster can be checking the VA repeatedly in the cross-cylinder station. This is not required and is only needed at the beginning and at the end of the station. Also, spending lots of time repeating the instructions to the patient is unnecessary as long as you are clear from the beginning.
Make sure you practise using the online iPad demo on the Royal College of Ophthalmologists’ website [1] for the refraction certificate exam, as it includes a built-in timer that updates every 15 seconds.
2. Small mathematical errors in retinoscopy
When you perform retinoscopy, the last step of the station is to remove your working distance from the lenses that you chose. When you’re in a high-pressure situation, small math errors can catch you out. Some candidates end up adding the working distance instead of removing it. Others mindlessly repeat the same values in both slots and fail to remove the working distance. After inserting the values, reread them to ensure they are correct. You might be surprised at how easy it is to miss such obvious mistakes which could cost you the whole exam. Please refer to Figure1 and Figure 2 for examples of how to correctly remove the working distance from plus and minus lenses.
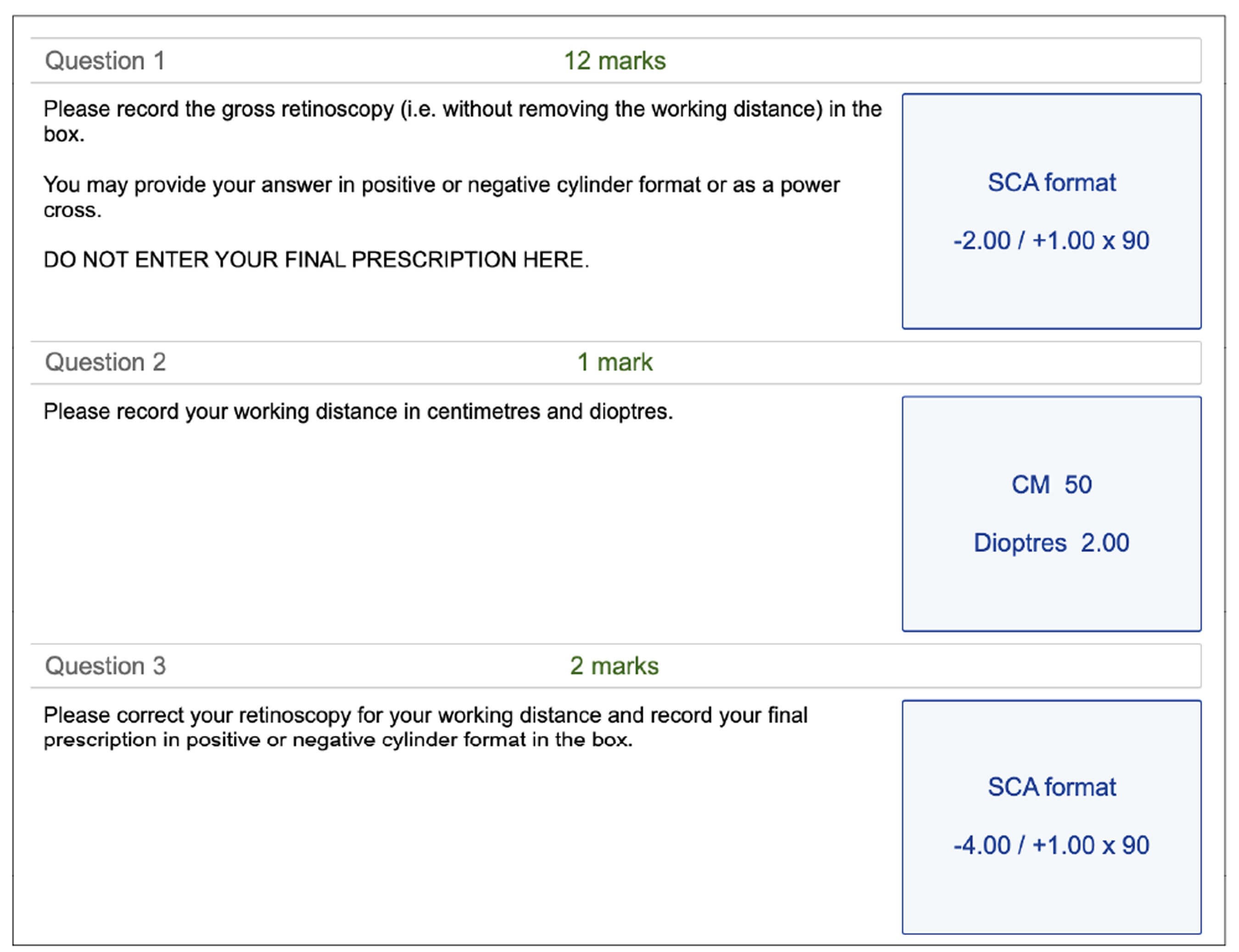
Figure 1: How to correctly remove the working distance with a minus prescription.
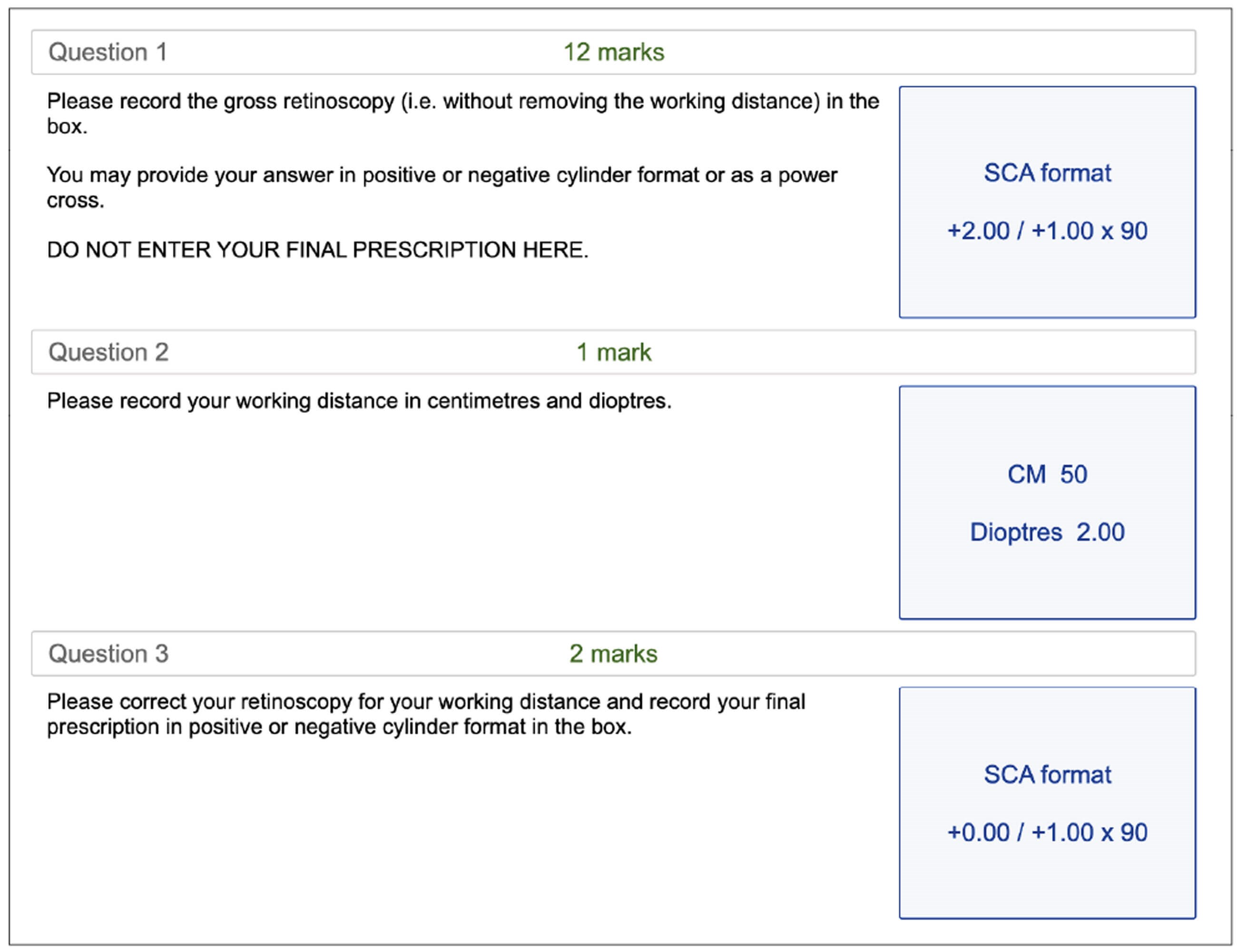
Figure 2: How to correctly remove the working distance with a plus prescription.
3. Over-plus the patient
During sphere refinement, we usually try to push the plus lens as much as possible. We generally ask the patient if they can see better with the lens, the same, or better without. On more than one occasion, there have been patients that say that they prefer the plus lens, or that it was the same, but when the lens was added their VA gets worse. Make sure you check if the patient can read more letters, or at least the same letters, before adding plus to the prescription.
4. Over-minus the patient
When showing the patient a minus lens, let them know that you will only show it for a short period of time, and make sure the lens doesn’t linger in front of the eye so that they don’t accommodate. Patients love minus lenses and will generally say that they can see better with it, but it is up to you to ask if they can read any more letters with this lens or if the letters are just darker and bolder. If they can’t read any extra letters, do not add the minus lens and leave it as it is.
5. Inefficiency when checking for prism in the focimetry station
During the focimetry station, you could be given a lens with a vertical prism (less likely to be a horizontal prism in the exam). There is a good chance that it will also be a bifocal lens, meaning you’ll have to push the glasses up to measure the near addition. If you start on the left lens, make sure that you check the right lens for any vertical prism before you check the near addition on either lens. Checking for the near addition would require you to push the spectacle table up, altering the vertical plane and not allowing you to check for prism without readjusting – so, checking the prism first could be more efficient.
6. Changing your working distance during retinoscopy
In the retinoscopy stations, make sure that you keep your working distance consistent. Shifting your position (whether closer or further away from the patient) will alter your working distance and make your sphere measurements inaccurate. When practising retinoscopy, make sure whoever is helping you occasionally steps in and measures your working distance to make sure it is consistent. It is also useful to have a measure of the distance which you can check. For example, your shoulder to wrist is around your working distance, so you can hold up your arm to make sure you are approximately in the right place.
7. Not being on axis for retinoscopy
Take time to ensure that you are aligned with the patient to avoid inaccurate cylinder measurements. Being off axis can give rise to misleading retinoscopy reflexes that lead to an inaccurate result. Move your chair height up and down accordingly so that retinoscopy is completed on the visual axis. Remember to use your right eye to patient’s right eye and left eye to left eye.
8. Confusing plus and minus in the subjective cylinder station
In the subjective cylinder station, many candidates turn the axis the wrong direction initially (candidates should make sure to check the plus and minus on the cross cylinder and take a second to think which way the axis needs turning). They often also change the power the wrong way initially, again just an error confusing plus and minus. This usually comes down to nerves on the day and can be avoided by taking a moment before the station starts to ground yourself and properly inspect your equipment.
Conclusion
Knowing the commonest mistakes in the refraction certificate exam beforehand could help you train to avoid them. They usually occur because of inadequate practise and nerves on the day, both of which can be managed by spending more time practising in order to improve your efficiency and confidence. Also, taking a second during the exam to think of the next step or review your answers can save you a few points and prevent failing because of trivial errors.
We would like to thank the the optometry department at the Manchester Royal Eye Hospital for their help with this article. Hopefully this has been helpful to you and good luck to anyone sitting the exam.
References
1. Refraction Certificate Examination [practice]. The Royal College of Ophthalmologists.
https://ripleyhosting.co.uk/fmi/
webd/RCOphth_Web?homeurl=
2. C35930 Elements of refraction - part 3, Optician.
https://www.opticianonline.net/
cpd-archive/11
[All links last accessed January 2024]
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME











