Case presentation
A 50-year-old female presented to eye casualty with a lump on the left medial lower eyelid with associated redness and occasional bleeding. The lump was present for a few months with recent enlargement (Figure 1). Her past medical history included blepharitis and bilateral periocular and facial eczema-related changes.
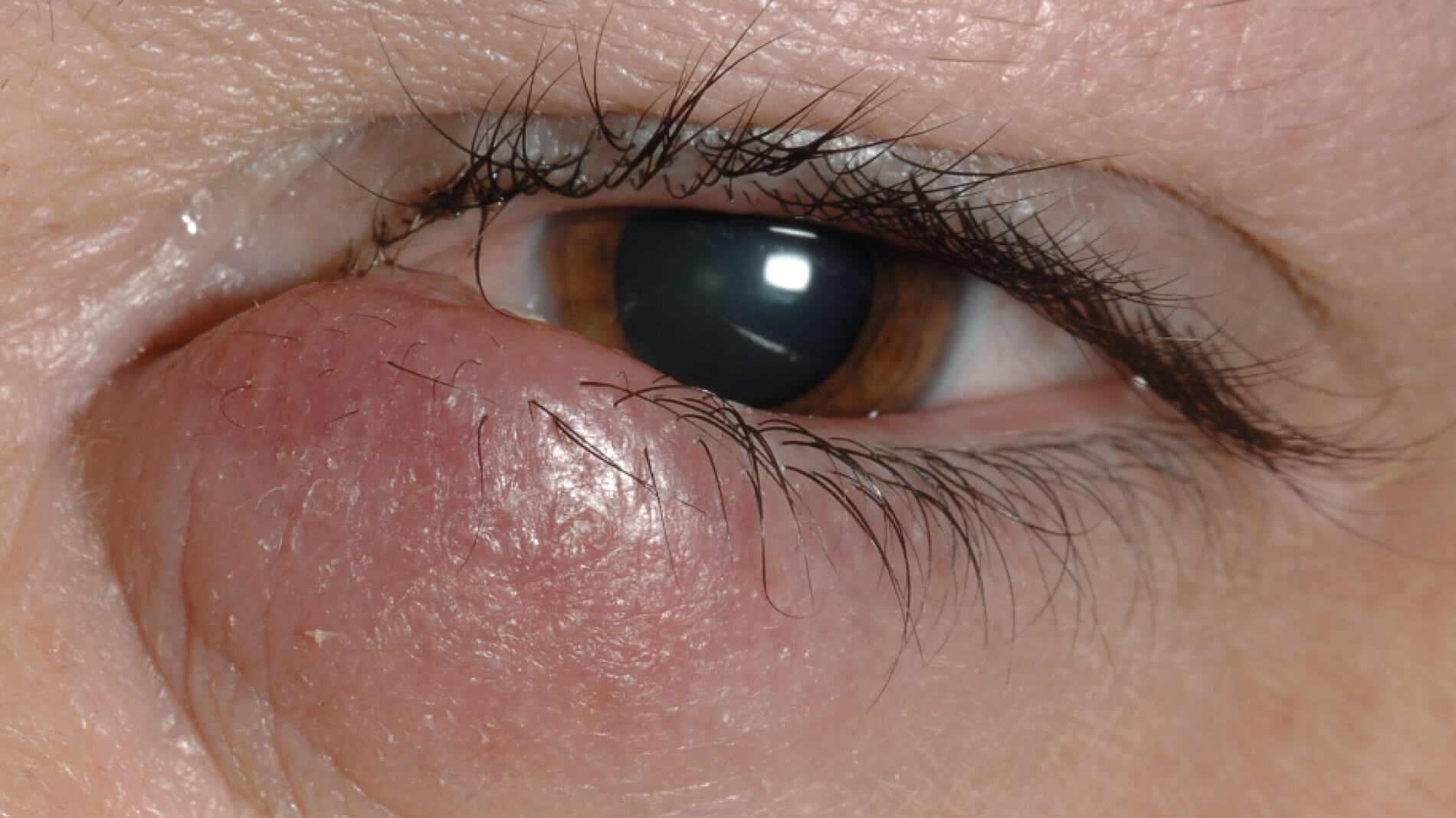
Figure 1: A 50-year-old female with a medial lower lid lump.
There was a history of previous hospitalisation due to severe eczema and she continued to require intermittent Betnovate steroid cream. She was presumed to have an acute internal hordeolum and advised to perform lid hygiene and antibiotic eye drops were prescribed. Safety-net advice was given to call eye casualty in case her symptoms persisted.

Figure 2: Learning pearl; always check the fornices and evert
the upper eyelid when examining the anterior segment.
A month later the patient called eye casualty reporting that her lump was larger despite performing lid hygiene and taking a course of oral antibiotics from her GP. An urgent incision and curettage of the suspected chalazion was arranged within two weeks. Upon incision no significant exudate was found from the large solid lump (Figure 2). Given the suspicion of a sebaceous gland carcinoma (SGC) an incisional biopsy of the left lower tarsal conjunctiva was performed. Two specimens were sent; one in formalin and one as fresh tissue (fresh tissue historically was required for lipid stains such as Oil Red O if SGC was suspected; but this is no longer required with the advances in immunohistochemistry).
Histology report
Histology report showed a moderately differentiated keratinising invasive squamous cell carcinoma (SCC) of the conjunctiva. A CT head, neck & orbits scan with contrast was performed which confirmed the presence of an inferior left conjunctival soft tissue mass with no evidence of orbital involvement, intracranial metastatic disease or lymph node metastasis. Staging CT chest, abdomen and pelvis was clear.
She was referred to the Sheffield ocular oncology service where she underwent conjunctival mapping biopsies. This was followed by a multi-staged excision of lesion and reconstruction with a Hughes flap and a fornix bolster. Cryotherapy was also applied to the mapping biopsy proven in situ bulbar conjunctival areas.
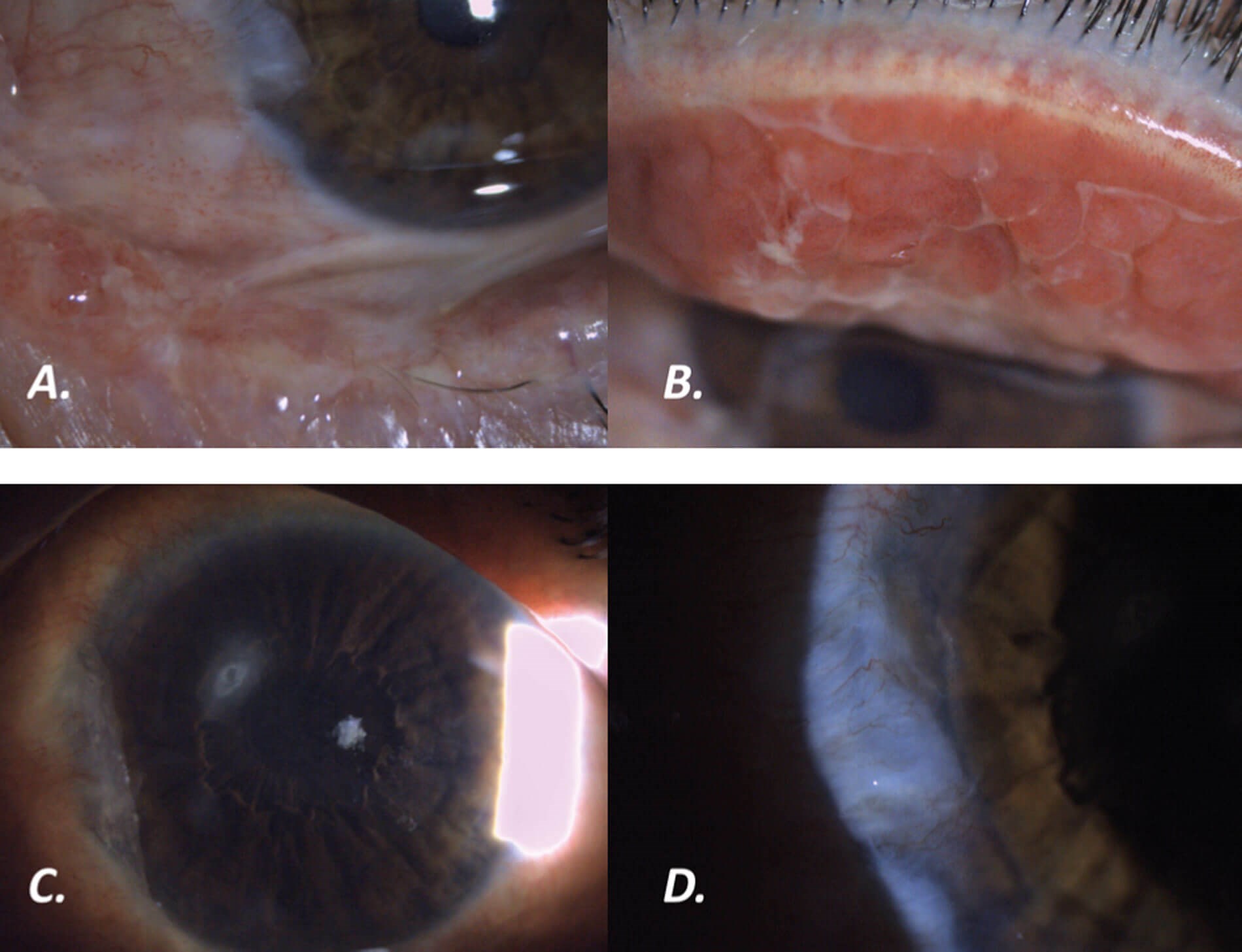
Figure 3: (A) Lower lid symblepharon; (B) Upper eyelid giant papillae; (C) Superior mid-peripheral
corneal ulcer; (D) Suspected squamous cell carcinoma of the nasal conjunctiva.
Two months later the patient re-attended eye casualty with a left eye discomfort and irritation. Examination revealed progressive granulation like tissue on the lid margin with no significant symblepharon or upper lid change. Urgent re-biopsy was performed, which revealed severe dysplasia but no invasive neoplasia. A few weeks later she developed pain and reduced vision. On examination there was a significant symblepharon inferiorly, an upper tarsal giant papillary conjunctivitis and a superior mid-peripheral corneal ulcer with a suspected area of SCC recurrence at the nasal conjunctiva (Figure 3). After discussion with the Sheffield team further mapping biopsies were taken from the conjunctiva of all four quadrants, upper and lower fornices, and the upper lid papillae. A repeat MRI scan with contrast of the neck & orbits scan was normal. The patient was treated with a course of ofloxacin eye drops and the corneal ulcer responded favourably.
The conjunctival mapping biopsies from the left inferotemporal bulbar conjunctiva, inferior fornix and inferonasal conjunctiva all confirmed evidence of residual in-situ squamous cell carcinoma. The upper lid biopsies did not show anything sinister. This was treated with topical chemotherapy with Mitomycin 0.04% eye drops, four times a day to her left eye for one week (one cycle) for four cycles delivered over eight weeks along with dexamethasone 0.1% preservative-free eye drops for eight weeks. The patient is being monitored closely and remains stable. Six-monthly neck ultrasound was recommended for the next five years to ensure that there is no lymph node metastasis.
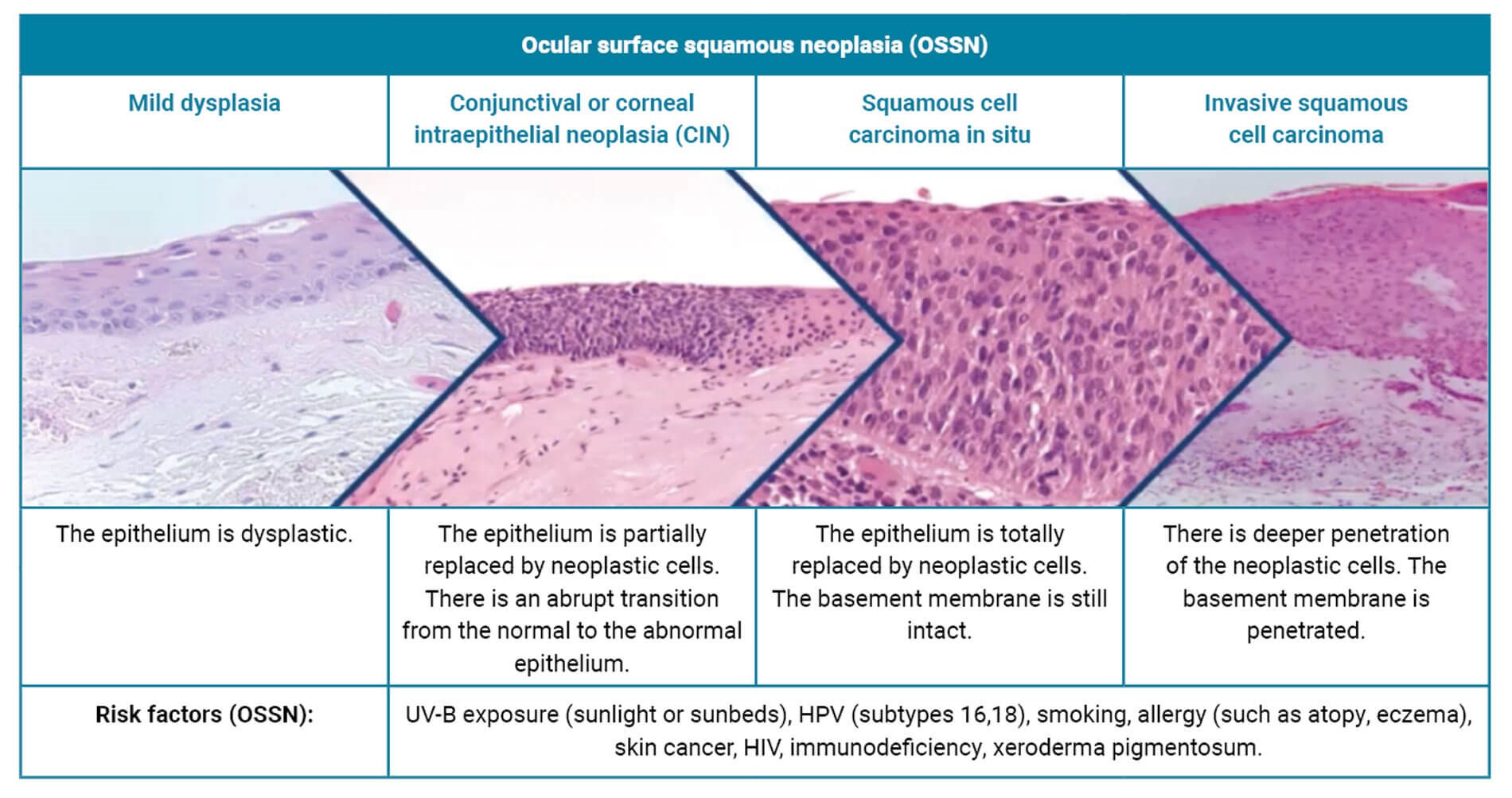
Table 1: Ocular Surface Squamous Neoplasia (OSSN) and risk factors [1].
Ocular surface squamous neoplasia
OSSN encompasses mild dysplasia, conjunctival or corneal intraepithelial neoplasia (CIN), SCC in situ, and invasive SCC (Table 1). The risk factors are multiple and these are also shown in Table 1. OSSN is the most common non-pigmented tumour of the conjunctiva. Most cases occur on the bulbar conjunctiva. Conjunctival SCC is less aggressive than conjunctival melanoma and metastasises less frequently. However, it is still important to palpate the pre-auricular and sub-mandibular lymph nodes, through which the lymphatic drainage of the conjunctiva drains.
Clinically we should ascertain the position of the suspected lesion, whether there are any feeder vessels and whether the lesion is movable. Rose bengal or lissamine green dyes can be useful because they stain OSSN but not the conjunctival melanoma, however they are not widely available in many units. Although OSSN is more common in older white men, it can present in young people, too. If it presents at a young age then we should enquire for any underlying risk factors and specifically for immunosuppression such as HIV.
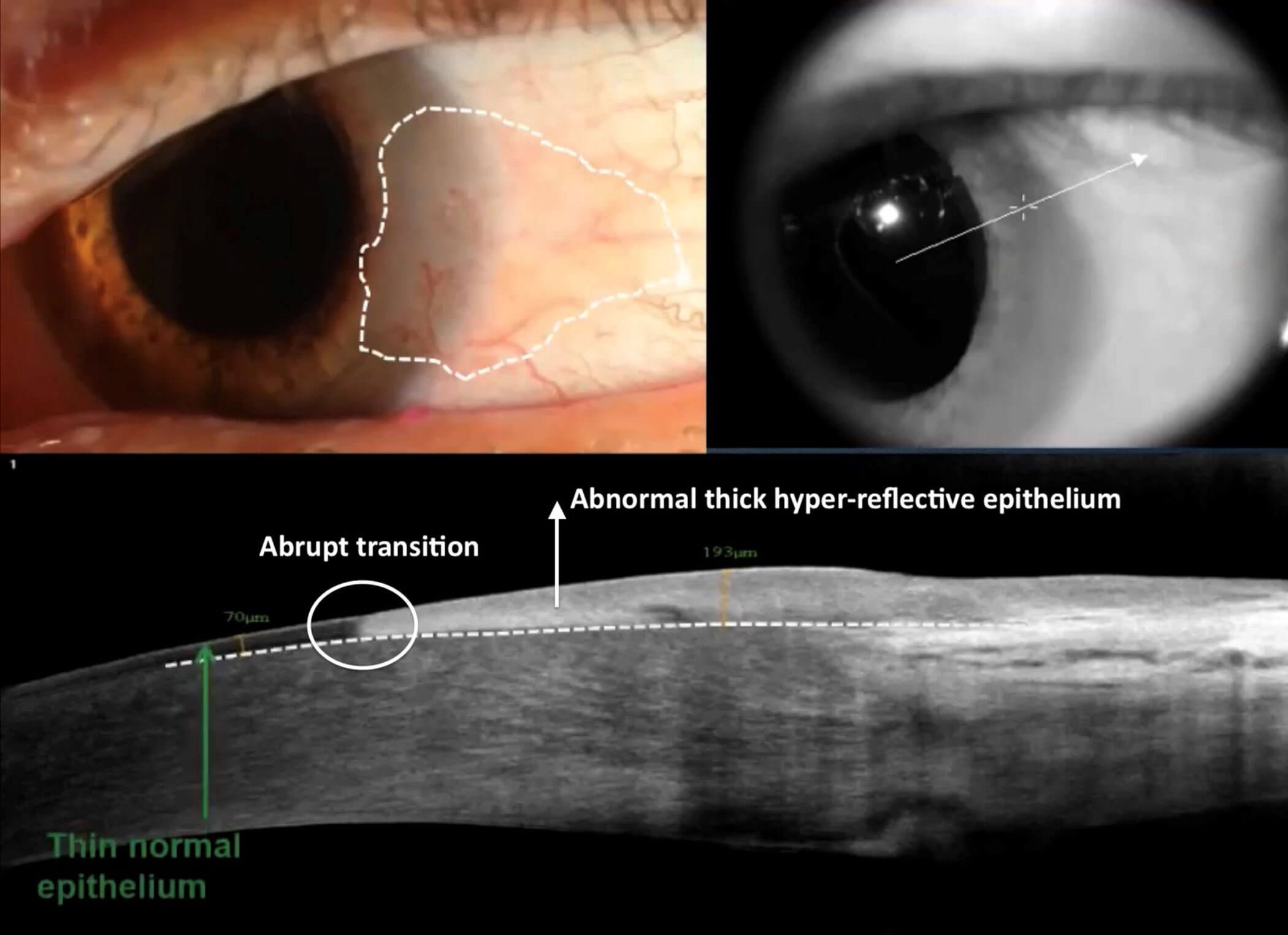
Figure 4: High-resolution OCT of a suspicious lesion at the nasal conjunctiva. Clinically the borders of the lesion are not well defined. The epithelium is thickened (193μm) and there is an abrupt transition from the normal to the abnormal epithelium. The amount of thickened epithelium is also important in differentiating the lesion. The features are highly suggestive of OSSN. Photo courtesy of Dr Carol Karp [2,3].
Diagnosis
The gold standard of diagnosis is biopsy. A high-resolution optical coherence tomography (OCT) of the anterior segment can be helpful in bulbar conjunctival disease. It can help to differentiate between epithelial lesions and sub-epithelial lesions. OSSN is epithelial whereas conjunctival melanoma (which is rarely non-pigmented) is sub-epithelial (Figure 4). HS-OCT can also be used to check the response to treatment and whether there is any evidence of recurrence of the lesion.
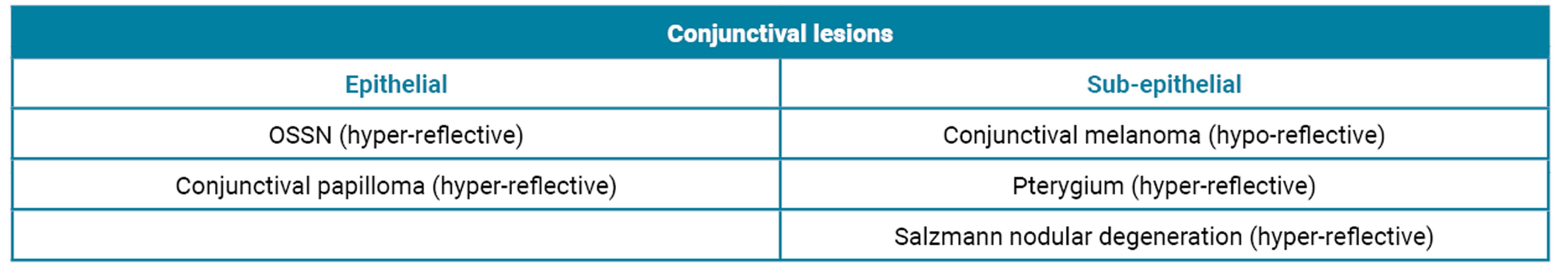
Table 2: Examples of epithelial and sub-epithelial conjunctival lesions with their associated OCT reflectivity.
In addition, HS-OCT can provide us with information as to whether the lesion is hyper-reflective or hypo-reflective, which is helpful in the differential diagnosis (Table 2). Despite the recent advances and usefulness of the HS-OCT we should be mindful that in terms of diagnosis the biopsy is still the gold standard.
Biopsy
Biopsy of suspected OSSN can be incisional or excisional. However, if melanoma is suspected, incisional biopsy should never be performed as it has the potential to cause local or distant spread. Mapping biopsies of conjunctiva is often required to ascertain extent of involvement.
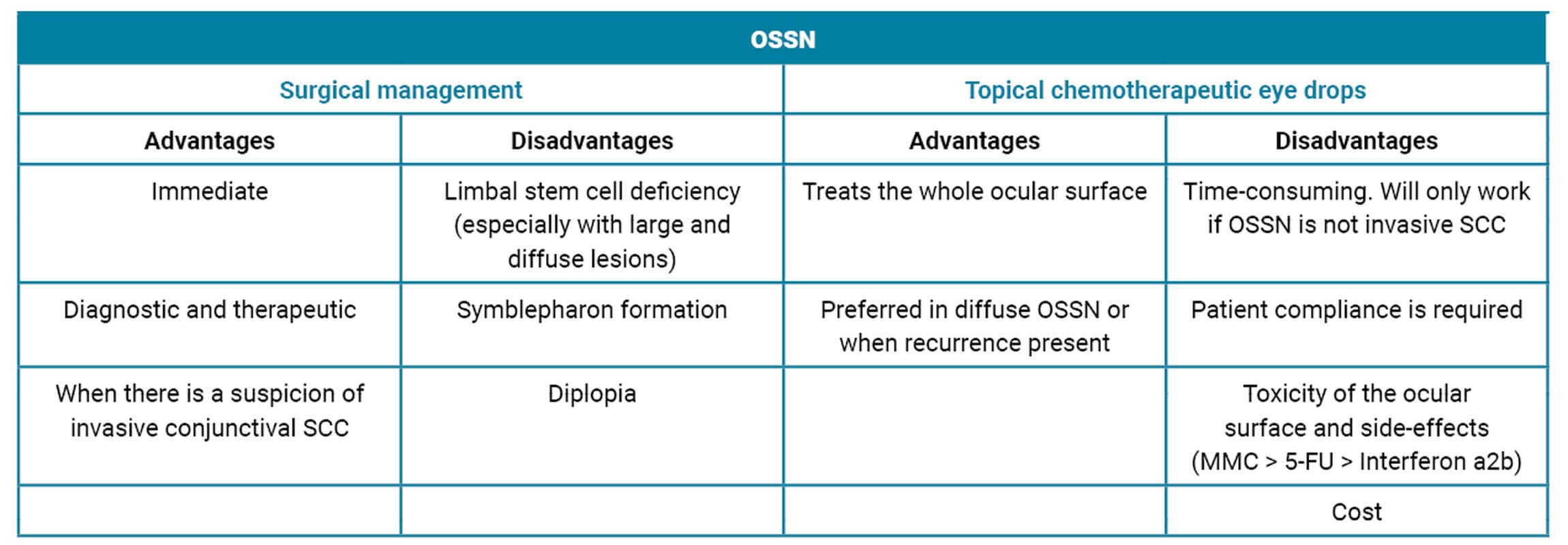
Table 3: Advantages and disadvantages of OSSN management;
surgical versus topical chemotherapeutic eye drops [6,7].
Treatment
OSSN can be treated with surgery, or topical chemotherapeutic eye drops such as Mitomycin-C (MMC), 5-Fluorouracil (5-FU) and topical immunotherapy drops such as interferon a2b [4]. The choice of surgery over topical treatment for OSSN needs to be individualised and the pros and cons are shown in Table 3. If surgery is to be performed then an excisional biopsy with a ‘no-touch’ technique is the treatment of choice with a 3–4mm margin combined with cryotherapy to the conjunctival edges [5]. OSSN has a high risk of recurrence and can be bilateral hence close monitoring of patient is essential and patients often require multiple treatments.
Conclusion
A systemic approach when encountering a patient with a suspicious conjunctival lesion is the key to making the correct diagnosis. Ensure that both eyes are thoroughly examined and that the upper lids are everted. Biopsy of the lesion remains the gold standard in terms of diagnosis. Mapping biopsies of conjunctiva is often necessary. Topical chemotherapeutic eye drops are becoming more popular as an alternative to surgical management with very promising outcomes, especially in diffuse OSSN or in OSSN recurrence. However, with invasive SCC lesions such as this one, surgical treatment is important to achieve disease control.
TAKE HOME MESSAGES
-
Conjunctival OSSN / SGC’s are great mimimickers and need to be kept in mind for unusual looking lumps on the inner aspect of the eyelid (like this patient’s presumed internal hordeolum).
-
In OSSN, incisional biopsy of lesion and mapping biopsy of conjunctival surface is necessary to decide management plan.
-
OSSN is only a clinical diagnosis at presentation as this is a spectrum from mildly precancerous to severely precancerous to frankly invasive disease, biopsy is essential for final diagnosis and management plan.
-
Trigger factors need to be looked into like HIV / immunosuppressant, etc.
-
Invasive SCC will need full body staging and management with wide local excision.
-
Non invasive OSSN management varies between cryotherapy, intralesional injections / topical chemotherapy with MMC / 5FU etc to surgical removal.
-
Often multi-modality treatment is necessary including surgery, cryo, topical chemo as in our patient.
-
OSSN has a high risk of recurrence hence patients need monitoring long term.
References
1. Eagle R. Ocular Oncology. WillsEye Hospital.
https://www.willseye.org/medical-services/
subspecialty-services/ocular-pathology
2. Kieval JZ, Karp CL, Abou Shousha M, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology 2012;119(3):481–6.
3. Carol Karp M. Ocular Surface Squamous Neoplasia Lecture - Carol Karp, MD. Oftalmo University [video] (May 2020).
https://www.youtube.com/
watch?v=4MjiJIi6hK0
4. Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol 2013;24(4):336–42.
5. Chang V BV, Wells J, Gurnani B. Ocular Surface Squamous Neoplasia (2023). EyeWiki.
https://eyewiki.org/Ocular_Surface
_Squamous_Neoplasia
6. Nanji AA, Moon CS, Galor A, et al. Surgical versus medical treatment of ocular surface squamous neoplasia: a comparison of recurrences and complications. Ophthalmology 2014;121(5):994–1000.
7. Alvarez OP, Zein M, Galor A, Karp CL. Management of ocular surface squamous neoplasia: Bowman Club Lecture 2021. BMJ Open Ophthalmol 2021;6(1):e000842.
[All links last accessed January 2024]
Acknowledgements: We would like to thank the patient for allowing the publication of their story. We would also like to thank Steve Slater, Lead Ophthalmic Photographer and his team at the Royal Eye Infirmary, University Hospitals Plymouth for the excellent photos.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME








