See also Simulated ocular surgery and Simulated ocular surgery: pars plane vitrectomy and scleral buckling surgery
Strabismus surgery requires a range of skills, distinct to those required for intraocular surgery. Even if a trainee does not plan to become a strabismus surgeon the tissue handling, dissection and scleral and rectus muscle suturing skills, which are integral to strabismus surgery, will benefit the budding glaucoma, vitreoretinal and oculoplastic surgeon. They will also enhance a surgeon’s ability to mange complex penetrating eye injuries, which may involve the sclera and extraocular muscles.
The aim of this article is to describe strategies for teaching different types of strabismus surgery using model eyes and / or cadaver material.
Simulation material
1) Model eyes – There are two types of simulated ocular surgery strabismus (SOS) eyes designed by Philips Studio:
a) The basic strabismus eye (Figure 1) has no conjunctiva nor Tenon’s capsule. It has four rectus muscles but has no oblique muscles. The globe is hollow, the sclera which is 0.5m thick, has been made out of a material that has the same resistance to a needle pass as human sclera and has a similar tensile strength, so sutures will not cut out of the sclera. The rectus muscles are the same dimensions and have a similar feel to a needle pass as real rectus muscles.

Figure 1: The basic strabismus eye.
b) The advanced eyes (Figure 2) have the same scleral shell and rectus muscles, but they also have a layer of conjunctiva, with similar elastic properties of human conjunctiva, a layer of Tenon’s capsule and a superior or an inferior oblique muscle. The superior oblique tendon is made from a thin stretchy material that has a wide insertion under the superior rectus as in life. The inferior oblique tendon is more cord-like as it is in life (Figure 3). Both eyes sit in a mounting cup, which is placed in a model head.

Figure 2: The advanced eye.

Figure 3: The inferior oblique tendon.
2) Cadaver material – Freshly defrosted cadaver material (stored at -18°C) or lightly embalmed cadaver material (popularised by Jim Innes in Hull) is perhaps the gold standard material for strabismus surgery simulation. These preservation techniques retain the elasticity of the conjunctiva and extraocular muscles, unlikely the formalin preparations. Once the eyes are inflated to a normal pressure using silicone oil injected in the vitreous cavity, they can be used to simulate any type of strabismus surgery (Figure 4). However, the major draw back of the cadaver material is that its use is restricted to one of wet-lab courses and so it does not lend itself to sustained deliberate practise.
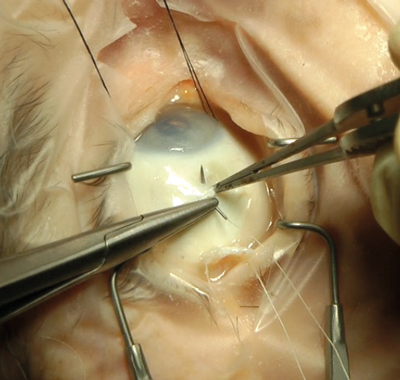
Figure 4: Cadaver eye.
However, for more experienced surgeons wanting to learn techniques such as superior oblique tucks, Harada-Ito procedures (Figure 5), transpositions or posterior fixation sutures it is the ideal material.

Figure 5: Harada-Ito procedures on a cadaver eye.
Simulation techniques
We use the basic eyes for practising scleral suturing, knot tying and rectus muscle suturing, letting the trainee get a feel for the tissues and allowing them to build up their confidence with these manoeuvres. The following is the step-wise training program published in the curriculum section of the RCOphth website:
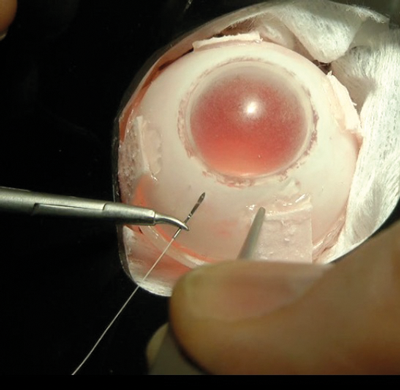
Figure 6: Basic suturing technique.
1) Basic scleral and muscle suturing
- The trainee observes the correct techniques either by watching their consultant operate, or by watching a video of techniques on the SOS website, or a strabismus DVD atlas.
- 10 minute tutorial with trainer to make sure the correct instrument handling and basic suturing techniques (as taught on the RCOphth Microsurgical Skills course) are sound (Figure 6). The trainee can then take the head and basic strabismus eyes home to practise.
- The trainer can then assess their progress using the SOS Ophthalmic Simulated Surgery Competency Assessment Rubic (OSSCAR).
Once a trainee has mastered these techniques they can move on to practise recession and resection techniques.

Figure 7: Disinserting the muscle.
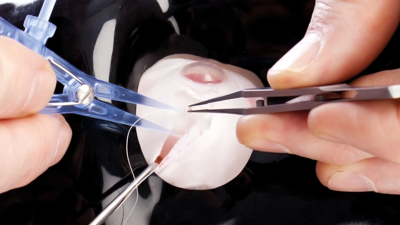
Figure 8: Measuring the recession point accurately.
2) Recession and resection techniques
- Observe correct techniques either by watching a consultant operating, or watching a video of techniques on the SOS website or a strabismus DVD atlas.
- 30 minutes of supervised instruction followed by solo practise.
- Use the SOS OSSCAR to determine level of competence and then move to practise the same steps of the operation on the advanced strabismus eyes with conjunctiva and Tenon’s capsule dissection and closure. All of the following steps can be simulated using the advanced model eyes.
- Opening the conjunctiva – via a limbal or fornix based approach. Dissecting through Tenon’s capsule and identifying the rectus muscle.
- Hooking the muscle.
- Cleaning off the Tenon’s capsule.
- Suturing the muscle for a recession or resection, but this time having to negotiate the conjunctiva and Tenon’s. Again the technique can vary using continuous or interrupted sutures, with a fixed or non-fixed hangback technique.
- Disinserting the muscle (Figure 7).
- Measuring the recession point accurately (Figure 8).
- Resuturing the muscle to the globe.
- Closing the conjunctiva.
Like cataract surgery we build up to performing a whole operation by breaking down the procedure into blocks of two to three steps and when a trainee is achieving a competent level for these blocks we allow them to perform the same stages of the procedure on our patients. As their confidence and competence grows they string together more stages of the operation until they can perform the complete procedure.
The other important skill that can be taught using simulation is the art of being a good surgical assistant. Knowing how to create good exposure of the surgical site, how to hold squint hooks correctly so that your hands are not getting in the way of the principle surgeon.
There is a misconception that simulation training requires intensive supervision by the trainer. However, the level of supervision suggested by the RCOphth can, in my experience, be easily fitted in between cases during an operating list or at the end of the theatre list.
Adjustable suture techniques
The technical aspects of adjustable suture strabismus surgery can be taught using these simulation methods, i.e. how to tie an adjustable knot and how to advance or recess the muscle. However, with a little bit of imagination simulation can be made very much more ‘life-like’. All experienced strabismus surgeons will have encountered unexpected difficulties whilst trying to carry out postoperative adjustments, such as the adjustable knot becoming fixed, the suture breaking or snagging on Tenon’s capsule, or the patient becoming distressed during the adjustment process. All of these problems can be simulated using the model eyes by tampering with the knot or intentionally fraying the suture to weaken it, or simply by shaking the head and adding a few sound effects during the adjustment! Of course the trainee should not be told beforehand what is going to happen, so adding to the drama! Other intraoperative mishaps such as a ‘lost’ or slipped muscle can also be simulated, by putting traction on the appropriate muscle (Figure 9).

Figure 9: Intraoperative mishaps can be simulated by putting traction on the appropriate muscle.
Inferior oblique and superior oblique surgery
Both SOS model eyes and cadaver material can be used to simulate inferior oblique recessions (Figure 10) or myectomies and a range of superior oblique surgery including tucks, Harada-Ito procedures and posterior tenotomies. The same principle of becoming competent with each stage of the procedure before proceeding to live surgery also applies to these techniques.
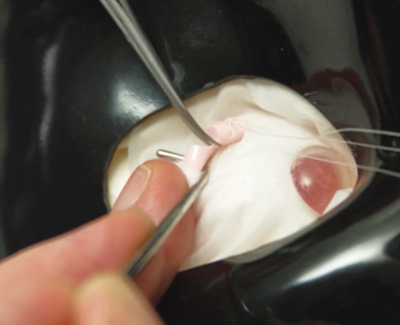
Figure 10: Simulating inferior oblique recessions.
Where to from here?
The simulated ocular surgery model eyes have been used in surgical workshops at the World Congress of Paediatric Ophthalmology and Strabismus in Milan in 2012 and Barcelona in 2015 and at AAPOS in 2013 and are now being used in teaching programs across the globe.
Studies to determine the construct and predictive validity of the SOS models are currently underway in the UK. The first validation study of the model eyes was published in JAAPOS in February 2015, which showed that residents’ comfort level with strabismus surgery statistically improved with a structured simulation curriculum using the model eyes [1].
Historically, strabismus surgery was frequently delegated to the most junior member of the surgical team, whilst the registrar and consultant got on with the ‘serious business’ of cataract surgery! Thankfully as these simulation techniques become embedded into curricula across the globe, attitudes towards how strabismus surgery should be taught are changing and this can only be of benefit to our patients and our trainees.
All of the simulation techniques described in this series of articles can be found on the Simulated Ocular Surgery website www.simulatedocularsurgery.com.
Reference
1. Gertsch KR, Kitzmann A, Larson SA, et al. Description and validation of a structured simulation curriculum for strabismus surgery. J AAPOS 2015;19(1):3-5.
Declaration of competing interests: John Ferris designed and owns the Simulated Ocular Surgery website.
COMMENTS ARE WELCOME





