See also Simulated ocular surgery - strabismus surgery and Simulated ocular surgery: pars plana vitrectomy and scleral buckling surgery
This is the first of a series of articles that will have three aims. Firstly, to demonstrate why simulated ocular surgery should be an integral part of all ophthalmology surgical training programmes. Secondly, to describe exactly how simulated ocular surgery can be incorporated into any training programme, irrespective of where in the world you work, and thirdly, to convince experienced surgeons that simulation can play a role in further improving their surgical skills.
Across the globe there are pressures on surgical training in all specialties. Long training programmes, virtually unlimited access to surgical cases and a ‘see one, do one, teach one’ attitude are all in the past. Training programmes are getting shorter, there are fewer surgical opportunities on operating lists which are filled to capacity and, not before time, a greater emphasis is being placed on improving the safety of surgical training.
All of these factors contribute to reduced surgical opportunities for our current trainees. There are also concerns that despite the adoption of competency based surgical training programmes we are still producing ophthalmologists who are struggling surgically.
A survey of 58 US programme directors regarding over 2000 residents, published in 2006, revealed that 9% of residents had trouble mastering surgical skills, a quarter of these had poor hand eye coordination, one in five had poor intraoperative judgement and a third had still not overcome these difficulties by graduation [1].
Another factor to consider is the cost of surgical training. It has been estimated that it costs $50K in lost theatre productivity to train an ophthalmology resident in the US.
There is nowadays no doubt that increased time spent in practising surgical technique will speed up the learning curve. There is also, however, no doubt that being taught the correct thing to practise is as important. No single technique is uniquely better than another and for the trainee it is very important to learn a range of techniques so that surgical adaptability is built up.
So what are the core surgical skills we are trying to teach and how can simulation help develop these skills? Surgery is not just about learning isolated technical skills. Developing manual dexterity, the basics of instrument handling, dissection and suturing skills are important building blocks for any surgeon and simulation can certainly help to hone these skills, but surgery is much more complex than this. A good surgeon will have the ability to deal with evolving and unexpected situations, be able to give, listen to and act upon instructions, as well as have the ability to make good decisions in pressurised situations. If all simulation training does is to teach technical skills then we have missed an opportunity to fine tune the attributes that set surgeons apart from technicians.
The RCOphth Microsurgical Skills course is an excellent introduction to these basic building blocks of good surgical practice, but historically the opportunities to continue with this form of structured practise have been limited.
Myths about simulation
Myth number 1 – Simulation must be high tech and expensive.
The emergence of high fidelity virtual reality simulators has helped to raise the profile of simulation for cataract and vitreoretinal surgery. The Eyesi is a fantastic piece of equipment and there is an increasing body of evidence that trainees who have spent time using the Eyesi have reduced complication rates and a shorter learning curve when they transfer to live cataract surgery [2,3].
However, with the advent of the Eyesi there is a misconception that all simulation needs to be high tech and expensive and is out of the reach of many training units across the globe. In the UK we are fortunate to have 20 Eyesis, whereas a recent European Board of Ophthalmology survey, presented at the EVER conference in 2014, showed that there were only 10 in continental Europe. Even prestigious training centres in the US, such as the Bascom Palmer Eye Institute, do not have an Eyesi.
In the cataract and vitreoretinal (VR) sections of these articles we will discuss the role that the Eyesi can play in these forms of surgery, as well as describing how other cheaper, but equally effective techniques can be used to teach the same skills. In fact, some of these models offer a more realistic and versatile simulation experience than the Eyesi.
Myth number 2 – You have to use animal or cadaver material to accurately simulate ophthalmic surgery.
Historically, porcine eyes have been used in wet-labs to simulate cataract, glaucoma and corneal procedures. However, as well as limiting the training to dedicated wet-labs, this material does not provide a particularly realistic simulation experience. With the newer preparation techniques human cadaver material provides an extremely realistic method of simulating strabismus surgery, glaucoma surgery and some aspects of corneal surgery. However, access to this material is usually limited to an annual training session and does not lend itself to the concept of sustained deliberate practise.
Simulated ocular surgery eyes
The model eyes have been refined over a 15 year period by Craig Phillips (Phillips Studios), using a variety of materials that accurately replicate the look and, more importantly, the feel of real ocular tissues. They come complete with conjunctiva, Tenon’s capsule, extraocular muscles, including superior and inferior obliques, and a sclera that handles just like a human eye (Figure 1).

Figure 1: Strabismus eye.

Figure 2: Phaco eye.

Figure 3: Retinal eye.
The cataract models have a lifelike capsule, nuclei of varying densities and a posterior chamber that can be filled with a vitreous-like material (Figure 2). The retinal eyes can be used to perform three port vitrectomies, have retinal tears (Figure 3) and membranes that can be peeled. Furthermore, the model heads have noses and eyebrows that will hamper surgical manoeuvres just as they do in real life (Figure 4).

Figure 4: Model head.
Most importantly, these eyes can be taken into surgeons’ own operating theatres, so they can practise using the microscope, instruments and phaco / vitrectomy equipment they are familiar with. Many forms of simulated surgery such as strabismus surgery, retinal buckling surgery and basic trabeculectomy training, can easily be practised at home, with or without the aid of loupes.
Assessment
To help with assessing a trainee’s progress towards competence we have designed a series of Ophthalmic Simulated Surgical Competency Assessment Rubrics (OSSCARs) for cataract, VR, glaucoma and strabismus surgery. These are modifications of the scoring schemes designed by the International Council of Ophthalmology (ICO) for live surgery. The scoring systems are self-explanatory and include a global assessment of tissue handling, instrument handling and knot tying. A PDF of these OSSCARs can be downloaded from the SOS website.
We would suggest that all operations are broken down into blocks of two to three steps and only when a trainee is achieving a competent level for these blocks, are they allowed to perform the same stages of the procedure on a patient. As their confidence and competence grows they can string together more stages of the operation until they are able to perform the complete procedure.
Different trainees will progress at different rates and this will be dependent on their natural ability, their exposure to good instruction and perhaps most importantly, how much practise they put in. Rather than stipulating the time that should be spent on a simulator or the number of cases to be performed, the OSSCARs define what level of competence must be achieved before trainees should be allowed to operate on patients.
The Royal College of Ophthalmologists Curriculum Committee is currently drafting guidelines for the incorporation of simulation techniques into the ST curriculum. These will be published in September 2015.
Figure 5: Practising capsulorhexis techniques.
Cataract surgery simulation
There are two types of SOS cataract eyes. The basic eyes are hemispherical. The cornea has a similar feel to a real cornea, allowing trainees to practise wound construction and their corneal suturing skills. The lens has an anterior capsule, which has very similar properties to the human capsule and enables trainees to practise their capsulorhexis techniques (Figure 5). The lens itself is made from a gel-like material of varying consistencies, to mimic different types of cataracts. These lenses behave in a similar way to the human lens during phacoemulsification surgery, enabling the trainee to practise their sculpting, cracking and segment removal techniques (Figure 6). There is no lens cortex equivalent to practise aspiration of soft lens matter. Once the lens has been removed an intraocular lens (IOL) can be inserted.

Figure 6: Practising sculpting, cracking and segment removal techniques.
Basic cataract eyes with small (4mm) pupils have been designed to facilitate practising the insertion and removal of iris hooks and Malyugin rings.
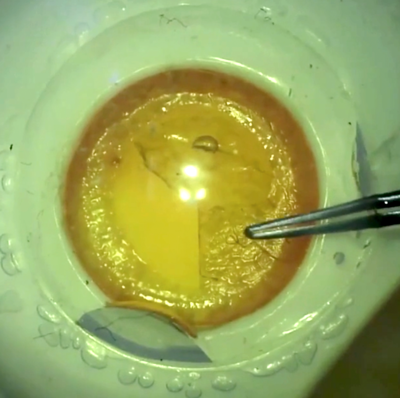
The advanced phaco eyes are spherical and have an anterior and a posterior chamber. The lens is encased within a capsule and the lens comes in a number of different densities, to simulate different types of cataract. The posterior chamber can be filled with egg white as a vitreous substitute. These eyes can be used to simulate either routine or complicated surgery such as posterior capsule (PC) rupture with vitreous loss (Figure 7) a dropped nucleus, dialysis +/- vitreous loss (insertion of capsular tension ring) and even an expulsive haemorrhage.

Figure 7: Simulating posterior capsule rupture with vitreous loss.
They enable trainers to set up lifelike simulation scenarios for more senior trainees who are learning to manage surgical complications, both in terms of techniques to be used, as well as machine settings and instrumentation. As experienced surgeons will have low posterior capsular rupture (PCR) rates, these eyes can be used to keep their anterior vitrectomy skills fresh or to familiarise themselves with the anterior vitrectomy settings on new phacoemulsification equipment.

Figure 8: The Eyesi.
If your training unit has access to an Eyesi, it will undoubtedly enhance your surgical training programme (Figure 8). One of the great strengths of the simulator is the ability to repeat tasks over and over again and see improvement. The cost of doing this is nothing other than your time. Some of its features like focussing and zooming with the foot pedal controls are just like the real thing and although some of the programmes are not so realistic, they do provide a consistent training environment which is assessed. There are structured programmes to work through which get progressively harder and allow a sense of achievement – similar to reaching the ‘next level’ on a video game!
The capsulorhexis programme is very realistic in terms of its tissue handling, with manoeuvres like the little rescue technique accurately rendered. This allows for very realistic tearing vectors to be practised.
Limitations include the initial capital cost and the cost of ongoing software updates. Other limitations are the physical feel of the simulation – it is very much a visual feedback rather than tactile and although the programming algorithms are improving all the time, there is currently not a realistic way of simulating some complications such as vitreous loss and anterior vitrectomy.
A combination of initial training on the Eyesi, followed by practice in theatre with the SOS models, will prepare trainees for the transition to ‘live’ surgery. Once trainees are ready to commence live surgery a number of models of training have been used and these range from repeating the same part of the procedure several times on a list, to so-called reverse training wherein the steps of the procedure are learned from the end of the procedure forwards, so in theory at least the trainee is operating in good conditions all the time.
Whichever method of actually performing surgery is used, there is no question that frequent repeated practise using the SOS models and the simulator will provide trainees with a more comfortable learning experience and a more rapid progression to becoming an adept adaptable surgeon.
References
1. Binenbaum G, Volpe NJ. Ophthalmology resident surgical competency: a national survey. Ophthalmology 2006;113:1237-44.
2. Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg 2011;37:1756-61.
3. Spiteri AV, Aggarwal R, Kersey TL, et al. Development of a virtual reality training curriculum for phacoemulsification surgery. Eye 2014;28:78-84.
All of the simulation techniques that will be described in this series of articles can be found on the Simulated Ocular Surgery website (www.simulatedocularsurgery.com). The next two articles will cover ‘retinal buckling surgery and vitrectomy simulation’ and ‘glaucoma and strabismus surgery simulation’.
Declaration of Competing Interests: John Ferris designed and owns the Simulated Ocular Surgery website.
COMMENTS ARE WELCOME