Understanding pupillary reactions is vital in understanding basic neuro-opthalmology. It is a skill required in eye casualty, clinics and perhaps most importantly, exams. To start at the beginning, the pupil is the central aperture of the iris, its size controlling the amount of light falling on the retina, varying in diameter from about 1-8mm. Pupil size is a result of the interplay between the sympathetic and parasympathetic nervous system supplying the intrinsic muscles within the iris, the dilator and sphincter pupillae respectively. The clinical examination of the pupils and pupillary reflexes are crucial in obtaining an accurate diagnosis of a clinical problem.
Normal pupil reflexes
Pupil constriction
Pupillary constriction is the result of the parasympathetic system activity and is normal in response to two types of stimuli; light falling on the retinal photoreceptors and the effort of near reflex and accommodation.
Light reflex
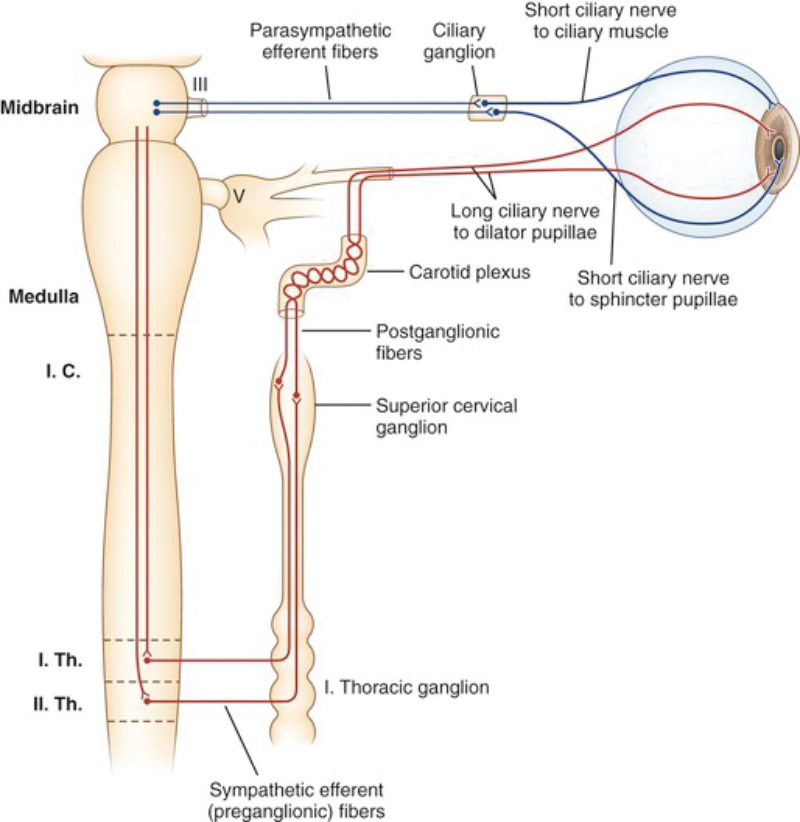
Constriction of the pupils in response to light involves four sets of neurons. The afferent pathway starts in the ganglion cell layer of the retina, which gives rise to the optic nerves. Fibres leaving the optic chiasm enter both optic tracts and terminate in the pretectal nuclei. Each pretectal nucleus is linked to its ipsilateral Edinger-Westphal nucleus by internuncial neurons. The contralateral Edinger-Westphal nucleus is reached by way of the posterior commissure.
This pathway results in the direct and indirect light reflex as the input to one optic nerve reaches both Edinger-Westphal nuclei. Pre ganglionic parasympathetic fibres enter the oculomotor nerve, leave the branch to the inferior oblique, and synapse in the ciliary ganglion. Postganglionic fibres run in the short ciliary nerves and enter the iris to supply the sphincter pupillae (Figure 1).
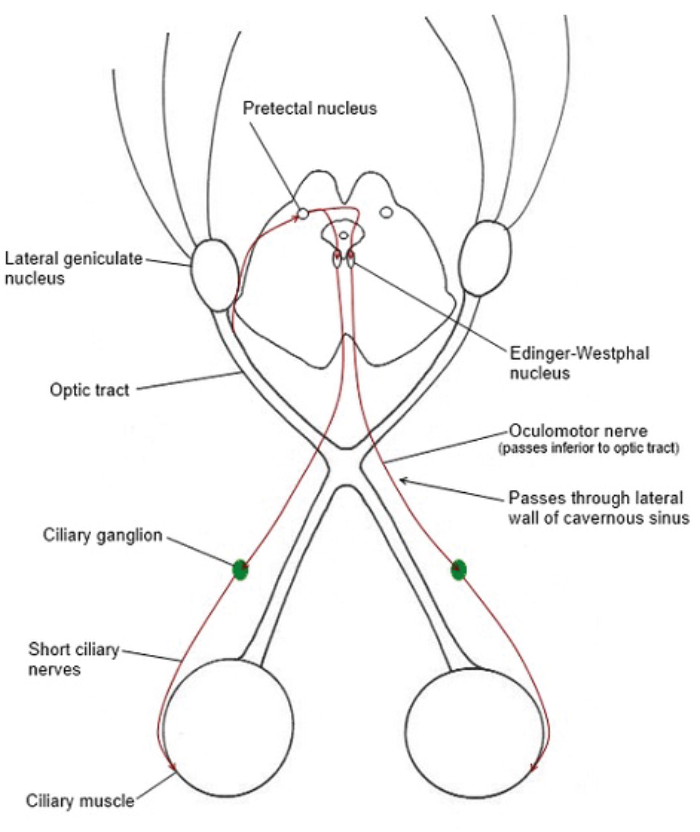
Figure 1: The light reflex.
Accommodation
With accommodation the afferent limb of the reflex passes from the retina to the occipital lobe via the lateral geniculate body. The efferent limb passes from the occipital lobe to the midbrain, where some fibres activate the Edinger-Westphal nucleus as well as the vergence cells in the reticular formation. Vision is not needed to achieve accommodation. Bilateral stimulation from pre-striate cortex area 19 to the Edinger-Westphal nuclei will do the same trick. This results in three responses: the ciliary muscles contract, relaxing the zonules causing the lens to become more globular, increasing the refractive power. At the same time the sphincter pupillae contracts eliminating the passage of light through the peripheral, thinner part of the lens. The medial recti increase in tone causing the two eyes to converge.
Pupil dilatation
Pupil dilatation on the other hand is the result of sympathetic activity. The sympathetic pathway starts with the central neuron in the posterior hypothalamus which as it descends is joined in the pons and medulla by the ipsilateral fibres descending from the reticular formation. The pre-ganglionic neuron emerges from the first thoracic ventral nerve root to enter the paravetebral sympathetic chain, which runs up to the superior cervical ganglion. Post-ganglionic fibres travel along the external and internal carotid artery. Some of the sympathetic fibres join the ophthalmic division of the trigeminal nerve in the cavernous sinus, then leaves this in the long ciliary nerve to supply the dilator pupillae (Figure 2). This pathway also supplies the Muller’s muscle of the eyelids and the sweat glands of the face. In the far response or in the presence of anxiety, stress or fear, the pupils dilate through this sympathetic activity.
Figure 2: The pupillary dilation reflex.
Examination
Examination of pupils
Step 1 – Compare the sizes of the pupils in the light and the dark. Pupils should be examined in light and then in the dark. A comparison of the size, symmetry and shape of the pupils in both eyes is crucial. Get the patient to fix their eyes on a distant point to begin with, then to observe the pupils through a side illumination.
Anisocoria is an inequality in the size of the pupils. Physiological anisocoria occurs in about 25% of individuals but the difference in size should not be more than 1mm. A greater difference than this is pathological anisocoria. The pathological pupil is the one with the deficient reactivity – either not constricting well to light or dilating poorly in the dark. Thus the largest pupil in the light or the smallest pupil in the dark should be the prime suspect in determining which is the abnormal pupil.
Step 2 – Direct and consensual light reflexes. A normal light reflex results in the constriction of both pupils to light (direct and consensual reflex). First test the direct light reflex – a normal pupil will constrict when light is directed to it. However, observe the other eye – the other pupil will constrict even without exposure to light (consensual light reflex). In this manner defects in the afferent or efferent pathways of the light reflex can be established.
Step 3 – Swinging flashlight test / relative afferent pupillary defect. This test is used to detect an afferent defect. When light is shone on the normal side, the pupil constricts but when the light is quickly shifted to the abnormal side, that pupil will dilate. When the light is moved back to the normal pupil again, that pupil will reconstrict again as there was no consensual reflex from the abnormal pupil. This clinical sign is known as a relative afferent pupillary defect (RAPD).
Even in the presence of bilateral optic nerve disease, an RAPD can still be detected as in most cases, the damage will not be equal: thus the optic nerve with the greater damage will manifest in a RAPD. In exceptional cases, when the degree of damage to both optic nerves is very similar, both pupils will show sluggish reactions to light. Causes of RAPD include: optic nerve disorders (optic nerve compression, optic neuritis), chiasm compression, retinal detachment, large unilateral macular lesion or advanced unilateral glaucoma.
Step 4 – Accommodation. Finally, accommodation can be tested by asking the patient to fixate on a distant point and then asking them to shift their focus quickly to a near object. Normally, the pupils constrict and the eyes converge while fixating on a near object. In exams, but certainly not in real life, pupils that constrict through accommodation but not through direct light stimulation, if due to neurosyphilis, are called Argyll Robertson pupils. I guarantee you will never see a case of this in your entire career, but you will be punished by examiners for not knowing it.
Conditions with pathological pupil size:
Single large pupil
Adie’s tonic pupil
An Adie’s tonic pupil is an anisocoria where the abnormal pupil is larger and does not constrict to light but slowly constricts to accommodation (Figure 3).

Figure 3: A patient with left sided Adie’s pupil.
This is referred to as a light-near dissociation. The pupil usually shows slow constriction on prolonged near effort and slow re-dilatation to distance. It is due to damage of the post-ganglionic fibres of the parasympathetic pathway. In 90% of patients, it presents unilaterally initially but often becomes bilateral. Eventually, the pupil becomes tonic with time and even miotic, a so called ‘little old Adie’s pupil’. This condition usually affects females and can be caused by viral infection, diabetes or trauma but is often idiopathic. If decreased tendon reflexes are present it is referred to as Holmes Adie syndrome. Diagnosis is confirmed by denervation hypersensitivity to weak cholinergic agents (0.125% pilocarpine), an abnormal pupil will constrict whilst a normal pupil remains unaffected.
Acute angle closure glaucoma
This happens when the anterior chamber angle is closed mechanically by the crowding of the peripheral iris when the pupil is semi dilated. This could be due to an intraocular tumour, formation of anterior synechiae or posterior synechiae following uveitis or rubeotic glaucoma caused by fibrovascular proliferation in the chamber angle secondary to retinal ischaemia (diabetes and central retinal vein occlusion classically). This condition is an ocular emergency often suspected from the history alone but needs to be confirmed with slit-lamp examination. A patient with this condition will need to be referred immediately to the ophthalmologist. Intraocular pressure lowering drugs, topical miotics and glaucoma drops are used to lower the eye pressure and these patients can be listed for an iridotomy or peripheral iridectomy.
Third nerve palsy
A third nerve palsy can either be complete or partial. A complete third nerve palsy is evidenced by a fully dilated pupil, fully abducted ‘down and out’ eye, complete ptosis and no constriction to either light or accommodation. You can confirm that the lesion is in the efferent pathway by shining light into that eye and noting that the pupil does not constrict but the consensual light reflex in the contralateral pupil is intact. Causes include microvascular infarction – occlusion of the vasa nervorum (risks: hypertension diabetes, atherosclerosis), compressive lesion (aneurysm, tumour) or due to trauma. In a partial third nerve palsy, the symptoms are not so severe but could be a sign of an impending emergency. Rapidly increasing intracranial pressure resulting from an acute extradural or subdural haematoma, often compresses the third nerve against the crest of the petrous temporal bone. The parasympathetic fibres are superficially placed and therefore the first to suffer, causing the pupil to dilate progressively on the affected side. Pupillary dilatation is an urgent indication for surgical decompression of the brain and a computed tomography (CT) angiogram looking for intracranial aneurysms is almost always indicated.
Single small pupil
Horner’s syndrome
Horner’s syndrome is a condition that affects the sympathetic pathway supplying the face and eye. This results in mild ptosis, a regular miotic pupil with pupil dilation lag, anhydrosis and pseudoenophthalmos (due to the ptosis and smaller palpebral fissure – see Figure 4).

Figure 4: A patient with left sided Horner’s syndrome.
Check the face for impaired sweating on the same side (may be easier to ascertain this information from the history). Examine the colour of the iris. Heterochromia of the iris with a lighter colour on the affected side will point to a congenital Horner’s syndrome. A deficient sympathetic stimulation in childhood results in impaired melanin deposition by the melanocytes in the superficial stroma of the iris.
“Remember to specifically ask for any history of trauma to the eye including surgical trauma. A blunt force to the eye can cause the anterior uvea to sustain structural and / or functional damage.”
Horner’s syndrome can be confirmed with the cocaine test. Ten percent topical cocaine dilates a normal pupil, as it prevents the re-uptake of norepinephrine from the post-ganglionic synapse resulting in overstimulation at the synapse and pupil dilatation. In Horner’s syndrome, there is a deficiency of norepinephrine at the synapse resulting in a poor dilation of the affected pupil. A post-cocaine anisocoria of greater than 0.8mm confirms a Horner’s pupil on the side of the smaller pupil. Most cases of Horner’s syndrome are innocuous but in some cases it may be sinister, for example thyroid carcinoma, a bronchogenic carcinoma of the apex of the lung (Pancoast tumour), carotid artery aneurysm, dissection of the carotid artery, lymphoproliferative disorders or brachial plexus injury. In practice it is near impossible to get hold of cocaine so a handy alternative is the ‘iopidine test’ using apraclonidine, a weak adrenergic agonist that reverses the anisocoria caused by Horner syndrome through denervation hypersensitivity [1].
Anterior uveitis
A patient with a unilateral red, painful eye with impaired vision and a small irregular pupil is most likely suffering from anterior uveitis. The diagnosis can be easily made on slit-lamp examination: an acute episode will show ciliary injection, endothelial dusting, aqueous cells, anterior vitreous cells and in severe cases hypopyon and posterior synechiae. Recurrent episodes of anterior uveitis will result in a painless irregular mitotic pupil which does not dilate in the dark. On slit-lamp examination, pigment deposits on the lens, keratoprecipitates can be seen and in some cases iris nodules and atrophy will also be present.
Bilateral small pupils
Iatrogenic
The use of eyedrops should always be considered when presented with bilateral constricted or dilated pupils. For example, miotics such as pilocarpine may be in treatment of glaucoma. Short acting mydriatics are used to enhance examination of the lens, vitreous and fundus. Mydriatics are also used in the treatment of acute uveitis especially iridocyclitis and severe corneal epithelial defects to relieve the spasm of the ciliary muscle and iris sphincter and breakdown / prevent the formation of posterior synechiae. The following are a list of common topical medications:
Mydriatics:
- Cholinergic antagonists
- Atropine
- Cyclopentolate
- Tropicamide
- Adrenergic agonist
- Phenylephrine
Miotics:
- Cholinergic
- Pilocarpine
- Anticholinesterase
- Physostigmine
- Neostigmine
Trauma
When taking a history from a patient with pupil abnormalities, remember to specifically ask for any history of trauma to the eye including surgical trauma. A blunt force to the eye can cause the anterior uvea to sustain structural and / or functional damage. The iris may be transiently compressed against the anterior surface of the lens by severe anteroposterior force, with resultant imprinting of the pigment from the pupillary margin. Transient miosis accompanies the compression.
Any kind of trauma causing damage to the iris sphincter may result in traumatic mydriasis, which can be temporary or permanent – the pupil will react sluggishly or not at all to light or accommodation but the consensual reflex in the other eye will be present. Iridodialysis is a dehiscence of the iris from the ciliary body at its root. The resulting pupil is typically D shaped and the dialysis is seen as a dark biconvex area near the limbus.
Conclusion
Examination of the pupils and pupillary reflexes are crucial in obtaining an accurate diagnosis of an ophthalmological problem and many other systemic conditions. It is a relatively simple examination that can be performed at most patients’ bedsides and is a skill all doctors should have.
Reference
1. Morales J, Brown SM, Abdul-Rahim AS, Crosson CE. Ocular effects of apraclonidine in Horner syndrome. Arch Ophthalmol 2000;118:951-4.
TAKE HOME MESSAGE
-
Familiarise yourself with the variations of normal pupils and their reflexes.
-
Anisocoria of more than 1mm should always be questioned / investigated further.
-
Have a low threshold for further testing and imaging.
COMMENTS ARE WELCOME