A 56-year-old type 2 diabetic with previously treated bilateral diabetic maculopathy develops a cataract requiring surgery in the right eye. He has had grid laser previously, followed intermittently by intravitreal triamcinalone, Avastin and more recently Lucentis in both eyes. His last injection was three months ago in the right eye and six months ago in the left eye. RE VA is 6/18; LE VA is 6/7.5. The left macula is dry on OCT but the quality of his optical coherence tomography (OCT) is now affected by the cataract in the right eye which is becoming more symptomatic. How would you manage him?
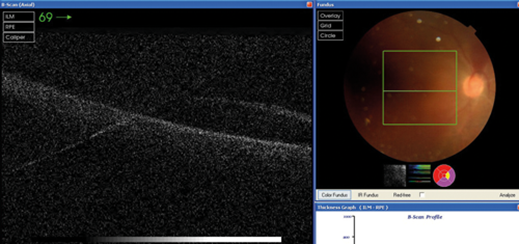
Figure 1: RE OCT showing poor quality scan due to posterior subcapsular lens opacity (PSCLO) cataract.
This patient has known diabetic macular oedema (DMO) that has required intravitreal therapy to manage, therefore there is a high risk of suffering recurrent DMO following cataract surgery leading to a suboptimal visual outcome. I would be keen to perform their surgery promptly and combine their cataract surgery with an injection of steroid. The clinician has a choice between intravitreal Kenalog 4mg/0.1 ml (unlicensed) or Ozurdex 700mcg dexamethasone implant (recently licensed).
I normally consider performing the injection procedure just prior to intraocular lens (IOL) implantation with the viscoelastic completely filling the lens bag. I find the eye is formed and unlikely to collapse with the injection procedure, but also allows you to easily examine the central retinal artery and assess that the steroid has been delivered intravitreally. I then proceed to IOL implantation and complete the surgery.
I will commence the patient on topical steroid and antibiotic as standard post-cataract surgery protocol, but would not bother with additional topical nonsteroidal anti-inflammatories (NSAIDs) as I have just given intraocular steroid. I would arrange for the patient to be assessed in clinic a fortnight after surgery, and check the intraocular pressure and examine how the eye has settled following surgery, and degree of visual rehabilitation. If the patient has had a satisfactory functional and anatomical response I would arrange to see them again in two to three months.
If my clinical judgment in the improvement in DMO was suboptimal, an unusual scenario with intravitreal steroid, I would see the patient for a repeat OCT four weeks later to decide if additional laser or an anti-VEGF agent is required.
Mr Fahd Quhill, Consultant Ophthalmologist, Royal Hallamshire Hospital, UK.
This scenario needs a bespoke assessment of the options preoperatively, perioperatively and postoperatively.
It is probably true to say that the previous practice of avoiding or delaying cataract surgery in the presence of DMO until it has dried out for a number of months is no longer necessary. The availability of a number of treatments other than laser for DMO offers a variety of management options. For this patient the timing of cataract surgery is likely to be dictated by progressing cataract making the vision worse and / or the assessment of the fundus more difficult.
Preoperatively, the patient’s expectations need to be addressed depending on the anticipated functional outcome of surgery. The patient needs to be reminded of the fact that the visual improvement is limited by the extent of pre-existing DMO and that treatment for the DMO may continue long after the surgery. In addition, the treatment for the DMO may continue right up to the time of cataract surgery, be that with laser or intravitreal therapy.
Perioperatively, I prefer to combine any ongoing intravitreal therapy with cataract surgery. This includes all available anti-VEFG and steroids. I usually perform the injection after the completion of the cataract surgery, rendering the eye ‘intact’ as if the patient were just having the intravitreal injection. If I doubt that either of the two corneal wounds are leaky I would place a 10/0 vicryl suture before the injection.
Postoperativley, I use the standard post cataract combination of steroid and antibiotic eye drops. I would review this patient at no longer than four weeks post the combined surgery and injection procedure. The assessment of the DMO will decide the next treatment steps. One potential difficult aspect is deciding whether persistent macular oedema post surgery is purely DMO, purely cystoid macular oedema (CMO) or a combination of both. I find the use of fundus fluorescein angiography (FFA) in these situations very helpful to decide what treatment to try. A small subgroup of diabetics will also be glaucoma patients on prostaglandin analogues, the management of which is subject to various opinions. Suffice it to say it is a point worth considering with persisting predominantly CMO in this scenario. Finally, non-steroidal anti-inflammatory eye drops in the prevention of post cataract surgery CMO has been noted more so in the published literature over the last 12-24 months. However, there continues to be a difference of opinion as to its exact role in relation to a specific patient cohort as well as its cost-effectiveness, given its unit cost compared to most post cataract surgery treatment regimes. Its role in a scenario like the subject of this article is even less clear with the presence of intravitreal injections, especially the steroids.
Mr Samer Elsherbiny, Consultant Ophthalmologist, Birmingham and Midland Eye Centre, UK.
COMMENTS ARE WELCOME






