These are a group of strabismus disorders where the angle of misalignment is different between near and distance. The focus of this article will be on the patients where the angle for near exceeds the distance angle by more than 10 prism dioptres (pd). These cases will be divided into N>D esotropias and N>D exotropias. The discussion will focus on management of these patients clinically and surgically.
Near esotropia (convergence excess esotropia)
These are a group of patients with near angle esotropia that exceeds the distance fixation angle by more that 8-10pd after full hypermetropic correction. These are a heterogeneous group of patients that can be subdivided into these categories:
- Non-refractive accommodative esotropia (convergence excess with high AC/A ratio): a. Usually esophoric or orthophoric at distance or have microtropia b. High AC/A ratio
- Non-accommodative convergence excess esotropia (near esotropia): a. Usually esophoric or orthophoric at distance or have microtropia b. Normal AC/A ratio
- Hypo-accommodative convergence excess esotropia (low AC/A ratio): a. Low AC/A ratio b. Remote near point of accommodation
- Partially accommodative esotropia with high AC/A ratio a. Esotropic for distance fixation.
Management
It is difficult to interpret literature data on this subject due to the heterogeneity of the group and different approach to managing these patients between the countries. The management is subdivided into non-surgical options and surgical management.
Convergence excess with high AC/A ratio:
Non-surgical treatment:
- Correction of refractive errors especially hypermetropia
- Treatment of amblyopia
- Bifocal glasses: they should be tried on all N>D esotropia. This helps differentiate convergence excess patients (high AC/A) from near esotropia patients (normal AC/A) who would not respond. The ultimate aim is to reduce the near add gradually until eliminated, although this is not always possible.
- Other options include contact lenses, botulinum toxin and orthoptic exercises. These are less successful options, mitotic drops has been discontinued as an option.
Surgical treatment: especially in patients where non-surgical treatment has failed, have esotropia of 20pd or more for near or have AC/A ratio of 8:1 or more.
The aim of the surgery is to reduce the near esodeviation to a level controlled by patient fusion reserves, as well as relieve the need for bifocal glasses and eliminate any diplopia symptoms.
It is important to prism adapt the patient in order to find the maximal deviation angle and identify the patient’s risk of over or undercorrections. Surgical options include unilateral or bilateral medial rectus recessions (standard or augmented), posterior fixation sutures (PFS) and marginal myotomy.
The dose of the standard recession is based on the outcome of the prism adaptation test. If patients remain slightly esophoric for near and distance (good binocular single vision, (BSV)) then surgery should aim to correct the full near prism-adapted angle (fixed or hang-back). If patients become exotropic for distance (suggestive of poor BSV) then bilateral medial rectus recession with PFS targeting 2/3 of the prism needed to leave the patient with small distance esophoria.
Smaller bilateral recessions or unilateral recessions tend to be ineffective.

Near esotropia:
Management: the treatment is usually surgical as other options usually fail to help. Bilateral medial rectus recession is the operation of choice in most cases, with looped sutures for added effect if warranted by the degree of esotropia. PSF with or without recession is another option. The target angle depends on the patient BSV potential as in convergence excess esotropia. Hang-back recessions are technically easier, whereas PFS surgery is challenging, prone to undercorrections and non-reversible. Y-splitting procedures offer an alternative method to address esotropia with larger angles at near than at distance. It reliably reduces distance / near disparity also in cases of reoperation and in unilateral surgery. Its effects may take a little longer to stabilise than with traditional recession or resection surgery, but its long-term effects are stable.
Hypo-accommodative convergence excess:
Management is usually optical options with refractive correction and bifocals.
Partially accommodative esotropia with high AC/A ratio:
Management: Non-surgical includes refractive correction of significant hypermetropia, treatment of amblyopia, use of prisms and use of botulinum toxin in small angle deviations.
Surgical management is either bilateral medial rectus recessions or unilateral recess / resect procedure. The target angle depends on BSV potential, patients who do not have that are left undercorrected by 5-8pd. Any significant alphabetical patterns should be corrected as can destabilise the surgical outcome. The surgical dose is based on the near angle (either prism adapted or average angle with and without glasses) in patients with high AC/A ratio and if more than 45pd then surgery on more than two muscles is needed.
Near-distance disparity exotropia
This is different to near esotropia where there is a link between convergence and accommodation which usually explains the difference in squint angle between near and distance fixation.
Intermittent exotropia could be divided into three groups, distance exotropia (which could be true or simulated), basic (non-specific) exotropia and near exotropia (again true or simulated).
Two of these groups will have near – distance disparity: true distance exotropia (divergence excess, where the distance angle is bigger than the near angle by at least 10pd) and true near exotropia (convergence insufficiency, where the near angle is bigger than the distance angle by at least 10pd).
In order to differentiate these groups, patients with intermittent exotropia should have a period of monocular occlusion in order to abolish the slow fusional and proximal convergence mechanisms and reveal the true near and distance deviation.
The following discussion will be for near exotropia patients.
Intermittent near exotropia:
This can be divided into two groups following monocular occlusion, true intermittent near exotropia where the angle does not change following occlusion and simulated intermittent near exotropia where the distance angle increases to match the near angle. This group is rare and usually managed as non-specific intermittent exotropia.
The true near exotropia is relatively uncommon and possible features include asthenopia symptoms, diplopia, poor convergence and reduced fusional range.
Management: It is important to correct any significant refractive errors or amblyopia. Assessment of level of control is also important and that can be done by various methods such as Newcastle control score and assessment of any binocular functions and angle of deviation and convergence for near fixation.
Non-surgical treatment: This is usually in patients with small angles, risk of over corrections and patients who cannot have surgical intervention.
Options include:
- Prisms: particularly in decompensating exophoria or in postoperative period.
- Orthoptic exercises: usually as a supplement to treatment in order to help improve control and increase convergence.
- Botulinum toxin: either as a definitive treatment option or in the post-operative period.
Surgical treatment: only if the deviation is large or has poor response to non-surgical options. The aim of surgical intervention is to preserve or restore binocular function or improve deviation angle by having a residual angle of less than 5pd esotropia to less than 10pd exotropia.
The surgical dose is usually based on the near deviation angle.
Recommended procedures for near exotropia:
- Unilateral or bilateral medial rectus resection. In order for this to have a stable outcome, it requires a period of over correction which some patients find difficult to tolerate. It is possible to use this in cases where the distance angle is less than 10pd with possible use of adjustable sutures in suitable patients.
- Unilateral medial rectus resection and lateral rectus recession. This can be done in asymmetric way (improved R&R, medial rectus resection based on the near angle and lateral rectus recession based on the distance angle).
- Other techniques have been described such as the use of slanted recession of the lateral rectus muscle for exotropia patients (upper border for the distance deviation and lower border for the near deviation). This helps collapsing the difference between the near and distance angles.

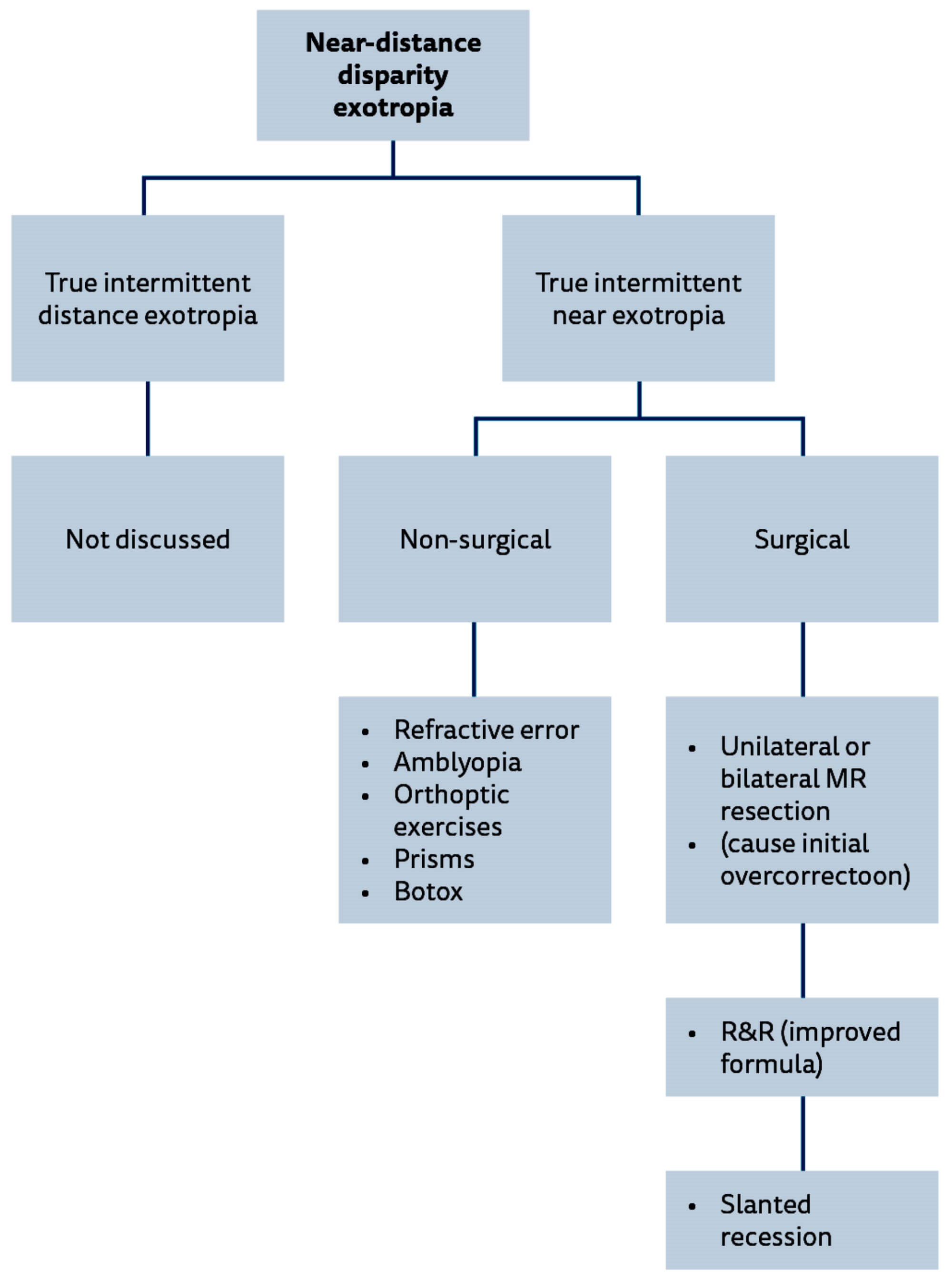
Figure 1: Management options flow chart for patients with near – distance disparity strabismus. BMR: bi-medial recession, BSV: binocular single vision, PFS: posterior fixation suture (Faden), R&R: recess / resect procedure.
Conclusion
Near-distance disparity represented a challenge to ophthalmologists. It is sometimes difficult to classify these patients and know what type of treatment to offer to patients and in cases of surgical intervention, which procedure to do and what is the target angle.
It is important to have a full assessment of the patient with all the details available before committing to a surgical correction. It is also important to explain to the patient the surgical expectations and make sure they are aware of the limitations of the surgical options.
Further reading
- Ansons AM, Davis H. Diagnosis and management of ocular motility disorder. Wiley-Blackwell; 2013.
- Burke JP. Distance-near disparity esotropia: can we shrink the gap? Eye (Lond) 2015;29(2):208-13.
- Kushner BJ, Morton GV. Distance/near differences in intermittent exotropia. Arch Ophthalmol 1998;116(4):478-86.
- Wipf M, Priglinger S, Palmowski-Wolfe A. Y-Split Recession of the Medial Rectus Muscle as a Secondary and/or Unilateral Procedure in the Treatment of Esotropia with Distance/Near Disparity. J Ophthalmol 2017;2017:6472690.
- Intermittent Exotropia: A Major Review. Rahul Bhola. EyeRound.org. 2006.
- Brodsky MC, Fray KJ. Surgical management of intermittent exotropia with high AC/A ratio. J AAPOS 1998;2(6):330-2.
- Wang B, Wang L, Wang Q, Ren M. Comparison of different surgery procedures for convergence insufficiency-type intermittent exotropia in children. Br J Ophthalmol 2014;98(10):1409-13.
COMMENTS ARE WELCOME





