Anatomically the cavernous sinus is a plexus of multiple veins that are connected and within this plexus there are several important vascular and neurological structures. These include cranial nerves III, IV, V1 (and sometimes V2), VI as well as the sympathetic carotid plexus and a section of the carotid artery.
These sinuses sit on either side of the sella turcica with the pituitary gland in the middle. Orbital veins (superior and inferior) drain into the cavernous sinuses which in turn drain into petrosal sinuses.
It is known that cranial nerves III, IV and V1 are situated within the lateral wall of the cavernous sinus but cranial nerve VI floats within the sinus beside the carotid artery.
It is important to clarify that it is very difficult to differentiate cavernous sinus syndrome (CSS) from superior orbital fissure syndrome as most of the above-mentioned structures will continue to go through the superior orbital fissure into the orbit.
The term ‘orbital apex syndrome’ is usually reserved for cases with multiple ocular motor nerve palsies as well as optic nerve dysfunction.
Presentations
These patients usually come with complains of ipsilateral ocular motility abnormalities suggestive of cranial nerve palsies along with periorbital pain and sensory dysfunction due to V1 involvement as well as sympathetic dysfunction (Horner’s). Patients can also have soft tissue signs such as chemosis and proptosis.
Aetiology
Cavernous sinus syndrome will usually cause painful ophthalmoplegia. This could be due to various reasons that can be summarised into the following categories:
- Inflammatory:
a. Sarcoidosis
b. Granulomatosis with polyangiitis (GPA)
c. Tolosa-Hunt syndrome - Infectious or parainfectious:
a. Viral infections: Herpes Zoster
b. Bacterial infections: spreading from adjacent structures such as sinusitis
c. Fungal infections: most significantly mucormycosis
d. TB - Vascular:
a. Cavernous sinus thrombosis (usually secondary to spread of infection from a local source such as paranasal sinus infection or orbital cellulitis)
b. Carotid-cavernous fistula
i. Direct fistula
ii. Dural (indirect) fistula
c. Carotid artery (intra cavernous) aneurysm - Tumours:
a. Pituitary adenoma
b. Craniopharyngioma
c. Nasopharyngeal carcinoma
d. Meningioma
e. Neurofibroma
f. Lymphoma
g. Metastatic disease - Trauma.
Differential diagnosis
There are several conditions that can mimic presenting features of cavernous sinus syndrome. These could include:
- Ocular myasthenia gravis (MG)
- Thyroid orbitopathy
- Local orbital diseases (inflammatory, etc.)
- Giant cell arteritis (GCA)
- Cranial nerve palsies
- Miller Fisher syndrome: ataxia, areflexia and ophthalmoplegia. Test for anti GQ1b antibodies.
Investigations
Urgent neuroimaging is always necessary. Depending on local availability, a CT scan could be done but ideally an MRI / MRA scan is needed. It is important to have orbital and coronal sections as it is important to assess orbits to rule out local orbital disease. Blood tests for routine tests and inflammatory markers are sometimes needed to rule out mimics such as GCA, MG and Miller Fisher.
Case study
A 76-year-old male presented to the eye emergency clinic with four months history of left eye redness lid swelling and irritation. This had got significantly worse in the last few days with spreading of the swelling. His symptoms are worse morning but generally get better as the day goes on. He also complained of pulse synchronous tinnitus. Past ophthalmic history includes bilateral cataract surgery and ingrowing eyelashes. His previous medical history includes hypertension and diabetes type II on treatment.

Figure 1: Appearance of left eye on recent eye emergency presentation.

Figure 2: Appearance of left eye from previous visits to the hospital.
On ocular examination, his visual acuity was excellent at 6/6 in both eyes. Slit-lamp examination showed bilateral pseudophakia, with moderate left proptosis, lid and conjunctival chemosis, mildly raised intraocular pressure and a left VI nerve palsy (Figures 1 and 2). He had blood tests for full blood count (FBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and thyroid function tests, as well as a brain and orbits CT scan plus angiogram (CTA) as the clinical signs were very localising to the left orbit / left cavernous sinus.
The CT / CTA findings confirmed the proptosis and enhancement of the left cavernous sinus as well as the left superior ophthalmic vein confirming the carotid – cavernous fistula (Figures 3 and 4).

Figure 3: Enhancement of left cavernous sinus on CTA (red arrow).
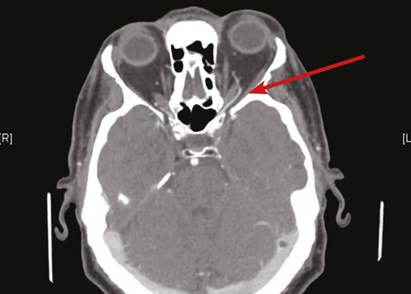
Figure 4: Enhancement of left superior ophthalmic vein suggestive of left CCF (red arrow).
He was also managed with lubrication eye drops and latanoprost to control his intraocular pressure.
Conclusion
It is important to recognise the signs and features suggestive and localising to the cavernous sinus. It is important to investigate these patients urgently and treat accordingly.
References
1. Bone I, Hadley DM. Syndromes of the orbital fissure, cavernous sinus, cerebello- pontine angle, and skull base. J Neurol Neurosurg Psychiatry 2005;76(Suppl III):iii29‑iii38.
2. Foroozan R, Vaphiades M: Kline’s Neuro-Ophthalmology Review Manual (8th ed). SLACK Incorporated; 2017.
COMMENTS ARE WELCOME





