History
-
A 37-year-old male was referred from the Emergency Eye Clinic with a swollen right upper eyelid.
-
Symptom relieved with nonsteroidal anti-inflammatory drugs (NSAIDs).
-
The initial clinical diagnosis was dacryoadenitis.
-
The patient presented again six weeks later with 3mm proptosis, hypoglobus and decreasing visual acuity.
-
CT scans (Figure 1) revealed concerning features.
-
Considering the clinical differential diagnoses he had incisional biopsy done for histopathological assessment.
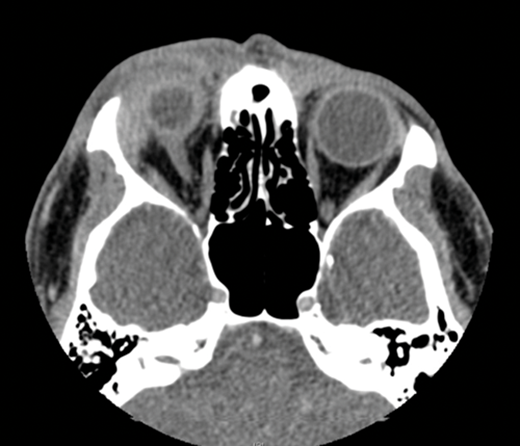
Figure 1.
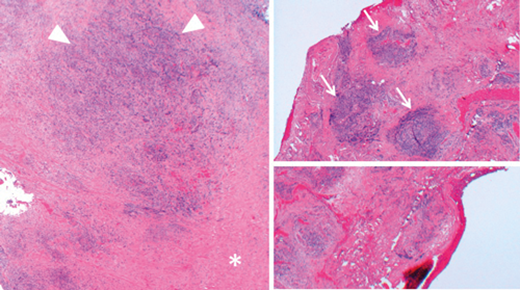
Figure 2.
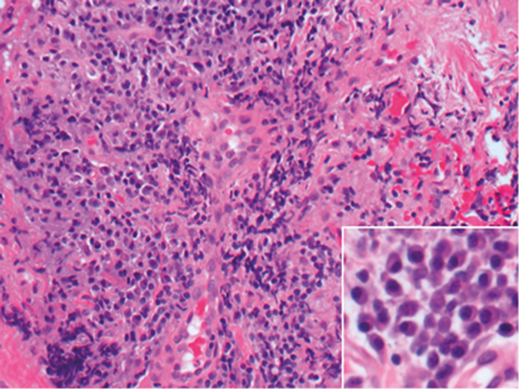
Figure 3.
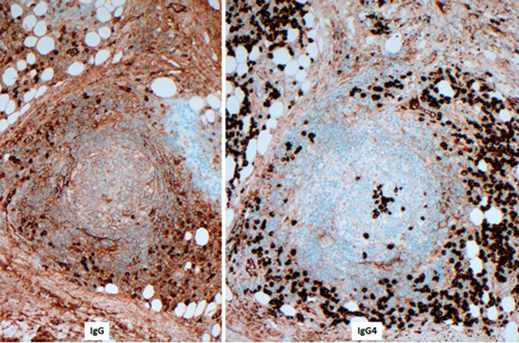
Figure 4.
Questions
-
How can Figure 1 be described? What clinical differential diagnoses could be considered?
-
How can Figures 2 and 3 be described?
-
Based on findings seen in Figures 1-4, what is the likely diagnosis? Are there any further useful diagnostic tests to be considered?
Answers
1. The image shows a right orbital mass displacing the globe. The mass is not distinguishable from the lacrimal gland. Possible differential diagnoses include but are not restricted to lymphoproliferative lesion, orbital inflammation and granulomatous disease.
2. In Figure 2 orbital fat was completely replaced by fibrosis (asterix) and diffuse chronic inflammation (arrow heads). Separate areas contain lymphoid aggregates (arrows). Figure 3 shows sheets of plasma cells. Eccentric nuclei of plasma cells are better appreciated on the inset.
3. The presence of sclerosing inflammation including plentiful plasma cells which show a high IgG4 + /IgG+ ratio >40% is suggestive of IgG4 related sclerosing disease. However, the definitive diagnosis still requires correlation with IgG4 serum levels. The above features in addition to serum IgG4>135 mg/dL or radiologically / biopsy proven involvement of other organs are diagnostic for IgG4 related sclerosing disease.
COMMENTS ARE WELCOME




