*Please be aware that this data does not form part of a peer reviewed research study. The information therein should not be relied upon for clinical purposes but instead used as a guide for clinical practice and reflection.
I continue to be surprised by the outcomes of our surveys. I hope the readership look at the outcomes and reflect on their own practice. Certainly, the outcomes have been eye-opening for me, and I have changed some of my standard practice because of them.
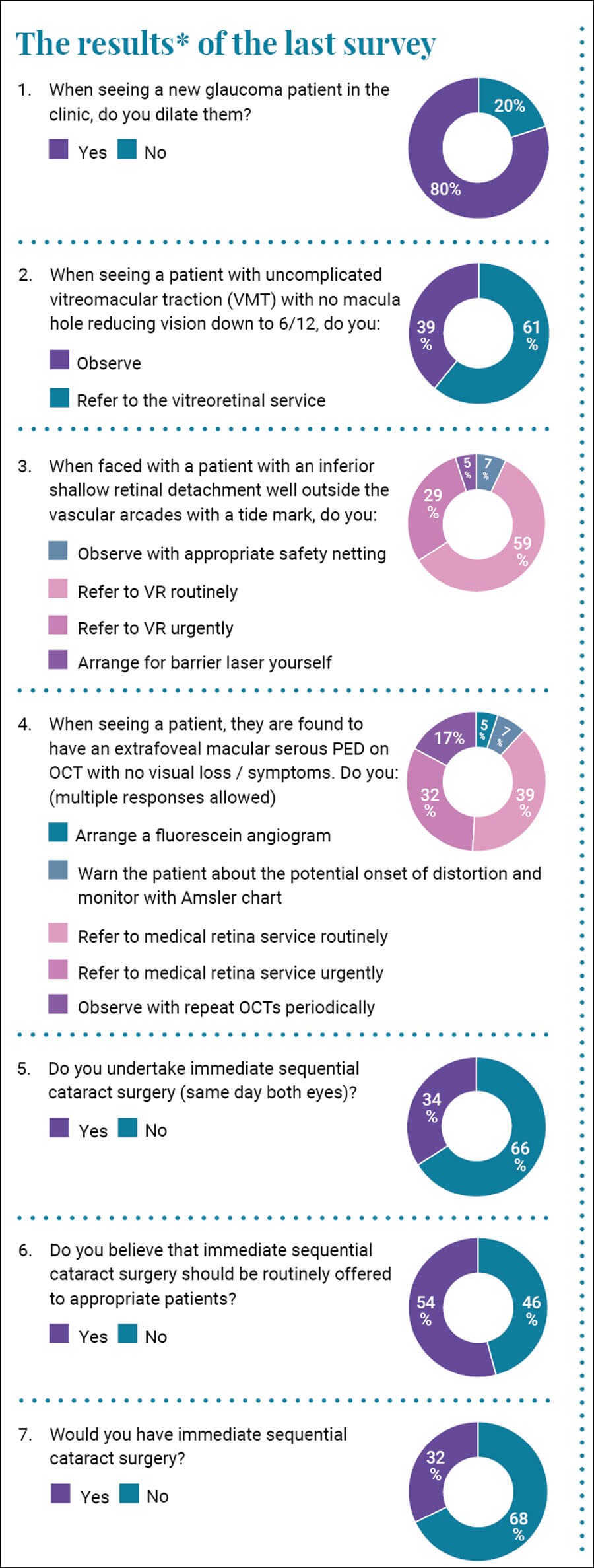
The first question relates to whether you use mydriasis when seeing a new glaucoma patient. I was surprised to see that one fifth of you did not. I would urge you to change your practice for the following reasons:
- You cannot fully assess the optic disc and detect signs of nerve fibre layer loss without dilatation as you do not get a true stereoscopic view. You will also miss optic disc haemorrhages.
- Often such patients may have or develop a visual field defect and we need to be able to exclude a retinal cause for it by examining the peripheral retina.
- And finally, because NICE tells you to; The NICE guidance published in November 2017, Glaucoma: diagnosis and management, states in Section 1.2 which relates to diagnosis requirements: “optic nerve assessment and fundus examination using stereoscopic slit-lamp biomicroscopy, with pupil dilatation.”
I have seen several cases where a patient was seen in a glaucoma clinic with a visual field defect with a referral querying glaucoma and then the field defect was found to be due to a non-glaucoma cause which was missed. Conditions such as retinal detachment and malignant melanoma were missed. This represents classical framing bias in that the patient is referred in with a glaucoma suspicion and potentially seen in a glaucoma clinic and the clinician is solely focused on confirming or refuting a diagnosis of glaucoma only to miss another more serious pathology.
The next question relates to a case scenario I see in my clinical work and less so in my medico-legal work. The question relates to a patient with 6/12 vision and vitreomacular traction (VMT). Clearly the clinical information is sparse and the real decision to refer or not will depend on how symptomatic the patient is and how motivated they are for surgical intervention, however we can get an indication of the split in opinion. I think that in most patients with 6/12 vision observation with sequential optical coherence tomography (OCTs) is the best route if we safety net and ask the patient to check their vision regularly. There is no specific guidance for ophthalmologists in the UK however there is guidance from the College of Optometrists and from the US indicating that in early VMT observation is sensible until surgical intervention is required.
We saw a divergence of opinion in the next question which relates to a clinical scenario we may all face. The hypothetical question relates to a patient with an inferior retinal detachment with a tide mark. This is theoretically a low-risk scenario. The inferior position of the detachment means that the likelihood of rapid propagation is minimal, and the tide mark would indicate it is long-standing and has stopped progressing. Seven percent of you would observe while 5% would apply barrier laser. Almost a third of you would refer to the vitreoretinal (VR) service urgently while 60% would refer on a routine basis. Who is right?
I see patients in the next clinical category frequently and was again surprised at how we vary in our decision-making. In a patient with an extrafoveal serous pigment epithelial detachment what would we do? We were surprisingly split in our opinions. Two thirds of you would refer to the medical retina (MR) service with half of you doing that urgently. Seventeen percent would observe with regular OCTs while 7% would discharge with an Amsler chart. I observe these patients with safety netting and repeated OCTs. They often resolve without any adverse sequelae. Seeing that two thirds of you refer to MR makes me question what I do. Am I incorrect in my management? I know I am not breaching my duty of care as a responsible body of medical opinion (the 17% of you who agree with me) would support me, but am I doing the best for the patient? I will reflect.
The next question refers to a topic which was controversial but now appears not to be so. I questioned whether you undertook immediate sequential bilateral cataract surgery (ISBCS) and was surprised to find that one third of you do. I recently presented at the Nottingham Eye Symposium and asked for a show of hands as to how many delegates undertook ISBCS. Out of an auditorium of several hundred people only two raised their hands. When I asked a follow-up question about whether the attendees would have ISBCS, only the two previous responders raised their hands. In response to our question, one third of you undertake it while two thirds do not. More than half of you think it should be routinely offered to patients. One third of you (presumably the same third who undertake the procedure) would have it themselves while two thirds would not.
I want to dislike the practice. I want to be able to cite the significant rate of bilateral endophthalmitis and say to the readership that even a one in 80,000 chance of bilateral endophthalmitis is not a risk I would be willing to take, however the evidence supports its safety. In a recent published study [1], the rate of postoperative endophthalmitis was assessed in a cohort of 5,573,639 IRIS Registry patients who underwent cataract extraction, 165,609 underwent ISBCS, and 5,408,030 underwent delayed sequential bilateral cataract surgery (DSBCS) or unilateral surgery (3,695,440 DSBCS, 1,712,590 unilateral surgery only). The confirmed endophthalmitis rates were 0.059% in ISBCS eyes and 0.056% in the DSBCS eyes, a difference that was not statistically significant. Odds ratios confirmed no statistical difference after adjusting for comorbid eye disease, age, sex, race and insurance status. Bilateral endophthalmitis was uncommon; seven cases were identified in the DSBCS group and none in the ISBCS group. So, there were more bilateral infections in the delayed group than in the same day group. Clearly the evidence supports its safety. I will still not be adopting it but I do apologise to ISCBS for the horrible things I have said about it.
There will be no survey for the next publication but instead I will share some of the lessons I have learned from my medico-legal practice.
References
1. IRIS® Registry Analytic Center Consortium. Endophthalmitis Rate in Immediately Sequential versus Delayed Sequential Bilateral Cataract Surgery within the Intelligent Research in Sight (IRIS) Registry Data. Ophthalmol 2022;129(2):129-38.
COMMENTS ARE WELCOME









