*Please be aware that this data does not form part of a peer reviewed research study.
The information therein should not be relied upon for clinical purposes
but instead used as a guide for clinical practice and reflection.
For the first time we have had some recurrent questions. I initially questioned you on the use of intracameral cefuroxime (ICC) in penicillin allergy back in 2019. I reiterated the questions in this survey to assess change. For certain issues I was surprised to see that very little had changed.
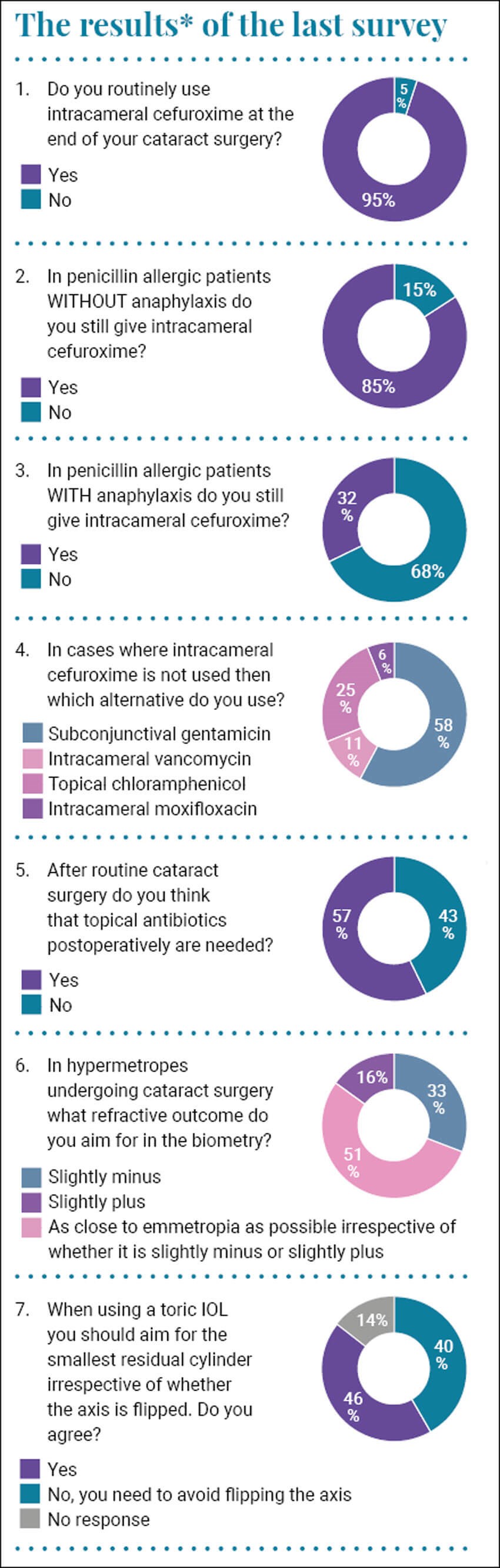
When questioned as to the use of ICC at the end of cataract surgery, 95% of respondents use it while 5% do not. This compares with 92.1% who said they used it and 7.9% who did not back in 2019. We seem to have managed to convince half of the respondents who did not use it back then into using it now. Whether you believe that it is a good thing, or whether you question the veracity of the ESCRS Endophthalmitis Study [1], and whether the findings can indeed be used as representative of your practice, the evidence is strong, and the layperson would find it hard to understand why it was not followed [1]. Thus, a judge may question if it was not used and endophthalmitis ensued. On the face of it not using it increases the risk of endophthalmitis five-fold.
When asked about the use of ICC in penicillin allergy 16% did not use it which compares with an almost identical 17.2% who said they did not use it back in 2019. Nothing seems to have changed which in itself is slightly concerning. When asked about the use of ICC in penicillin anaphylaxis one-third of you still use it which is unchanged to previously.
The original survey back in 2019 prompted some guidance from the Royal College of Ophthalmologists who published a Clinical Practice Point entitled “Intraoperative Antimicrobial Prophylaxis in Elective Cataract Surgery Patients with Penicillin Allergy” [2]. The recommendation is that if there is a confirmed or suspicion of possible anaphylaxis to penicillin then intracameral moxifloxacin should be considered as an alternative. If there is no confirmed anaphylaxis, then the recommendation is that ICC is used.
It is heartening that the work we are doing together has prompted a clinical recommendation, however it appears that the message has not really been received as the use of ICC in penicillin anaphylaxis is still at one-third. If a problem occurs in such a patient the defence of the position is hard as there is official guidance which the Claimant will point to. I believe that if guidance is issued every effort should be made to ensure it reaches the coalface clinicians who can then have the opportunity to implement a change in practice.
When an alternative antibiotic was used, only 6% used the recommended moxifloxacin. I tried to obtain intracameral moxifloxacin and was unable to. The only supply I could obtain was in one-litre bags as an infusion which was clearly not suitable for our cataract procedures.
When asked about using antibiotics in the postoperative period after cataract surgery 57% used them while 43% said they did not. I always give antibiotics, however my practice is not evidence-based. I think that our corneal wounds may not always be sound and may fish mouth particularly with a temporal approach. If there is potential ingress of ocular surface fluids I would rather they were sterile.
I was always taught to leave a patient on the myopic side after cataract surgery as hyperopic vision was “wasted vision”, and so I always did so. I found that some of the hypermetropes, particularly the younger patients, were unhappy as they have always used their small residual amount of accommodation to keep a sharp focus and when they had a permanent blur of slight myopia they resented it. Half of respondents aim for as close as possible to emmetropia regardless of plus or minus while 16% went for slightly plus and one-third went for slightly minus.
When questioned about the use of toric intraocular lenses (IOLs) and the postoperative axis 46% felt that flipping the axis was acceptable and that we should aim for the smallest residual cylinder irrespective of axis. Forty-one percent felt that flipping the axis should be avoided.
It is well established that when prescribing spectacles flipping the axis is not desirable, however there is some comment within the literature that the axis makes no difference when using toric IOLs. I read this and changed practice to simply aiming for the lowest cylinder irrespective of axis. I subsequently had a handful of cases who were unhappy with the visual outcome despite an excellent postoperative refraction. The only issue I could see was the flipping of the axis so now I have reverted to maintain the axis and accepting a fraction more residual cylinder.
As always, I am grateful to those who took the time to answer our questions.
References
1. ESCRS Endophthalmitis Study Group. Prophylaxis of postoperative endophthalmitis following cataract surgery: Results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg 2007;33(6):978-88.
2. Royal College of Ophthalmologists, Clinical Practice Point. “Intraoperative Antimicrobial Prophylaxis in Elective Cataract Surgery Patients with Penicillin Allergy”
https://www.rcophth.ac.uk/wp-content/uploads/
2022/07/Intraoperative-Antimicrobial-Prophylaxis
-in-Elective-Cataract-Surgery-Patients.pdf
Last accessed January 2023.
COMMENTS ARE WELCOME






