*Please be aware that this data does not form part of a peer reviewed research study.
The information therein should not be relied upon for clinical purposes
but instead used as a guide for clinical practice and reflection.
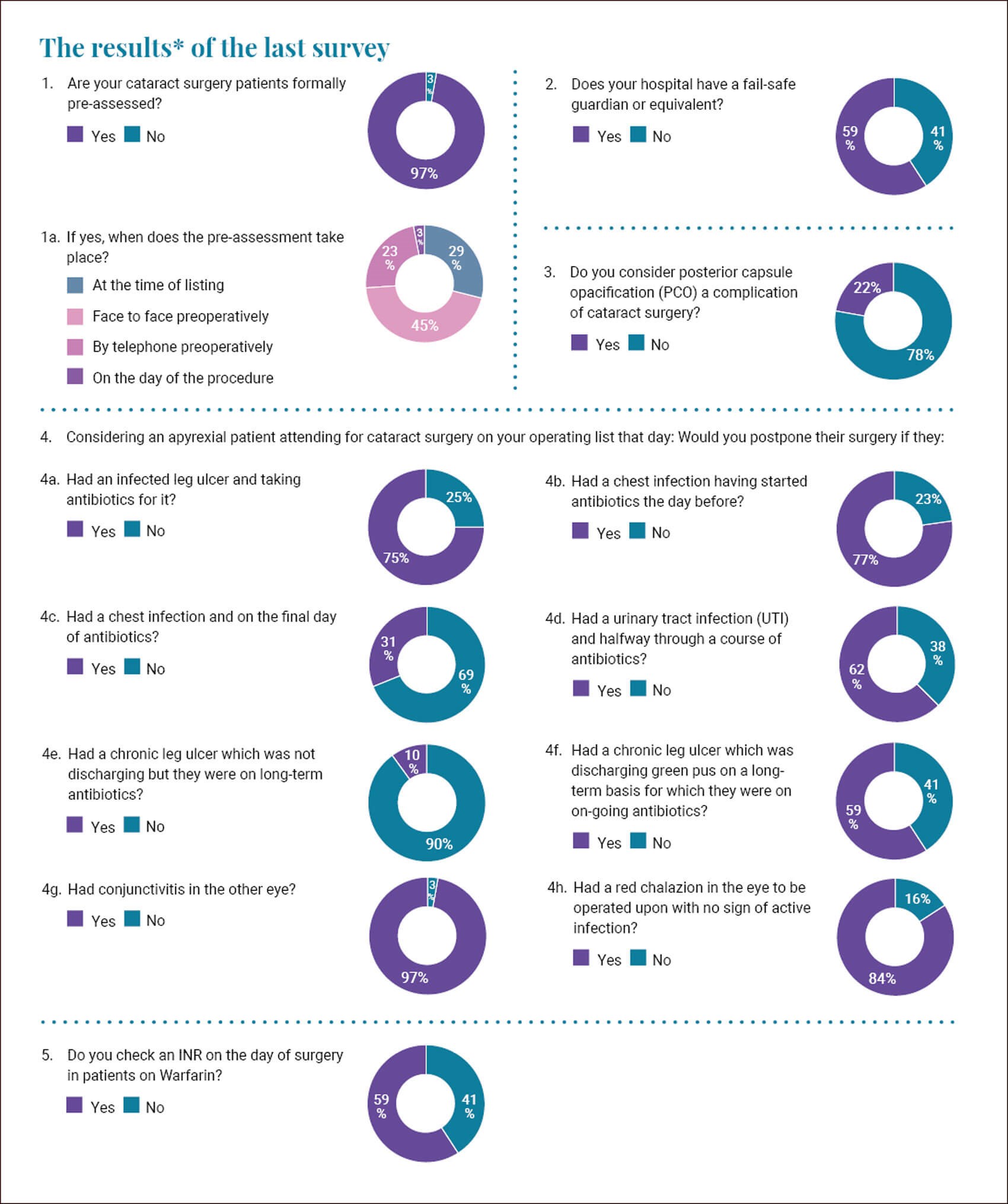
My thanks for all those who took part in our latest survey. I was relieved to see that the vast majority of your cataract patients are pre-assessed. I think this is important and has positive effects on optimising medical and ocular conditions for surgery, and also minimising the risk of cancellations on the day.
When asked when the pre-assessment took place and how it was done there was significant variability in practice. In 29% this happened at the time of listing, while in 45% of cases it was done face-to-face preoperatively. In 23% this occurred by telephone preoperatively and in the minority (three percent) this happened on the day of the procedure.
Clearly different hospitals and different units will have differing logistic issues in getting their patients pre-assessed, however I am always surprised that we cannot come to a consensus on what is the best way to do it. These practice variance surveys have highlighted that we do things differently and I hope we have had the opportunity to learn from each other. We do most of our procedures under topical anaesthetic or local anaesthetic so the need for a face-to-face assessment seems to be minimal. I like the idea of the telephone pre-assessment and then an upgrade to face-to-face if the initial screening detects issues.
When asked about a fail-safe guardian or equivalent I was relieved to see that 59% of you reported that you had one. In my medico-legal work I am always faced by scenarios where something slips through the net. Commonly this involves delays to appointments, cancellations, and failures to make appointments. There are always some specific failings but also systemic failings that could have been avoided. Having an individual who is devoted to spotting gaps in the net and addressing them seems a sensible, cost-effective, and safe barrier to clinical errors and harm.
When asked whether you consider posterior capsule opacification (PCO) a complication of cataract surgery I was surprised to see that 22% felt that it was. I consider a complication to be an adverse event or occurrence whereas PCO is simply a “normal” sequelae of cataract surgery in a large proportion of patients who have routine cataract surgery. I tell my younger patients that it is almost inevitable and despite polishing the posterior capsule diligently I still see it occurring after a few years. So, I do not believe it to be a complication. However, when I googled the definition of ‘complication’ I saw, under medicine, the definition “a secondary disease or condition aggravating an already existing one.” So maybe I and four out of five of you are wrong and PCO would meet the definition of a complication. You live and learn.
There were some interesting responses when we discussed an apyrexial patient attending for cataract surgery and what scenarios around infections would prompt a cancellation. I was surprised to see the variance in decision-making and I am sure a patient would also be surprised by it. It seems inherently unfair that a patient presenting to one unit with a chest infection may be cancelled while, if they attended a different one, the surgery would proceed.
We know that endogenous endophthalmitis can occur from an infective source elsewhere in the body. This typically involves patients who are severely debilitated or immunosuppressed. Arguably, by undertaking cataract surgery we are immunocompromising the eye. We also know that there is often a bacteraemia with any active infection. This means that we should be cautious about operating on patients with active infection.
Three quarters of you would cancel on the day if the patient had an infected leg ulcer and was taking antibiotics for it, while a quarter of you would proceed. I worry about this. I have had two cases whereby endophthalmitis occurred in this scenario. In one case the organism cultured from the ulcer was grown from the vitreous tap of the the post-operative endophthalmitis eye. I think that if the condition is reversible and we can optimise the patient then a delay of a few weeks against the theoretical risk of infective complication is worth it. There is a different scenario to the later question which refers to a patient with a chronic leg ulcer which is discharging green pus, for which they were on long-term antibiotics. In this latter situation the ulcer is not going to clear up and there is no hope to optimise the patient. Patients should be made aware of the slight theoretical increased risk of infection, as they need to make informed choices about their care. Fifty-nine percent of you would postpone, but I question how the patient will be any different at a later date.
When we look at the other scenarios presented, we can see that there is again significant variance when dealing with an active chest infection or a urinary tract infection. Our professional obligation is to keep the patient safe and away from harm. If we decide to proceed with cases, then it is vital that patients are involved in the decision process. I often prefer to err on the side of caution. Cataract surgery is an elective procedure, and a small delay until an infection clears seems to be a sensible option to consider.
Thankfully we have almost complete consensus on postponing if there is an active conjunctivitis in the other eye whereas we again have variance with the presence of a chalazion. A lot of it is about the perception of the patient and later the potential perception of the court. I know that a red chalazion is not really infected but I wonder whether, if that case developed a blinding infection, the claimant and the court would be critical of me operating on an eye which was already red and angry. Again, erring on the side of caution seems to make sense to me.
COMMENTS ARE WELCOME









