The first laser was created in 1960 and its name is an acronym for ‘light amplification by stimulated emission of radiation’. Laser technology has been used for medical, industrial, research and entertainment purposes in a variety of fields following extensive animal studies. The retina is most vulnerable to damage from lasers because visible and near-infrared light are focused and concentrated there.
Subretinal haemorrhage, retinal oedema, damage to the retinal pigment epithelium, vitreous or chorioretinal haemorrhage, perifoveal pigment changes or deposits, foveal ring-shaped hypopigmented lesions, and choroidal neovascularisation are among the retinal laser injuries that have been reported [1]. We report a unique case of macula laser burn from a reflected green laser.
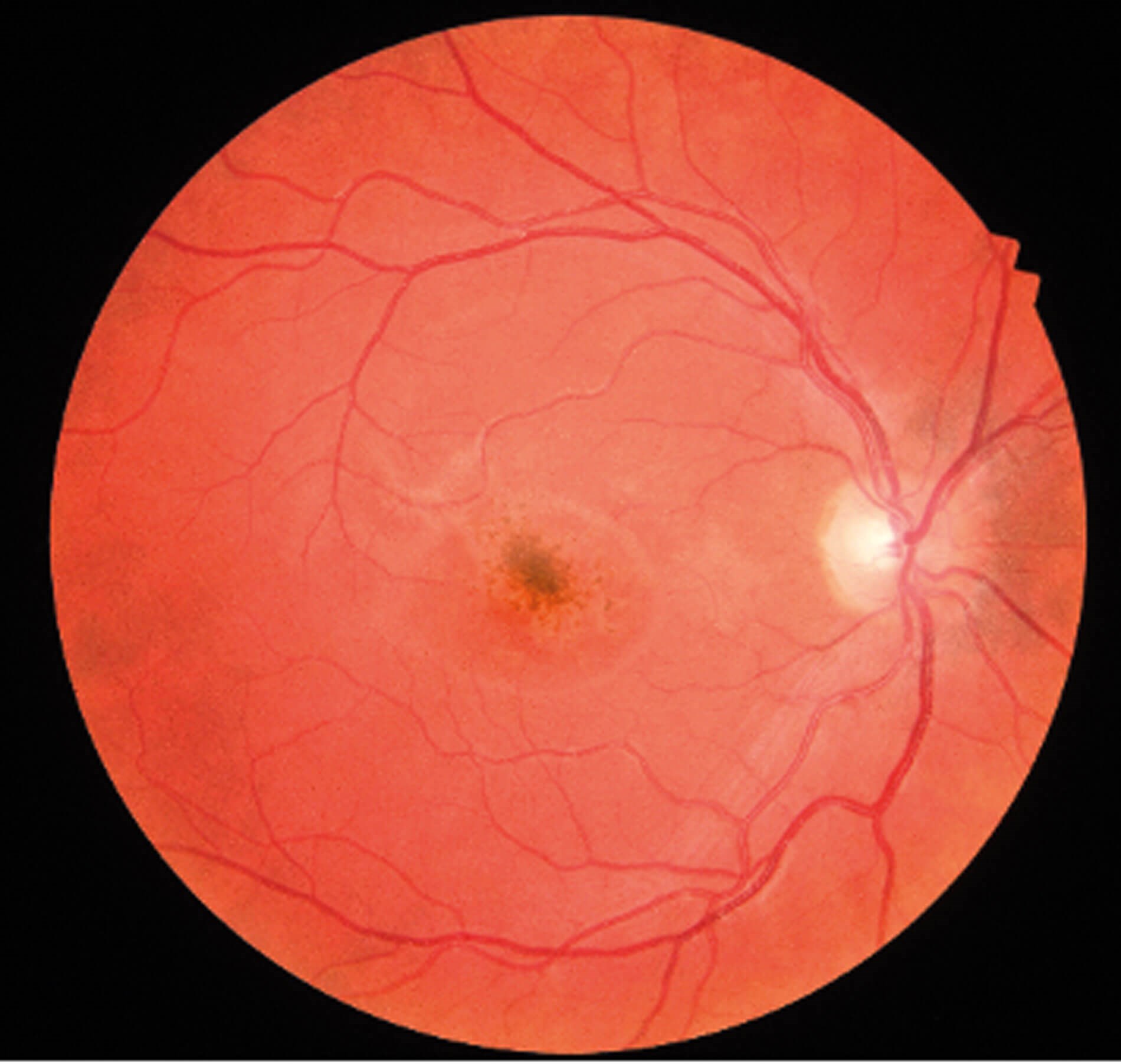
Figure 1: Right-eye (OD) fundus image showing pigmentary changes at the fovea.
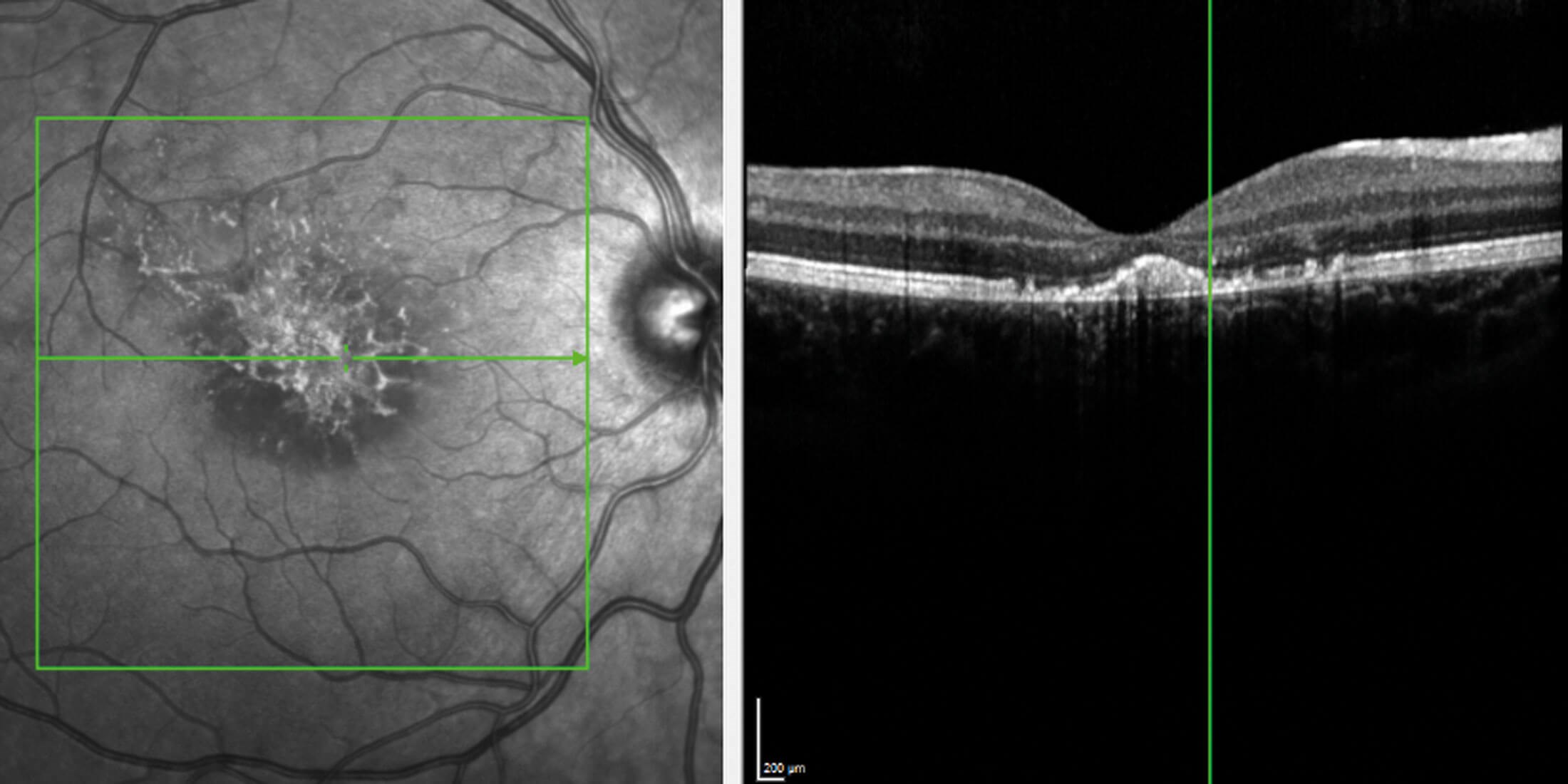
Figure 2: The ellipsoid zone is disrupted in the right macula by RPE loss that affects the umbo
and a concentration of focal hyperreflective material is visualised.
Case report
A healthy 16-year-old female with no significant past medical history presented to the emergency ophthalmology on-call service following right eye (RE) acute, painful decrease in visual acuity (VA) after pointing a green laser pen into her bedroom mirror. She mentioned that the laser of unknown class was recently purchased over the internet.
Visual acuity in the affected eye was 3/60 improving to 6/60 with pinhole. Her left eye (LE) was unaffected with VA 6/6. Pupils were equal and reactive to light and accommodation with no relative afferent pupillary defect detected. Intraocular pressures were within normal limits.
Fundal examination identified pigmentary changes at the central macula in both eyes. Spectral domain optical coherence tomography (OCT) of the LE initially showed foveal disruption of the outer retinal layers with hyperreflectivity.
The patient underwent further electrodiagnostic testing which demonstrated reduced pattern visual evoked potentials, pattern ERG and multifocal ERG in the RE when compared to the left.
Initial treatment was commenced with oral and topical steroids. Follow-up assessment after three months revealed minimal visual improvement with scarring at the macula.
Discussion
Eight categories – Class 1, 1C, 1M, 2, 2M, 3R, 3B, and 4 – make up the updated UK classification of laser products, with Class 4 lasers posing the greatest radiation risk [2]. Public Health England advises that a laser pointer should not be more powerful than a Class 2 laser. Consumer-oriented devices shouldn’t use Class 3B or Class 4 laser products due to the extent of harmful ocular damage they may pose. Permanent sight threatening injuries should be reported to Public Health England and the local authority for further investigation [2].
Handheld laser pointer retinal burns are a significant and rapidly rising public health concern. These gadgets are getting cheaper, more potent, frequently mislabelled, and simple to order online. In addition, concerns about aviation safety are growing after commercial airline pilots allegedly suffered retinal injuries from laser attacks were reported [3].
It is believed that children are more vulnerable to laser pointer injuries than adults because they are more fascinated by their appearance, lack the protective blinking and gaze aversion that adults display, and have clear ocular media that offer little protection from laser injury [4].
The majority of laser pointer injury cases that UK ophthalmologists encountered were reported to have involved online-purchased laser pointers. A recent review by Birtel, et al. involving 111 patients with laser pointer eye injuries discovered a wide range of retinal injuries such as macular holes, retinal haemorrhage, disruption of the retinal pigment epithelium on OCT imaging, and disruption of the outer retinal layers [5].
Management of this condition requires long-term monitoring for secondary complications. When treating patients who develop macular holes or ERM, it is important to consider the severity of the damage as well as the patient’s visual prognosis. Agents that block vascular endothelial growth factor can be used to treat choroidal neovascular membranes. Referral to a vision rehabilitation specialist may be considered if the extent of the damage is visually debilitating. Preventative counselling should be used in all cases to mitigate the risk of recurrence [1].
According to the literature, prognosis of laser pointer injuries is favourable, and many patients make a full recovery over several months [6]. However, those who have sustained serious injuries may experience scotoma or long-term visual deficits. Long-term outcomes are significantly worse for lasers with a power >5 milliwatts [7]. Several studies advocate the use of oral corticosteroids because it is believed to lessen the cellular inflammatory response brought on by the laser. However, larger studies are necessary to prove its clinical utility and efficacy [8].
Conclusion
There must be continued strict legal restrictions against the production, use, and possession of dangerous laser pointers. Laser safety education for the public is also essential to reduce the incidence of these injuries of which a larger proportion occur in people under 20 years of age [3]. This may be achieved by delivering teaching in schools and creating awareness through public health messaging.
References
1. Muslubaş IS, Hocaoğlu M, Arf S, et al. Macular Burns from Nonmedical Lasers. Turkish J Ophthalmol 2016;46(3):138.
2. Laser radiation: safety advice (2017). Public Health England (GOV.UK)
https://www.gov.uk/government/
publications/laser-radiation-safety
-advice/laser-radiation-safety
-advice#laser-classes
3. Linton E, Walkden A, Steeples LR, et al. Retinal burns from laser pointers: a risk in children with behavioural problems. Eye 2019;33:492–504.
4. Turaka K, Bryan JS, Gordon AJ, et al. Laser pointer induced macular damage: Case report and mini review. Int Ophthalmol 2012;32(3):293–7.
5. Birtel J, Harmening WM, Krohne TU, et al. Retinal Injury Following Laser Pointer Exposure: A Systematic Review and Case Series. Dtsch Arztebl Int 2017;114(49):831.
6. Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol 2000;44(6):459–78.
7. Torp-Pedersen T, Welinder L, Justesen B, et al. Laser pointer maculopathy – on the rise? Acta Ophthalmol 2018;96(7):749–54.
8. Lee GD, Baumal CR, Lally D, et al. Retinal injury after inadvertent handheld laser exposure. Retina 2014;34(12):2388–96.
[All links last accessed August 2023]
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME








