Central serous chorioretinopathy (CSCR) is a common retinal disease characterised by one or more serous neurosensory detachments. Patients present with acute onset blurring of vision, metamorphopsia and / or central scotomas.
The condition is six times more common in men than women and reportedly more prevalent in the Asia Pacific region [1]. In Asia the condition is also more aggressive and will more frequently present bilaterally or as multifocal CSCR [2]. Even so, more than 80% of CSCR presents in an acute manner and resolves spontaneously within three months. For these patients no treatment is required and the majority will recover their vision fully. Average final visual acuity for spontaneously resolving CSCR is 20/30 [3].
What can be done to avoid recurrences or accelerate remission?
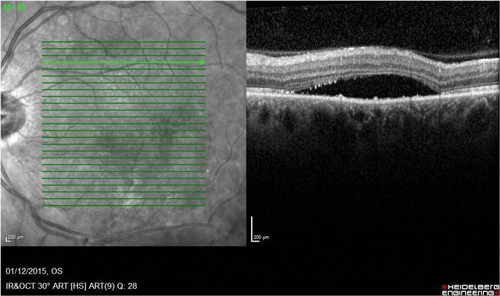
CSCR is associated with risk factors including type A personality, systemic steroid use and excess caffeine. Reducing sources of stress and caffeine intake and minimising or excluding exogenous steroid is advised (Figure 1).
Figure 1: Chronic CSCR in a patient treated with long-term exogenous corticosteroids.
What if the condition lasts more than three months?
Although CSCR is often self limiting, in some patients it may become chronic. If it lasts more than three months, treatment is recommended to avoid irreversible sight loss [4].
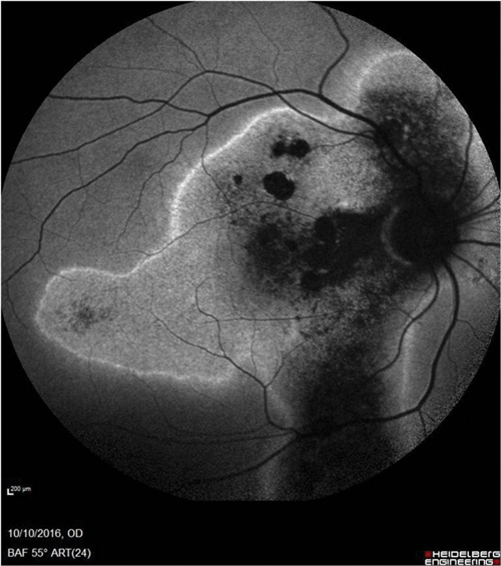
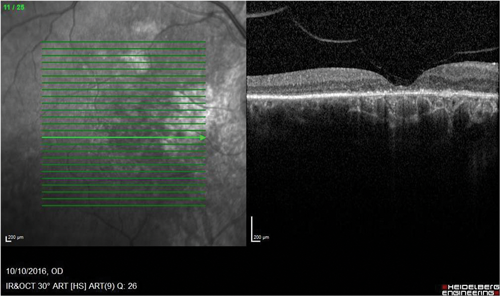
Figure 2: Consequences of chronic CSCR. (Top) Autofluorescence image of the right fundus showing widespread damage and atrophy of the retinal pigment epithelium and a ‘gravitational’ appearance. (Bottom) OCT scan of the same eye showing photoreceptor loss and RPE damage as well as abnormalities in the choroid.
Sight loss is due to photoreceptor damage and atrophy of the retinal pigment epithelium (RPE) (Figure 2). There are many different treatment options for chronic CSCR and no standard guidelines published on treatment protocols [5]. The treatment options range from systemic treatment to photodynamic therapy, as well as argon laser and micropulse laser treatment. Unlike other retinal conditions, anti-VEGF does not appear to be a useful treatment modality.
What is the role of systemic treatment and which therapies are available?
Although the pathogenesis of CSCR remains poorly understood, it is widely believed that overaction of the mineralocorticoid receptor is involved. For this reason, mineralocorticoid receptor antagonists have been successfully used to treat chronic CSCR. Spironolactone and Eplerenone have proven better than observation alone at treating chronic CSCR. A randomised control crossover study on the use of Spironolactone for chronic CSCR showed a statistically significant treatment effect with spironolactone as compared to placebo (p=0.04) [6]. Eplerenone has also shown encouraging results in non-randomised pilot studies to improve visual acuity (p<0.001) and reduce central macular thickness (p<0.01) with three months of treatment [7].
When would photodynamic therapy normally be considered?
Photodynamic therapy (PDT) works by causing short-term choriocapillaris hypoperfusion and long-term choroidal vascular remodeling, which reduces choroidal congestion, vascular hyperpermeability and extravascular leakage [8,9]. Multiple studies have now shown the long-term treatment efficacy of PDT for CSCR. A four-year retrospective review showed a mean gain of 8.7 letters with three quarters of patients gaining at least five letters [10]. Only four eyes (9%) had a reduction in vision and this was attributed to thinning of central macular thickness (CMT) and loss of IS/OS junction. PDT has, however, been associated with side-effects such as RPE rips and subretinal haemorrhage, which is a concern when treating CSCR patients with good pre-treatment visual acuity. For this reason, modified treatment protocols such as half dose, half fluence and half time PDT have been reported. A recently published retrospective review of 136 eyes in 123 patients treated with half dose PDT with long-term follow-up ranging from 36-96 months showed 97.1% of patients having complete resolution of subretinal fluid at final follow-up [11]. Recurrence of CSCR was reported in 6.6% of patients and a history of bilateral CSCR was significantly associated with recurrence. The same study also showed that baseline best corrected visual acuity (BCVA) was significantly associated with final visual acuity after treatment. The recommendations are therefore to treat CSCR in a timely manner before significant visual deterioration.
What about different PDT regimens?
Numerous published studies compare the different modified PDT treatment protocols. A randomised controlled trial (RCT) comparing half dose with half time PDT showed no difference in treatment efficacy or safety [12]. However, in a study by Uetani et al., with half dose PDT all patients have anatomical resolution of CSCR compared to only 33% with one third dose PDT [13].
Will patients respond to PDT?
Indocyanine green angiography is used to image the choroidal vasculature. In patients with CSCR, it is often observed that the choroid is hyperpermeable and this can be demonstrated on indocyanine green (ICG). The use of PDT is believed to be more efficacious in such patients.
What about standard laser treatment?
Argon laser photocoagulation has been reported to achieve resolution of CSCR but is also associated with a high complication rate of paracentral scotomas, contrast sensitivity loss, distortion and choroidal neovascularisation [14].
Where is the laser treatment directed?
Fundus fluorescein angiogram can be used to investigate CSCR and may show a focal leak (‘smoke stack’ or ‘ink blot’) throughout the run. If such a leak is demonstrated and if this is extra-foveal, then laser may be used. Complications are reduced if the site of the leakage is far away from the foveal centre.
Can the risks be minimised by the use of micropulse laser?
The risks of standardised laser have been significantly reduced with the advent of subthreshold micropulse laser (SML) treatment. SML delivers effective nondestructive treatment for both subfoveal and extrafoveal CSCR lesions with no significant retinal damage discernible postoperatively.
Is micropulse laser effective?
Micropulse laser delivers only 5% of the stimulus duration in a series of short rapid fire pulses. A number of case series have reported the safety and efficacy of diode laser (810nm) SML in CSCR and a large RCT (PLACE trial) comparing diode SML with PDT is currently recruiting patients [15]. A new wavelength of SML, 577nm yellow laser, reportedly has the advantage of superior absorption in the RPE layer over 810nm SML. Small case series have reported the use of yellow (577nm) to treat chronic CSCR but there are no RCTs planned to compare its treatment efficacy with that of 810nm SML or PDT to our knowledge.
Is there a role for combination therapy?
Whether mineralocorticoid treatment is as good as other treatments (PDT or micropulse laser) or may even have a synergistic effect with other treatments remains to be studied in future trials.
References
1. Tsai DC, Chen SJ, Huang CC, et al. Epidemiology of idiopathic central serous chorioretinopathy in Taiwan, 2001-2006: a population-based study. PLoS One 2013;8(6):e66858.
2. How AC, Koh AH. Angiographic characteristics of acute central serous chorioretinopathy in an Asian population. Ann Acad Med Singapore 2006;35(2):77-9.
3. Baran NV, Gürlü VP, Esgin H. Long-term macular function in eyes with central serous chorioretinopathy. Clin Exp Ophthalmol 2005;33(4):369-72.
4. Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol 2013;58(2):103-26.
5. Salehi M, Wenick AS, Law HA, et al. Interventions for central serous chorioretinopathy: a network meta-analysis. Cochrane Database Syst Rev 2015;(12):CD011841.
6. Bousquet E, Beydoun T, Rothschild PR, et al. Spironolactone for nonresolving central serous chorioretinopathy: a randomized controlled crossover study. Retina 2015;35(12):2505-15.
7. Bousquet E, Beydoun T, Zhao M. Mineralocorticoid receptor antagonism in the treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2013;33(10):2096-102.
8. Chan WM, Lam DS, Lai TY, et al. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol 2003;87(12):1453-8.
9. Pryds A, Larsen M. Choroidal thickness following extrafoveal photodynamic treatment with verteporfin in patients with central serous chorioretinopathy. Acta Ophthalmol 2012;90(8):738-43.
10. Silva RM1, Ruiz-Moreno JM, Gomez-Ulla F, et al. Photodynamic therapy for chronic central serous chorioretinopathy: a 4-year follow-up study. Retina 2013;33(2):309-15.
11. Lai FH, Ng DS, Bakthavatsalam M, et al. A multicenter study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol 2016;170:91-9.
12. Liu Y, Li L, Xu G, Wang W. [Observation on long-term efficacy of half-dose photodynamic therapy with chronic central serous chorioretinopathy using optical coherence tomography]. Zhonghua Yan Ke Za Zhi 2016;52(5):328-34.
13. Uetani R, Ito Y, Oiwa K, et al. Half-dose vs one-third-dose photodynamic therapy for chronic central serous chorioretinopathy. Eye (Lond) 2012;26(5):640-9.
14. Khosla PK1, Rana SS, Tewari HK, et al. Evaluation of visual function following argon laser photocoagulation in central serous retinopathy. Ophthalmic Surg Lasers 1997;28(8):693-7.
15. Breukink MB, Downes SM, Querques G, et al. Comparing half-dose photodynamic therapy with high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy (the PLACE trial): study protocol for a randomized controlled trial. Trials 2015;16:419.
COMMENTS ARE WELCOME