Aboriginal Australians have faced numerous challenges over the past centuries. Here in this article, Edward Saxton highlights why there are inequalities of ophthalmic care in Australia and why this has led to increased levels of blindness in Aboriginal people relative to non-Aboriginals. Saxton then explores the strategies that are in place to improve eye health outcomes.
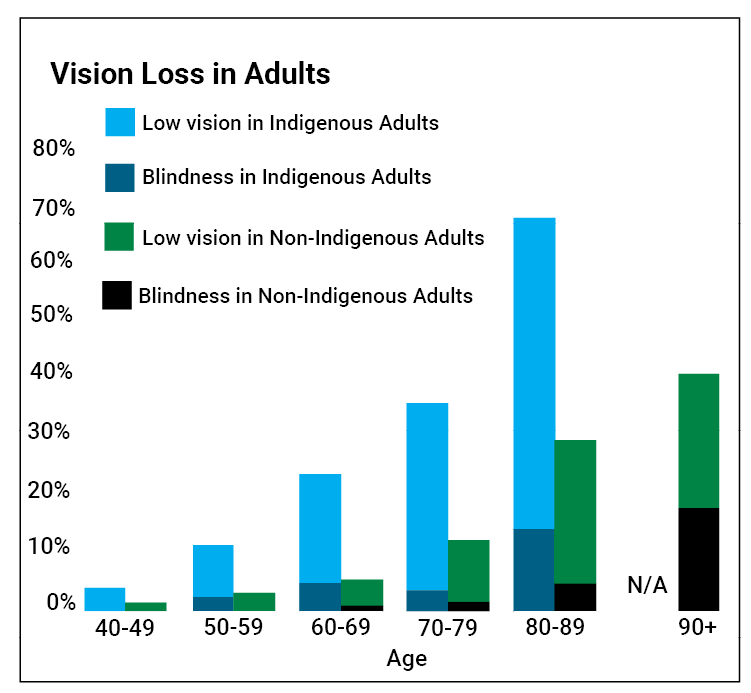 Figure 1: Vast disparities in quality of vision for Aboriginal vs. non-Aboriginal people [4].
Figure 1: Vast disparities in quality of vision for Aboriginal vs. non-Aboriginal people [4].
A brief history of Indigenous Australia
Aboriginal people have occupied Australia for at least 65,000 years and have the oldest living culture in the world. In its prime, there were more than 600 dialects spoken and they practiced traditional medicine with their knowledge of plants and herbs. Their approximate life expectancy was 75-80 years [1].
The colonisation of Australia by the British in 1788 had a devastating impact on Aboriginal people and severely reduced the population due to the introduction of disease (e.g., smallpox), massacres and removal from country. Aboriginal people were forced to live on government land and were banned from practising their culture. Aboriginal children were forcibly removed from their families in a design to assimilate Aboriginal children into the non-Aboriginal community. This is referred to as 'The Stolen Generation' [2].
These historical events have a strong impact on the health and wellbeing of Aboriginal people today. This intergenerational trauma also influences how the Aboriginal community interacts with the health services and the mistrust some Aboriginal people have of the Australian Government. Today, the average Aboriginal Australian’s life expectancy is eight years less than non-Aboriginal Australians. Leading causes of death include cardio-respiratory disease, diabetes and cancer [3].
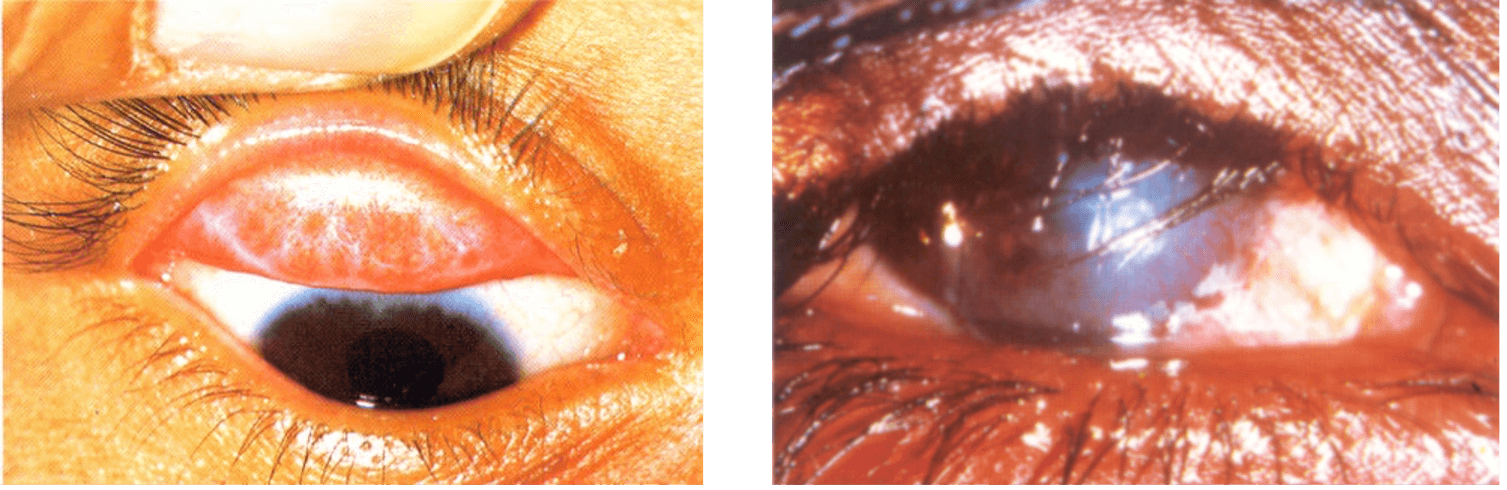
Figure 2: Pictured on the left is conjunctival scarring from repeated infection and on the
right one can see end-stage blinding trachoma with trichiasis and corneal opacities [6].
Aboriginal ophthalmic care
The National Indigenous Eye Health Survey was conducted in 2008 to better understand the magnitude, distribution and causes of vision loss in Aboriginal people [4]:
- Blindness is six times more common in Aboriginal Australians compared to non-Aboriginal Australians.
- 94% of the vision loss is preventable or treatable.
- Aboriginal children had better vision than non-Aboriginal children.
There are four main causes (accountable for 94%) of vision loss of which all are treatable [4]:
1. Refractive error
Only 20% of Indigenous adults wear glasses for distance compared to 56% of non-Indigenous adults.
2. Cataract
Blinding cataract is 12 times more common in Indigenous adults but rates of cataract surgery are seven times lower with the wait time for surgery being 50% longer than within the mainstream.
3. Diabetes
Thirty-seven percent of Indigenous adults have diabetes and 13% of these have lost vision. Ninety-eight percent of blindness from diabetes is preventable with early detection and timely treatment. Only 20% of Indigenous adults with diabetes had an annual eye exam and only 37% needing laser received it.
4. Trachoma
Trachoma will not be a disease known to many people in the UK, however it is a granulomatous conjunctivitis that affects many Indigenous people within remote communities. It is caused by the bacterium Chlamydia trachomatis and thrives in areas with poor hygiene and living conditions. Infection is usually acquired when living in close proximity to others with active disease. After years of repeated infection, the conjunctiva becomes scarred leading to entropion and subsequent trichiasis causing corneal damage. The resulting symptoms are ophthalmalgia and photosensitivity [5].
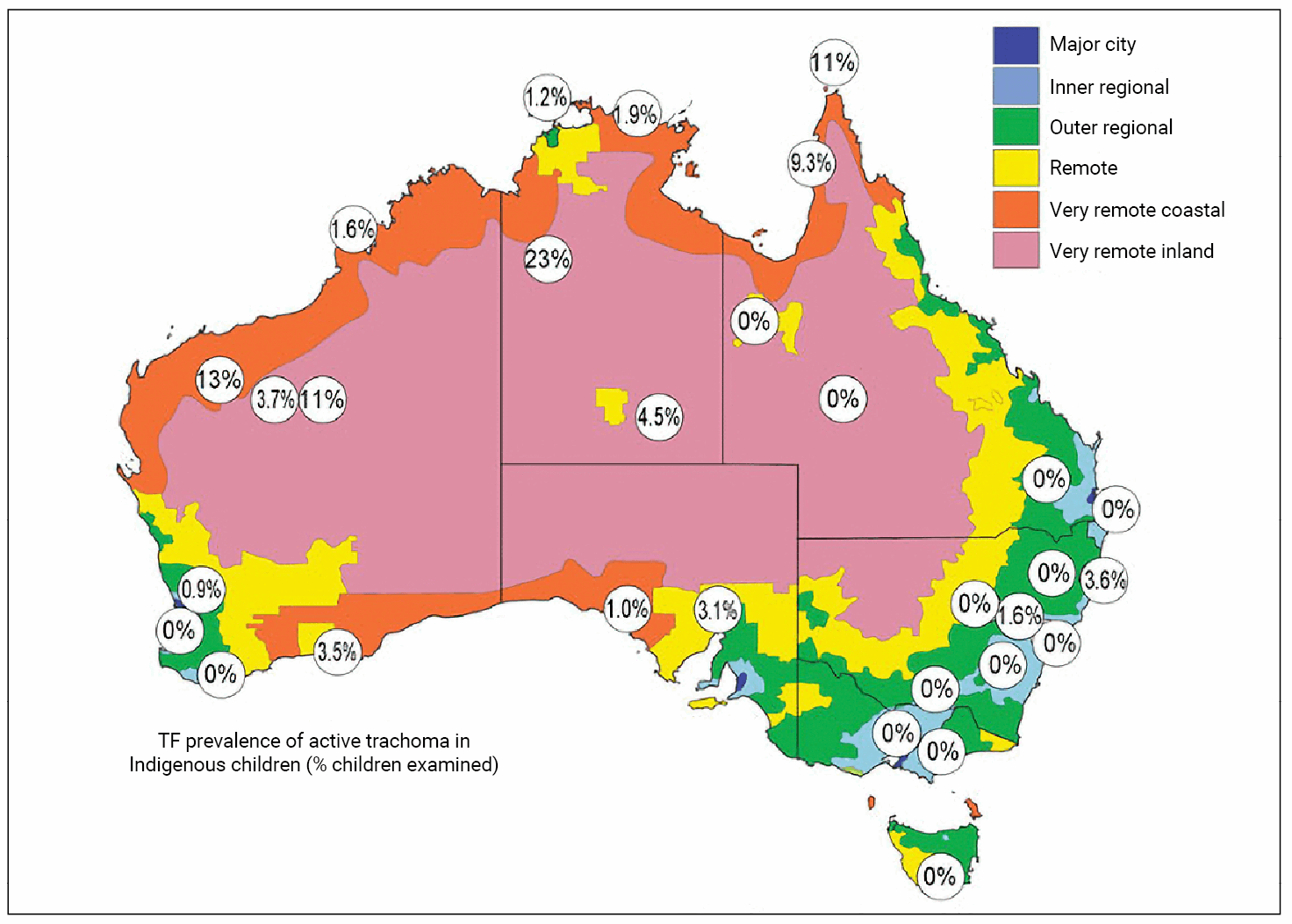 Figure 3: A map of Australia which shows the rates of active trachoma.
Figure 3: A map of Australia which shows the rates of active trachoma.
Higher rates are found in the most remote areas [7].
Australia is the only developed country worldwide to have trachoma. Blinding endemic trachoma occurs in 60% of outback communities. Late scarring and trichiasis affects 1.4% of older Indigenous people [4].
The World Health Organization (WHO) have introduced the SAFE strategy [5]:
- Surgery for trichiasis
- Antibiotic (azithromycin) treatment
- Facial cleanliness
- Environmental improvements (access to potable water).
In 2009 the Australian government committed to eliminating trachoma. Communities are screened, children are examined, treatment coverage has improved, and better infrastructure has been provided (installing washing sinks with clean water). With the SAFE strategy, trachoma rates have shown a marked decline as shown in Figure 4 [4].
I was fortunate enough to attend the annual Aboriginal and Torres Strait Islander Eye Health Conference to learn more about the processes in place to improve the ophthalmic services to Indigenous Australians. Here, I learned about the ‘Closing the Gap’ health campaign that was introduced to help improve healthcare equality for Indigenous Australians [8].
The Indigenous Eye Health Unit at the University of Melbourne laid out a plan titled ‘The Roadmap to Close the Gap for Vision’ in 2012. To this date there has been significant progress. The roadmap consists of 42 recommendations to improve ophthalmic care to remote communities.The recommendations in improving eye health care include [4]:
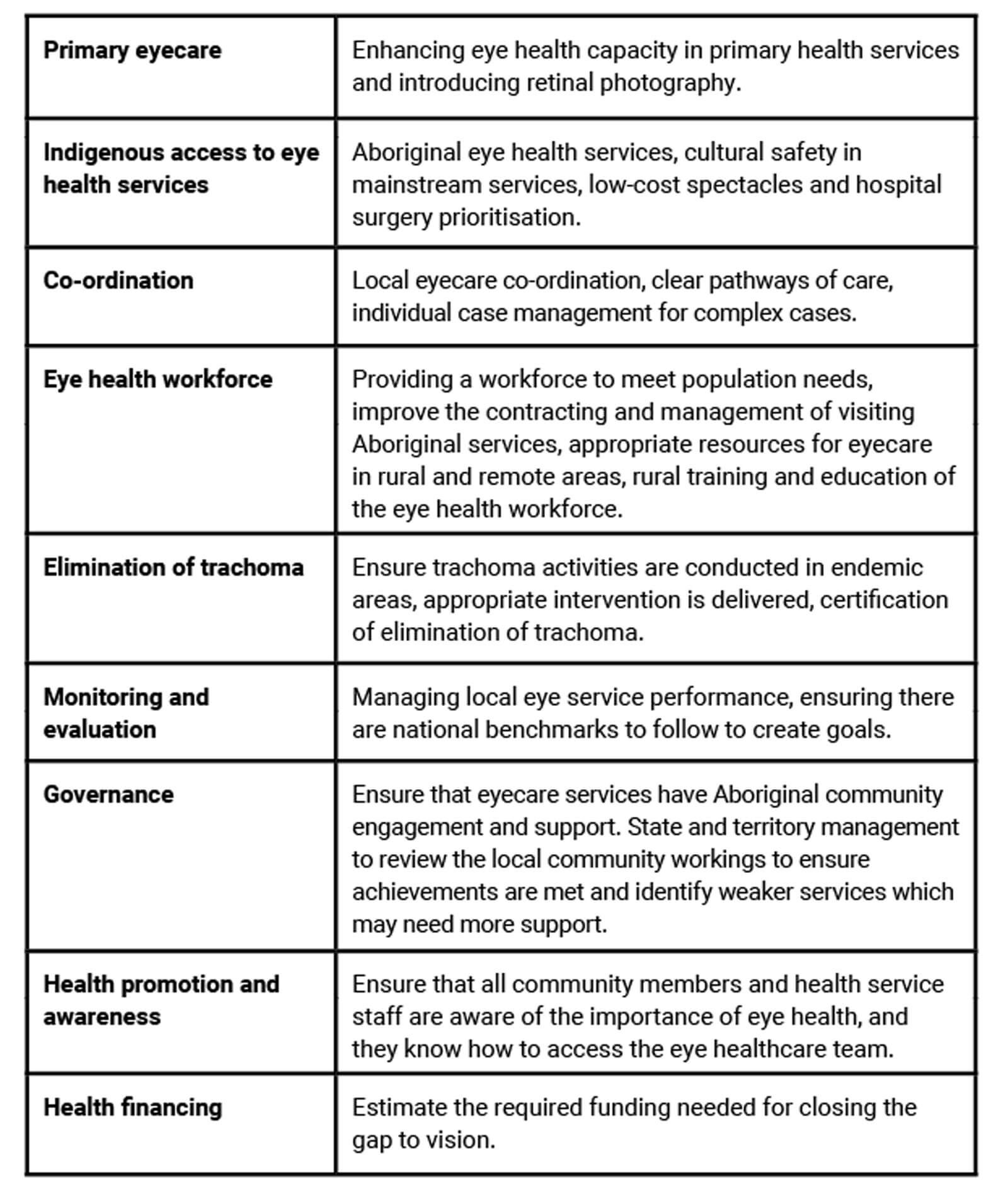
As of a 2021 survey, 27 of the 42 recommendations have been completed and the remaining 15 are making progress. Eye examinations have increased, as well as the number of cataract surgeries. However, the wait times to see an ophthalmologist have not improved when compared to non-Indigenous people.
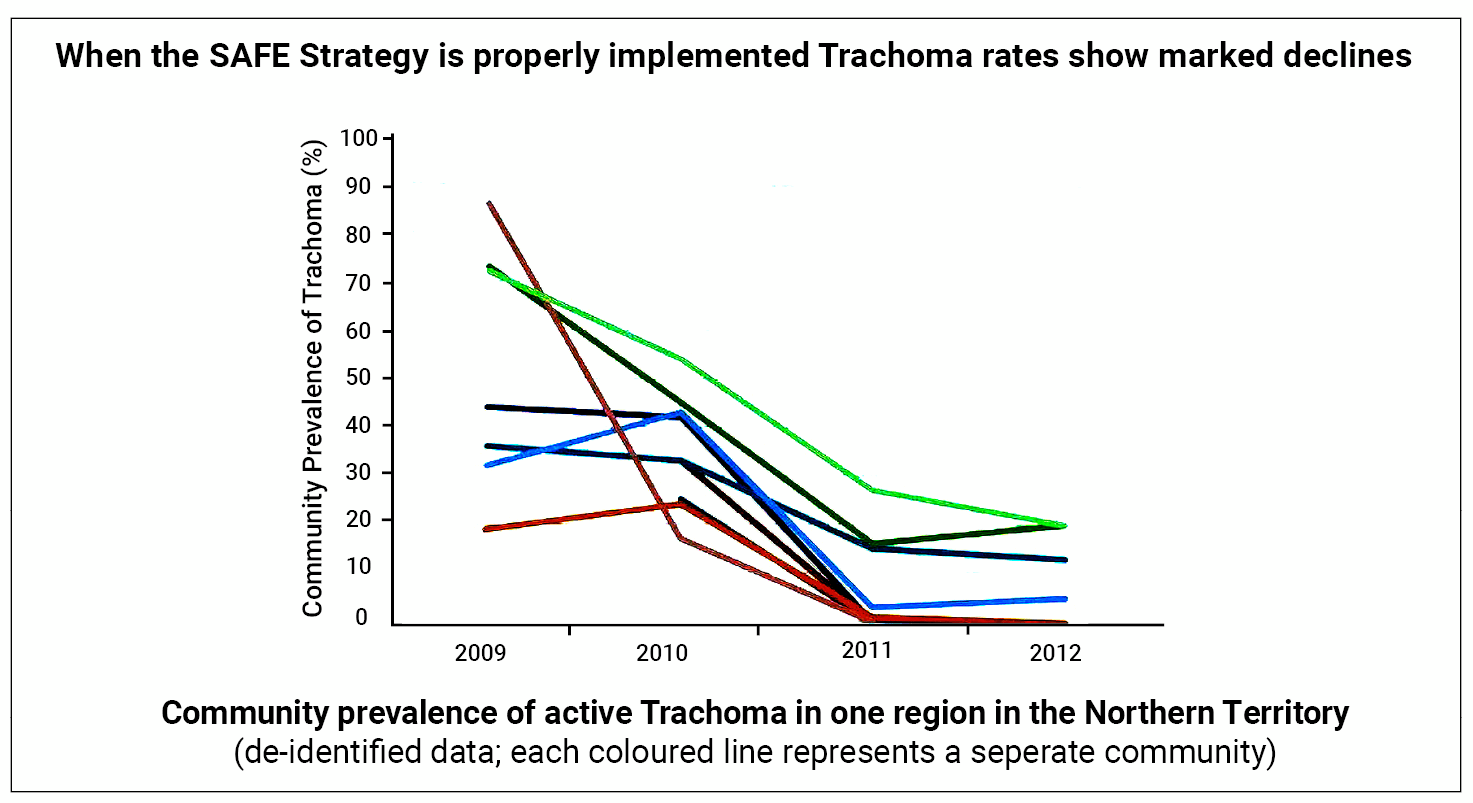 Figure 4: Reduction in trachoma rates following SAFE strategy implementation [4].
Figure 4: Reduction in trachoma rates following SAFE strategy implementation [4].
Overall, the conference was interesting and informative, especially having had little exposure to Aboriginal healthcare. I learned about the culture and how best to consult Aboriginal people in keeping with cultural safety and understanding. Furthermore, there was also a keynote about the ‘Yes’ campaign which was a national referendum on the voting for recognition of Aboriginal and Torres Strait Islander people in the constitution, through a voice to parliament [9].
“Blindness is six times more common in Aboriginal Australians compared to non-Aboriginal Australians. 94% of the vision loss is preventable or treatable"
It was interesting to understand in number how great the inequality is within a first world country, however in the past decade Australia has made huge steps to try to reduce the inequality. Thus far a lot of progress has been made by reducing rates of trachoma and increasing the number of ophthalmic examinations taken so hopefully this will continue until eye healthcare equality has been achieved. I hope that this article highlights some interesting issues for those that may potentially complete fellowships or consider training in Australia.
References
1. Berndt R, Tonkinson R. Australian Aboriginal peoples: References & Edit History (2017). Britannica.
https://www.britannica.com/
topic/Australian-Aboriginal
2. Colonisation 1788 - 1890. Working with Indigenous Australians FIRST NATIONS PEOPLE.
http://www.workingwithindigenousaustralians.
info/content/History_3_Colonisation.html
3. Closing the Gap Report: Life Expectancy (2020). Australian Government.
https://ctgreport.niaa.gov.au/
life-expectancy
4. Taylor HR, Boudville AI, Anjou MD. The roadmap to close the gap for vision. Med J Aust 2012;197(11):613-5.
5. Trachoma (2022). World Health Organization.
https://www.who.int/news-room/
fact-sheets/detail/trachoma
6. Diagnosing Trachoma (2016) International Trachoma Initiative.
https://www.trachoma.org/
slideshow/diagnosing-trachoma
7. Taylor H, Fox S, Xie J, et al. The prevalence of trachoma in Australia: The National Indigenous Eye Health Survey. Med J Aust 2010;192(5):248-53.
8. Closing the Gap.
https://www.closingthegap.gov.au/
9. Yes23.
https://www.yes23.com.au/
[all links last accessed September 2023]
TAKE HOME MESSAGES
-
Ophthalmic care in Australia is worse for Aboriginal people compared to non-Aboriginal people.
-
Ophthalmic care is not prioritised the same in remote communities and a lack of cultural safety deters Aboriginal people from seeking healthcare.
-
The ‘Closing the Gap’ campaign has vastly improved the delivery of ophthalmic care to the Aboriginal community with the aim of having equal treatment of care by 2025.
Declaration of competing interests: None declared.







