The author looks at the increasingly significant role of medical ophthalmologists and the importance of integrative healthcare.
The eye is a remarkable organ, and for decades we have been discovering intimations of pathology existing elsewhere in the body [1] simply through observing signs in the eye. There is no dearth of diseases which can affect the eye in myriad ways [2], and the medical ophthalmologist (ophthalmic physician) operates at the interface between eye disease and systemic medicine in both children and adults.
In these instances, a physician’s approach and training can be crucial in investigating and managing both the systemic (full body) problem and the eye, and to ensure that patients receive integrated care. Bestriding hospital ophthalmology, inpatient and outpatient medical care and the community, the medical ophthalmologist is crucial in bridging the diagnosis and management of complex patients. Therapeutic options can be very effective, and in some cases the need for potentially risky surgery can be avoided. The UK is unique in being the only country in the world which provides specialised training in this specialty.
Expertise in not only ophthalmic medicine, but the systemic specialties, is a fundamental part of medical ophthalmology [3], whether neurology, rheumatology, respiratory medicine, cardiology, infectious disease, gastroenterology, endocrinology, haematology, nephrology, dermatology, or any other specialty within medicine. Examples of diseases include uveitis, scleritis, thyroid eye disease, lung diseases, strokes, brain inflammation, pituitary diseases, vasculitis, rheumatoid conditions, infections, cancers, bowel and skin problems, vascular diseases such as high blood pressure and diabetes, genetic diseases and all the complications relating to these conditions. Often the disease is not identified, and the medical ophthalmologist has to put together the clues.
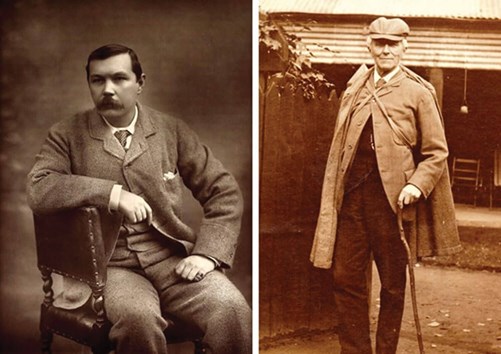
Figure 1: Left: Arthur Conan Doyle. Photographed by Herbert Rose Barraud, 1893.
Right: Joseph Bell in deerstalker. From the collections of The Royal College of Surgeons of Edinburgh.
Sir Arthur Conan Doyle’s most renowned sleuth, Sherlock Holmes, was famously based on a real-life physician detective, Joseph Bell [4]. The medical ophthalmologist embodies the Holmes approach to pick up the cross-disciplinary clues, and unravel the mystery in patients who have been previously undiagnosed, or whose medical problems might straddle different specialties. In many cases, taking the patient’s history and listening to their story is crucial. Hints can be obtained, and a diagnosis made, before even looking at the eye.
“You mustn’t touch him. Use your eyes, sir, use your ears, use your brain, your bump of perception, and use your powers of deduction.”
Joseph Bell, 1837-1911.
There is tremendous satisfaction to be gained when fitting the jigsaw pieces together and finally diagnosing a disease, especially for patients who may have struggled to be diagnosed. Whilst talking to the patient, the ophthalmic physician will be assessing the patient from a full-body perspective, never taking anything for granted.
“It is a capital mistake to theorise before you have all the evidence.”
Sherlock Holmes, created by Arthur Conan Doyle 1859-1930.
The advent of artificial intelligence has brought about new insights into how the eye can be a window into full-body diseases, with the findings that features in retinal scans can signal present cardiac health, as well as future risk of heart disease [5]. This burgeoning field of oculomics [6] bestrides the complex disease relationships, and the medical ophthalmologist will have a key role in interpreting and acting on these new rivulets of information.
“Interfacing between hospital ophthalmology, inpatient and outpatient medical care and the community, the medical ophthalmologist is crucial in bridging the diagnosis and management of the complex patient”
At the core of medical ophthalmology is the tenet that each patient case presents individually, and the reasons why a condition has manifested in the eye and the body can have many factors. When eye inflammation is the first sign of a body condition, it is crucial that the whole patient is investigated and treated, not just the eye. Treatment incorporates the overall health and wellbeing of the patient, and amongst the most enjoyable aspects of the job is getting to know patients over time. Teamwork with colleagues in ophthalmology, the medical specialties and the community is paramount to bring about the best outcomes for patients.
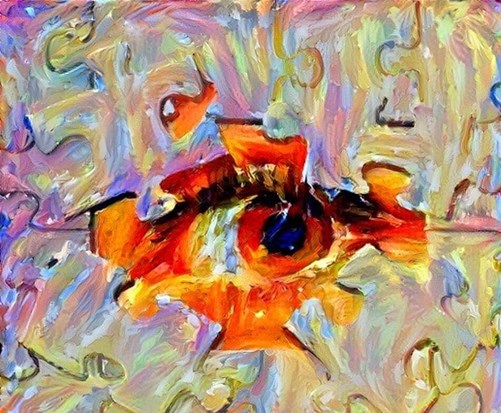
Figure 2: The eye can solve the jigsaw puzzle. Credit: own artwork (Nima Ghadiri).
Medical ophthalmology training
“I have ventured to say that a considerable part of the field of clinical ophthalmology requires not the art and craft of the surgeon, but the diagnostic and therapeutic methods of the physician.”
Dr CA Hawthorne, 1919 [7].
The Royal College of Physicians, alongside the Royal College of Ophthalmologists, established a training programme for medical ophthalmology in 1995, harkening back to the early 20th century desire for a clinician who is “skilled in ophthalmic medical diagnosis, in relating systemic medical disease to ophthalmic conditions, in assessing the general medical status of patients who have primary ophthalmological disease, and in prescribing the most appropriate drug therapies and monitoring schedules for treatment of medical sight threatening diseases” [8].
In 2014, the Centre for Workforce Intelligence recommended a graduated increase in the number of medical ophthalmology training places, aiming for one specialist per every 263,000 people [9]. Currently, trainees may enter the five-year training programme from either ophthalmology or the Internal Medical Training pathways at ST3 level, yielding specialists who are experts in both ophthalmic and systemic medicine. For further information, please read below:
Further Reading
-
https://www.jrcptb.org.uk/specialties/
medical-ophthalmology -
https://www.st3recruitment.org.uk/
specialties/medical-ophthalmology -
https://www.healthcareers.nhs.uk/
explore-roles/doctors/roles-doctors/
medicine/medical-ophthalmology -
https://www.rcplondon.ac.uk/
education-practice/advice/specialty
-spotlight-medical-ophthalmology -
http://careers.bmj.com/
careers/advice/A_career_in
_medical_ophthalmology
TAKE HOME MESSAGE
-
The eye provides us with a view of the nerves and blood vessels in the body.
-
There are many clues in the eye which can help us uncover medical mysteries elsewhere in the body.
-
Medical ophthalmologists (ophthalmic physicians) are specialists who are trained in both the eye and full-body medicine.
-
The medical ophthalmologist can have a key role in eye clinics and hospitals worldwide, linking the eye and systemic disease, particularly with the dawn of AI-augmented practice and increasingly personalised medicine.
References
1. Sacks JG. Eye disorders: Looking at the eye for clues to systemic disease. Postgrad Med 1976;59(3):181-4.
2. Cordes FC. Ophthalmology: Medical Ophthalmology. Cal West Med 1927;27(1):90.
3. Whitcup SM. The Eye In Systemic Disease. Arch Ophthalmol 1991;109(4):478-9.
4. Harnagel EE. Joseph Bell, MD.; the real Sherlock Holmes. N Engl J Med 1958;258(23):1158-9.
5. Wong TY, Klein R, Nieto FJ, et al. Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case–control study. Ophthalmology 2003;110(5):933-40.
6. Wagner S, Fu DJ, Faes L, et al. Insights into Systemic Disease through Retinal Imaging-Based Oculomics. Transl Vis Sci Technol 2020;9(2):6.
7. Discussion on Mr Rayner D Batten’s Paper, “The Need of Ophthalmic Physicians for the Advancement of Ophthalmology”. Proc R Soc Med 1920;13(Sect Ophthalmol):18-27.
8. Dick AD, Forrester JV. The ophthalmic physician: an indulgence or a necessity? Br J Ophthalmol 1996;80:782-3.
9. Centre for Workforce Intelligence. Securing the future workforce supply: medical ophthalmology stocktake. Feb 2014:
http://webarchive.nationalarchives.gov.uk
(Last accessed December 2021).
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME









