I am a former orthoptist, now trained in medicine and working as a foundation doctor. In my previous work, I was frequently approached by ophthalmology trainees eager for guidance with strabismus and ocular motility.
Drawing on my clinical experience, I have written this overview to help demystify these notoriously complicated topics. This article will introduce some of the theory behind our extraocular muscles and provide practical tips on how to excel at this aspect of the ophthalmic examination.
By providing the reader with a base level of understanding of strabismus and ocular motility, I hope to demonstrate that strabismus and ocular motility need not be perceived as cryptic and complicated, but as a fascinating space where neurology and ophthalmology collide.
Key concepts
Strabismus
1. Manifest vs. latent
Strabismus is categorised as manifest (-tropia) or latent (-phoria). Manifest strabismus involves an abnormal deviation of one eye during fixation, detectable with a cover-uncover test (CT). Latent strabismus cannot be detected by CT or when both eyes are open, as it is a combined deviation of both eyes, present only when fusion is disrupted. It is uncovered with an alternating cover test (ACT) which causes the eyes to become dissociated.
2. Concomitant vs. incomitant
Strabismus is further classified by its relationship to the ocular movements, whether normal or abnormal. Concomitant strabismus features normal ocular movements, and an equal angle of deviation no matter which eye is used for fixation. Incomitant strabismus occurs in the presence of ocular movement limitation. It is characterised by an increasing angle of deviation as the eyes are turned in the direction of the limitation. The angle of deviation will differ depending on which eye is fixating, with a larger angle when fixating with the affected eye. Neurogenic, myogenic, and mechanical causes of strabismus lead to incomitant strabismus.
Ocular motility
1. Extraocular muscle actions
Each extraocular muscle (EOM) exhibits anatomical primary, secondary, and tertiary actions. For example, the superior oblique muscle primarily depresses the eye, but also contributes to abduction and incyclotorsion. However, clinically, the superior oblique muscle function is tested in an inferior-nasal position, which seems to contradict its secondary function of abduction. In fact, the anatomical actions describe the hypothetical action of each muscle if it were acting in isolation. In reality, the other EOMs are also exerting tension on the eye, and therefore the eye movement is tested in the direction where that muscle is most active when all six muscles are operational.

Figure 1: OM diagram depicting full ocular movements of all EOM.
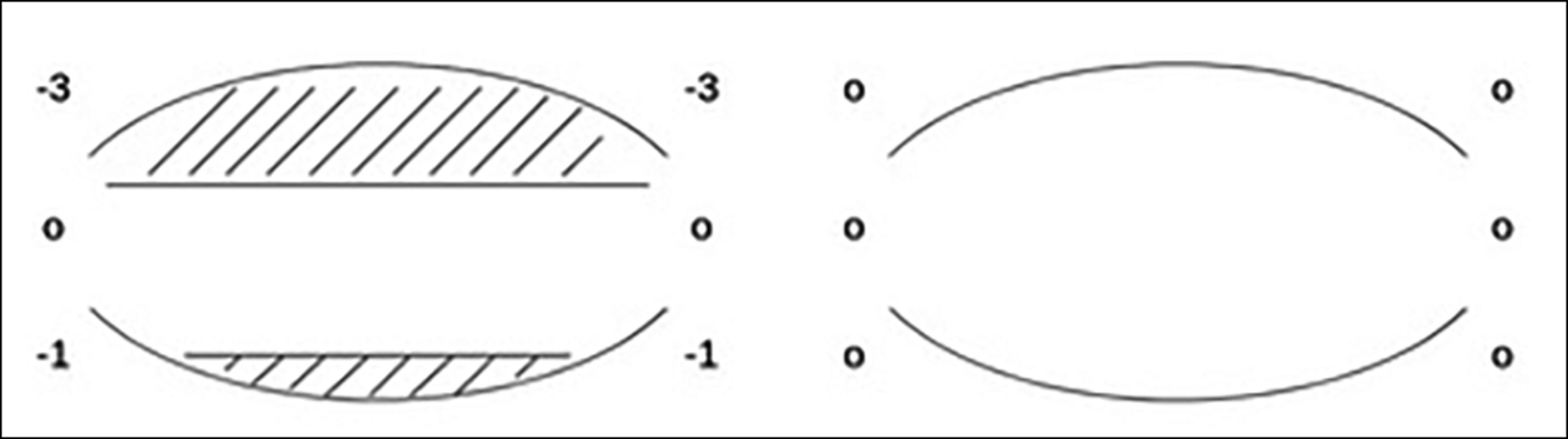
Figure 2: OM diagram depicting mechanical restriction of elevation, and depression
to a lesser extent, as seen in a case of orbital floor fracture.
2. The ocular motility diagram
Ocular motility (OM) diagrams are one method of documenting eye movements. Both eyes are represented from the perspective of the examiner. Six testing areas for each eye are recorded, each representing one EOM as described above. Full movement is depicted with a score of 0. Limitation of any movement is graded in increments of 25% from 1-4, with 4 denoting no movement beyond the midline. The addition of hatching indicates mechanical restriction of muscle (i.e. duction limited in addition to version), whereas minus numbers without hatching indicate muscle underaction (See Figures 1 and 2).
3. Ductions and versions
Version describes the range of movement when both eyes are open. Dextroversion and laevoversion describe movement to the right and left respectively, which are suffixed with -elevation or -depression when also moving upwards or downwards – e.g. laevodepression when the eyes are directed downwards and to the left.
Duction is tested by occluding one eye and assessing the uniocular range of movement of the other. It is normal for ductions to be slightly greater than versions. When a limitation of movement is seen, testing ductions can help differentiate between neurogenic and mechanical strabismus. A limitation seen in versions that improves on duction suggests neurogenic strabismus.
4. Alphabet patterns
Alphabet patterns are OM patterns occasionally seen in strabismus, denoting significant horizontal strabismus changes in up-gaze compared to down-gaze. Two common types of alphabet patterns are ‘V’ and ‘A’ patterns, which can occur in both exotropia and esotropia. The choice of letter used helps to describe the phenomenon seen. In V patterns, the eyes are relatively more diverged on up-gaze, and relatively converged on down-gaze, with a >15Δ difference in deviation size [1]. An A pattern is present when the eyes are relatively converged on up-gaze and diverged on down-gaze, with a >10Δ difference [1]. They are depicted on OM diagrams with two slanting lines, in an approximate V or A shape (Figure 3).
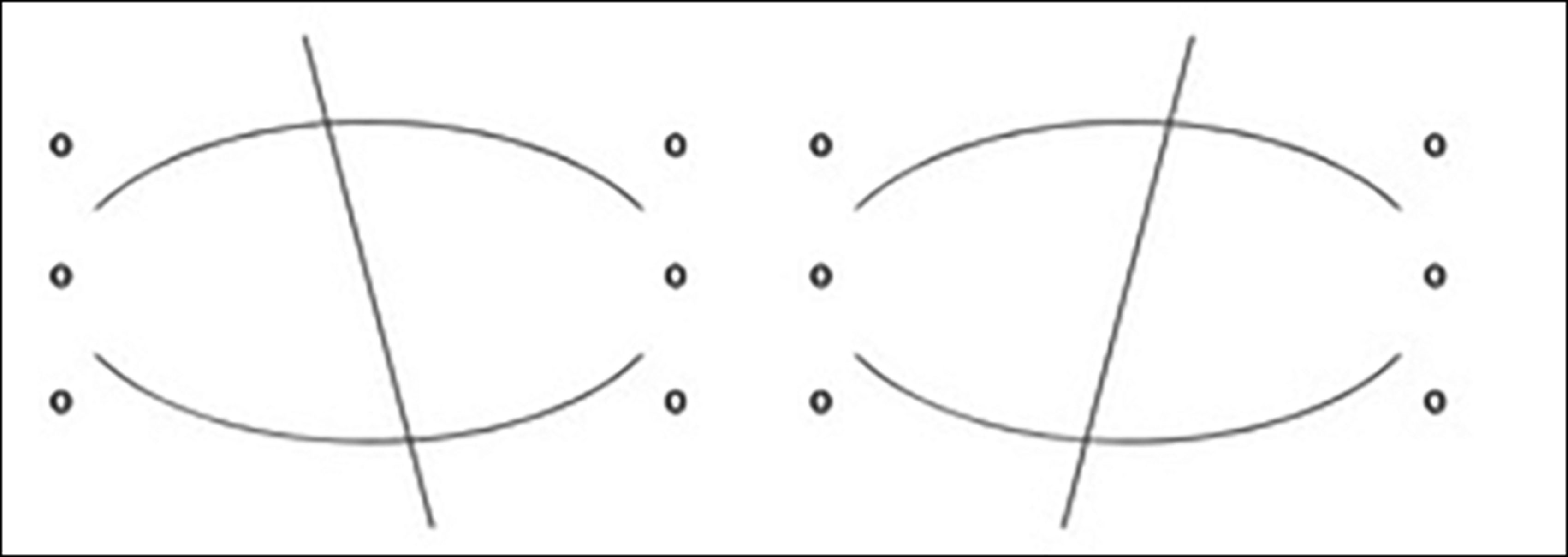
Figure 3: OM diagram depicting presence of a V pattern. Inverted lines would indicate A pattern.
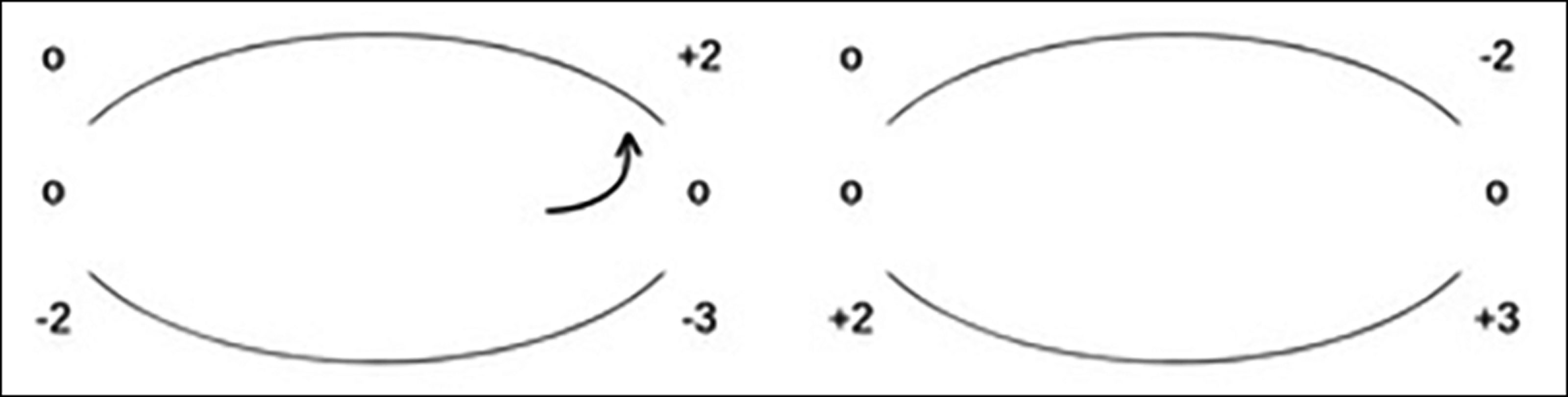
Figure 4: OM diagram depicting a typical case of fourth nerve palsy.
The underacting right eye superior oblique leads to development of muscle sequelae.
An arrow indicates that the right eye upshots when moving into adduction.
Alphabet patterns can be caused by abnormalities of vertical or horizontal muscle action, anatomy, or muscle insertion. Cosmetic concerns can be addressed surgically with augmented techniques such as vertical muscle recessions, or minimal vertical transpositions of horizontal muscles [2].
5. Overactions and underactions
Hering’s law is crucial in understanding muscle under- and overactions. It states that a contracting muscle and its synergistic muscle in the contralateral eye receive equal and simultaneous innervation [3]. It means that when a muscle underacts due to weakness or restriction, the contralateral synergist overacts. On the OM diagram, underactions are represented from –1 to –4, and overactions from +1 to +4. Although the effect also occurs in horizontal muscles, it is only recorded for vertical muscle actions. Arrows denote upshoots or downshoots of an eye on horizontal gaze, due to significant underaction of a vertical muscle.
6. Muscle sequelae
A pattern of muscle overaction and underaction seen in incomitant strabismus, which sequentially develops after onset. Sherrington’s law of reciprocal innervation is required to help understand this phenomenon, stating that when a muscle receives increased innervation, decreased innervation is directed to its ipsilateral antagonist [3]. Muscle sequelae follows the initial weakness of one EOM in the following order:
- Overaction of the contralateral synergist (Hering’s law)
- Overaction of ipsilateral antagonist (Sherrington’s law)
- Underaction of contralateral antagonist (Hering’s law and Sherrington’s law).
Practical tips
This section provides practical tips to aid trainees with detection and assessment of strabismus and OM abnormalities. Trainees may have already encountered orthoptic notation and abbreviations, for more details on how to decipher an orthoptic report, please refer to this excellent article www.eyenews.uk.com/education/top-tips/post/making-sense-of-the-orthoptic-assessment
Testing for strabismus
- Corneal reflections: Begin by directing a penlight at both eyes simultaneously. Normally aligned eyes should each produce symmetrical corneal reflections. Asymmetry may indicate misalignment, requiring further assessment.
- CT / ACT: Two simple tests which can reveal so much! Perform in primary position, with and without glasses. Ensure rapid occluder movement to maintain eye dissociation.
- Testing in different gaze positions: A complete examination also entails testing in horizontal and vertical gaze. Have the patient fixate on a distant target with the head turned opposite to the direction of interest. For example, to test left-gaze, ask the patient to turn their head to the right while fixating on the target. In incomitant strabismus this will affect the size and / or direction of deviation.
- Choice of fixation target: Use a detailed near target to stimulate accommodation. An insufficiently small target may not reveal the true extent of a strabismus. Use of a light as a target will also not stimulate accommodation. Adapt the target size for eyes with concurrent amblyopia or reduced visual acuity.
- Testing distance: Perform near cover tests at 33cm and distance tests at 6m. Strabismus may vary based on fixation distance. A subtle lateral rectus palsy may present with controlled esophoria at near, but only at distance testing will the presence of esotropia and diplopia be revealed.
Testing ocular motility
- Target choice: Use a penlight for fixation to monitor corneal reflections, avoiding non-illuminated targets like pens or fingertips. Illuminated targets reveal subtle limitations of movement, especially at extreme gazes, by producing asymmetrical corneal reflections.
- Distance: Hold your penlight at a distance of 50–60cm from the patient. This will depend on the arm length of the examiner! A target held too close to the patient may induce convergence which may confound the examination.
- Star shape: Test each position of gaze individually from primary position, observing the movement quality, range and any deviation, before returning to primary position to test the next position. This ‘star’ technique ensures accurate assessment, unlike the limited H-shape method taught in medical school, which misses out direct elevation and depression, thereby missing alphabet patterns, and other disorders of vertical movement.
- Extremes of gaze: Ensure that the target is moved out to the true endpoint of gaze in each direction. A common mistake is to halt the target too early, meaning that subtle muscle limitations or underactions may be missed.
- Noses and eyebrows: Be mindful of facial features obscuring binocular fixation on peripheral gaze, such as deep-set eye sockets, prominent eyebrows or large noses. A penlight is advantageous once again here as the examiner will notice one corneal reflection disappearing with the obscuration.
- Versions and ductions: As mentioned earlier, test the range of movement in each direction with both eyes open, and then again as a uniocular duction movement.
- Alternate cover testing: Perform ACT at the endpoint of each gaze position to detect subtle incomitant horizontal and vertical strabismus, which may not always be visible through corneal reflections alone.
Case example
A 51-year-old female presents to eye clinic with intermittent vertical diplopia for two years. It tends to be present when reading or walking downstairs, and it resolves with an adjustment of head posture. It began after she fell from her bike and sustained a minor concussion, although she didn’t seek medical attention at the time. CT in primary position reveals an intermittent right hypertropia. Squint measurements in different positions confirm incomitant strabismus, with the largest vertical deviation present in laevodepression. Ocular motility testing reveals a 75% limitation of the right superior oblique muscle, with improvement when testing duction, hence confirming a neurogenic fourth nerve palsy. Overaction of the left inferior rectus and right inferior oblique, alongside underaction of the left superior rectus are noted, representing developed muscle sequelae which is consistent with the chronic history following trauma (Figure 4).
Conclusion
In summary, this article offers an introductory guide to the theory of strabismus and ocular motility. While not intended to be comprehensive, it provides a starting point for ophthalmology trainees to gain deeper understanding of this fascinating and important field.
TAKE HOME MESSAGES
-
Head trauma is a common cause of acquired fourth nerve palsy, due to the particularly long course of the cranial nerve.
-
Patients with fourth nerve palsy may complain of diplopia on reading or descending stairs. These activities generally require the eyes to be in a depressed position, in the direction of action of the weakened superior oblique muscle.
-
Compensatory head posture may be adopted in cases of acquired strabismus with diplopia. The patient may turn, raise, lower, or tilt their head in order to move the eyes away from the direction causing diplopia. Strabismus assessment should always be performed with and without compensatory head posture.
References
1. Gantz L, Millodot M, Roth GL. Analysis of Alphabet Patterns of Deviations Found in Patients Without Strabismus in Primary Position. Clin Optom (Auckl) 2022;12:49–56.
2. Ansons AM, Davis H. Alphabet patterns. In: Diagnosis and Management of Ocular Motility Disorders (4th ed). Oxford, UK; Wiley Blackwell; 2014:431–50.
3. Ibid.:121–43.
COMMENTS ARE WELCOME










