Assessment of optic nerve appearance and functions is a daily routine in neuro-ophthalmology. Following a recent high profile court case there has been a significant increase in the amount of referral to ophthalmology departments to assess the optic nerve and its functions and rule out optic nerve swelling. (Part two of this topic available here)
The aim of this review is to provide an overview of optic nerve anatomy and functions, as well as a discussion of optic nerve swelling, its features and its possible causes.
The review will be split over two articles. The first will discuss the basic optic nerve anatomy, functions and various features on optical coherence tomography (OCT) scans and differentiating true from pseudo optic nerve swelling. This article will also discuss unilateral optic neuropathy.
The second article will discuss features of bilateral optic nerve swelling as well as our experience and protocols of management in Manchester Royal Eye Hospital.
Optic nerve anatomy
The optic nerve is the culmination of the axons of the ganglion cells in the neuro sensory retina. These axons form the nerve fibre layer in the retina which then converges to go through the lamina cribrosa and form the optic nerve. The optic nerve is divided into several sections starting with the optic nerve head, which can be seen through funduscopy followed by intraorbital section, intracanalicular section and intracranial section before it joins the contralateral optic nerve to form the optic chiasm.

Upon leaving the globe, the optic nerve is surrounded by the meninges with a small cuff of cerebrospinal fluid (CSF). Although the optic nerve is labelled as the second cranial nerve, in true sense it is an extension to the brain as it is covered with meningeal layers as well.
Optic nerve functions [2]
The optic nerve serves as the connection between the eye and the brain. During assessment of visual functions, there are several areas that need to be tested and each will help differentiate optic nerve from retinal or other ocular pathology.
- Visual acuity is the first of visual functions to be assessed. Various methods are used to assess this function depending on availability as well as patient age and background. The current method used in our unit is LogMAR visual acuity charts.
- Colour vision: There are several ways to assess this function. Ishihara pseudo chromatic plates are most commonly used for this.
- Peripheral vision: This is usually assessed using kinetic perimetry (Goldmann’s) or static perimetry (Humphries) depending on availability and patient cooperation. We tend to use 30-2 Humphries visual fields to assess our patients.
- Pupil reaction (RAPD) [3]: Relative afferent pupillary defect (RAPD) is a clinical sign indicating a difference in function between the right and left optic nerves. It is very helpful to differentiate reduced vision from optic nerve lesions from other possibilities. It is also useful in bilateral versus unilateral optic nerve pathology as well as functional visual loss. The pupillary reaction pathway is as follows: it starts with retinal ganglion cells (RGCs) which axons form the optic nerve. Some of these axons connect to the pretectal nucleus in the upper midbrain; these RGCs contain melanopsin and play a role in the circadian rhythm as well as pupillary reflexes. The pretectal nucleus axons connect with Edinger-Westphal parasympathetic nucleus which is a part of the oculomotor nucleus complex. Axons from this nucleus travel with the III cranial nerve and synapse in the ciliary ganglion, where post ganglionic axons travel in the short ciliary nerves to innervate iris sphincter muscle [4].
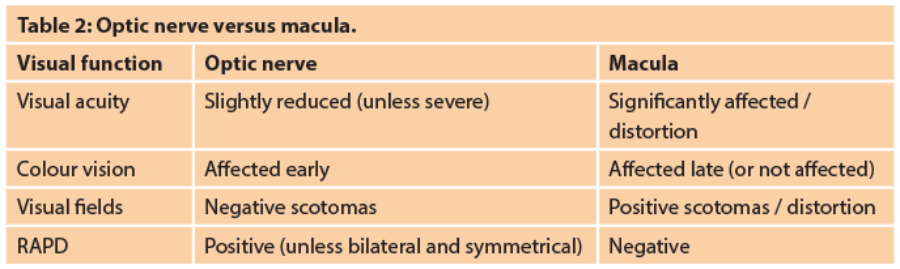
Differentiating optic nerve versus macula pathology:
Table 2 helps differentiate the cause of reduced visual performance.
Optic nerve reaction to injury:
Acutely affected optic nerves tend to swell. The degree and extent of the swelling depend on the type and severity of the insult to the optic nerve. For example, vascular insult to the optic nerve tends to cause ischaemic reaction leading to swelling of the optic nerve head, which can range from mild and sectorial in non arteritic anterior ischaemic optic neuropathy (NAION) to severe and ‘chalky white’ in arteritic anterior ischaemic optic neuropathy (AION). Retrobulbar optic neuritis tend to produce minimal optic nerve swelling compared to other inflammatory optic neuropathies which tend to cause more severe optic nerve swelling. In optic nerve swelling secondary to raised intracranial pressure (papilledema), the swelling is usually bilateral, although might be significantly asymmetric or even unilateral in rare cases [5].
It is usually very important to differentiate unilateral optic nerve swelling from bilateral cases as each will have different possible causes. It is also important to remember that bilateral cases could be unilateral in nature but sequential. Clinical history is crucial in neuro-ophthalmology, it helps understand patient presentation, link symptoms to possible signs, develop an appropriate differential diagnosis and arrange appropriate investigations.
Pseudo optic nerve swelling
Before diagnosing optic nerve swelling, it is very important to rule out causes of pseudo optic nerve swelling; otherwise patients might end up having several unnecessary invasive investigations with financial implications as well as adding to patient anxiety.
- Optic nerve drusen [6]: These are deposits of calcium in the structure of the optic nerve. They are usually present since childhood and asymptomatic. The difficulty in diagnosis lays in identifying buried drusen as they are deep in the structure of the optic nerve (compared to surface drusen which could be readily seen). It is also important to remember that some of these will cause visual fields defects (nerve fibre bundle defects), however, these defects are stationary and do not change with time. Optic nerve ultrasound and auto fluorescence (AF) are usually helpful in diagnosing optic nerve drusen.
- Crowded optic nerves: Small optic nerves tend to be seen in hypermetropic patients, although some high myopes also have them. They usually measure less than 1.75cm of funduscopy and will have a small cup / disc ration (C/D ~ 0.1). Again, optic nerve ultrasound will help in the diagnosis.
- Tilted optic nerves: These tend to feature in high myopic patients and are difficult to assess due to the abnormal anatomy.

OCT features of optic nerve swelling [7,8,9]:
There are several features that can be seen on OCT scans suggesting true optic nerve swelling:
- Increased thickness of the retinal nerve fibre layer. RNFL is measured in the peripapillary region with circular scans of 3.4mm diameter centred on the optic nerve head. The software on the machine compares thickness of RNFL from the patient scanned with an age matched cohort. The normal ‘double hump’ pattern of the patient tests usually falls into the green zone on assessment panel. The green area is the 5-95th percentile by age, yellow area is 1-5th percentile, and red area is below the first percentile. If the nerve fibre layer is swollen, then the patient’s reading will fall into the white zone (above the normal green zone). Attention needs to be paid to the centration of the assessment circle around the optic nerve head.
- Blurring of the optic disc margins. This usually starts with the nasal margin followed by the superior and inferior poles then lastly the temporal margin.
- Assessment of the disc margin / retina angle. In true optic disc swelling usually the angle is wide and the raised optic nerve head slopes into the peripapillary retina, while in pseudo optic nerve swelling that angle is steeper and raised optic nerve falls into a flat peripapillary retina.
- Pockets of fluid at the optic nerve margins.
- Obscuration of blood vessels on and around the optic nerve head, these blood vessels get covered by swollen optic nerve fibres. Frisen classification looks into features of optic nerve swelling such as blurring of the optic disc margin as well as blood vessel obscuration. This can range from small vessels on the optic nerve head in grade III to all large vessels away from the disc in grade V [9].
How to assess the optic nerve head in neuro ophthalmology:
- Assessment of the margin of the optic disc: is it blurred or not?
- How much of the margin is blurred and where?
- Is there any obscuration of the blood vessels?
- Is there any cotton wool spots suggesting ischaemia or any haemorrhages?
- Is there any cup or is it obliterated, compare with the other eye as well?
- Any spontaneous venous pulsation (SVP)? although this sign is very nonspecific as optic nerve swelling is seen in cases with positive SVP and around 20% of normal people will not have SVP.
- What is the patient refractive error?
- What are the patient’s presenting complaint and their visual functions?
- OCT features as discussed before as well as features of pseudo swelling such as disc drusen.
Unilateral optic nerve swelling [2,10]:
- Inflammatory
– optic neuritis
– Demyelination (typical optic neuritis)
– Other inflammatory cause (sarcoid, lupus, etc.)
– atypical optic neuritis - Infectious
– Syphilis
– Spread from sinus or orbital infection - Vascular
– Non arteritic anterior ischaemic optic neuropathy (NAION)
– Arteritic anterior ischaemic optic neuropathy (giant cell arteritis)
– Diabetic papillopathy - Compressive from orbital or cranial lesions
– Aggressive thyroid orbitopathy
– Optic nerve sheath meningioma
– Optic nerve glioma - Infiltrative (lymphoma, etc.)
- Traumatic
1. Inflammatory [11,12]
Features of typical optic neuritis:
- Female gender
- 20-45-years-old
- Mild pain at onset for few days
- Sub-acute reduction of vision (up to hand motion (HM) level)
- Reduced colour vision, various fields defects, RAPD
- Mild or no optic nerve swelling.
Signs and symptoms: Patient usually presents to casualty complaining of dull pain around or behind the eye for a few days with loss of vision over a few hours to two to three days down to CF/HM level. The loss of vision peaks at two weeks after onset then gradual slow improvement of vision to near normal levels in six to eight weeks from onset.
Investigations: Typical optic neuritis does not need investigation as can be diagnosed clinically, although local guidelines may vary and in Manchester Royal Eye Hospital (MREH) we tend to check Aquaporin 4 antibodies levels to rule out Devic disease early on and arrange a head and orbits MRI scan to assess the presence of demyelination. In the presence of features suggestive of atypical nature of the optic neuritis, neuro-imaging becomes essential and various blood tests are requested to look for other causes of unilateral optic nerve dysfunction such as autoimmune antibodies, vasculitis and various infection screening tests.
Treatment options: Most patients with typical optic neuritis recover without any treatment. According to the Optic Neuritis Treatment Trial (ONTT) trial, steroid treatment does not change the outcome with regards to visual function recovery but shortens the time of the episode. In MREH, we tend to treat patients with severe loss of vision (below HM), significant impact on work or life (severe amblyopia in the other eye) or various atypical features. If treated, patients can be given either three doses of 1g of IV methyl prednisolone followed by 10 days of 1mg/Kg of oral prednisolone, or a five day course of 500mg oral methyl prednisolone.
Case example
-
Female 35-year-old
-
Sudden onset blurred vision, developed over a course of two to three days
-
Mild pain behind the eye
-
Seen in Emergency Eye Department (EED)
-
Visual acuity: HM
-
Colour vision: 9/17 on Ishihara plates
-
Reduced central sensitivity on Humphrey visual test
-
RAPD present
-
Diagnosis: Typical optic neuritis
-
No treatment was given as per ONTT
-
Investigations: AQP4 & MRI
-
Prognosis: dependent on presence of demyelination features on the brain MRI
2. Infectious optic neuropathy
This type of optic neuropathy is much rarer. It usually follows from nearby infections in the orbit or paranasal sinuses. Para-infectious optic neuropathy can sometimes affect optic nerve functions following severe infections such as meningitis as well as pneumonia.
Investigations: These include screening for various possible infections with blood tests, neuro imaging, lumbar puncture and chest X-ray.
Treatment options: Depends on the type of infection found and possible need to give steroids as an adjunct treatment.
Case example
-
38-year-old male
-
Seen in EED for reduced vision in right eye
-
Noted to have optic nerve swelling
-
Reduced VA, CV, and RAPD
-
Enlarged blind spot on field testing
-
Diagnosed with atypical optic neuritis
-
Blood tests showed positive syphilis titres
-
Referred to GUM clinic for treatment
3. Vascular optic neuropathy
• Non arteritic anterior ischaemic optic neuropathy (NAION):
Features: This is the most common type of optic neuropathy. It affects patients over 40-years-old, usually with microvascular risk factors such as hypertension and diabetes. These patients can also have other systemic risk factors such as sleep apnoea and usually have local risk factors (crowded optic disc, known as ‘disc at risk’, so there is a need to assess the other eye).
Signs and symptoms: Patients usually are aware of acute sudden painless loss of vision with varying level of reduced vision. The typical associated field defect is inferior altitudinal field defect. The level of vision is usually stable following onset although some patients show signs of further deterioration in the first few days following onset and some patients show some slow improvement at later stages. Patients will have concomitant loss of colour vision (although difficult to assess on Ishihara if visual acuity is significantly reduced) as well as RAPD, unless have bilateral symmetrical optic neuropathy. Fundus examination shows swollen optic nerve, which typically affects a segment of the optic nerve head only.
Investigations: NAION can be diagnosed clinically although most patients will need blood tests to assess vascular risk factors and rule out AAION due to giant cell arteritis (GCA). Neuro-imaging could be done to rule out compressive lesions depending on local guidelines.
Treatment: There is no evidence based treatment for NAION. Patients are referred to their general practitioner to assess their vascular risk factors and optimise them. If other risk factors are present (such as sleep apnoea and use of sildenafil then these need to be addressed as well).
4. Arteritic anterior ischaemic optic neuropathy (AAION) due to GCA:
Features: Sudden, profound loss of vision in an elderly patient due to anterior ischaemic optic neuropathy. This will cause diffuse ‘chalky white’ optic nerve swelling. Other common symptoms include recent onset headaches, temporal pain, jaw claudication. Other general symptoms include weight loss, malaise and night sweats. Giant cell arteritis is an emergency that needs to be investigated and treated urgently. Risk factors for this condition include age, female gender, Caucasian race and history of polymyalgia rheumatica (PMR).
Investigations: These include urgent blood tests looking for raised inflammatory markers such as ESR, CRP, as well as an increased platelet count and possible normocytic anaemia. Other tests include temporal artery ultrasound and biopsy (TAB).
Treatment: GCA should be suspected clinically and treated urgently with high dose of oral or IV steroids depending on the local guidelines without the wait for the TAB results. Further assessment by rheumatology teams is usually recommended in order to assess the patient generally and manage immunosuppression.
Case example
-
78-year-old male
-
Episodic loss of vision in right eye then vision loss to HM
-
Mild pain around right eye / slightly tender
-
Swollen right optic nerve
-
Diagnosis AION due to GCA
– Bloods: raised ESR, CRP, platelets
– IVMP then oral steroids
– TAB
– Referral to rheumatology
References:
1. Hayreh SS: Ischemic Optic Neuropathies. Springer-Verlag: Berlin Heidelberg; 2011:7-34.
2. Miller N, Newman N. Walsh and Hoyt Clinical Neuro Ophthalmology. 6th edition. Lippincott Williams & Wilkins: Philadelphia, USA; 2005.
3. Bremner FD. Pupil assessment in optic nerve disorders. Eye 2004;18:1175-81.
4. Kaufman PL, Levin LA, Alm A, et al. Adler's Physiology of the Eye. 11th edition. Elsevier Health Sciences: Amsterdam, Netherlands; 2011.
5. Lepore FE. Unilateral and highly asymmetric papilledema in pseudotumor cerebri. Neurology 1992;42(3 Pt1):676-8.
6. Lam BL, Morais CG Jr, Pasol J. Drusen of the optic disc. Curr Neurol Neurosci Rep 2008;8(5):404-8.
7. Johnson LN, Diehl ML, Hamm CW, et al. Differentiating optic disc edema from optic nerve head drusen on optical coherence tomography. Arch Ophthalmol 2009;127(1):45-9.
8. Rebolleda G, Diez-Alvarez L, Casado A, et al. OCT: New perspectives in neuro-ophthalmology. Saudi Journal of Ophthalmology 2015;29(1):9-25.
9. Scott CJ, Kardon RH, Lee AG, et al. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Arch Ophthalmol 2010;128(6):705-11.
10. Chan J. Optic Nerve Disorders, Diagnosis and Management. 2nd edition. Springer-Verlag: Berlin Heidelberg; 2014.
11. Beck RW, Cleary PA, Anderson MM Jr, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis: The Optic Neuritis Study Group. N Engl J Med 1992;326(9):581-8.
12. Beck RW, Cleary PA. Optic neuritis treatment trial: one-year follow-up results. Arch Ophthalmol 1993;111(6):773-5.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME