Cataract surgery is the most frequently performed surgical procedure in the UK [1]. The demand for cataract surgery is projected to increase with ageing population, and the recent pandemic has further contributed to the extended waiting times in the UK. Therefore, all stakeholders have focussed their efforts to increase the efficiency of the cataract care pathways [2].
Introduction
At Addenbrooke’s Hospital, Cambridge, the cataract care pathway was redesigned during the pandemic to incorporate telephone preassessments led by specialist nurses. This replaced the traditional pathway which involved a face-to-face (F2F) preassessment, which had its limitations during the pandemic due to social distancing rules. It also created difficulties for elderly patients who often required transportation but found this challenging in the pandemic climate.

The newly designed telephone preassessment formed part of the Cambridgeshire cataract shared care model in which cataract referrals and postoperative follow-up were undertaken by community optometrists [3,4]. This shared care model with community optometrists has already aided in a noticeable reduction in hospital visits and reduced doctor led clinics since its implementation [3] leaving room for surgeons to focus on surgical aspects of the cataract pathway.
Telephone preassessment was intended to benefit the cataract pathway and aid in the implementation of high-flow cataract surgery; however, no formal assessment of its impact has been made to date. We therefore designed a retrospective study to assess the effectiveness of telephone preassessment to replace F2F assessments in the cataract pathway.
Methods
Objectives
The purpose of the study was to evaluate the outcome of the nurse-led telephone preassessment pathway for cataract surgery in relation to its role, benefits and limitations.
Study Design
We retrospectively analysed 302 (of which 301 were successfully contacted) consecutive patients referred to the telephone preassessment service at Addenbrooke’s hospital for cataract surgery. This spanned from April-June 2021.
The telephone preassessment service was introduced in March 2021. A one-month period between introduction of the service and data collection (April 2021) was given to account for any initial teething issues.
Data from these patients were extracted from the hospital patient records (EPIC Hyperspace database) and imported into Excel for further analysis.
Inclusion and exclusion criteria
Simple non-complex cataract patients assigned to the nurse-led telephone preassessment route were included in the analysis. Patients triaged to doctor-led F2F clinics were excluded from the study.
Telephone preassessment pathway
The telephone preassessment pathway was conducted for both internal and external cataract referrals.
Patients were first triaged into two groups: those eligible for the nurse-led telephone preassessment pathway and those requiring a doctor-led F2F consultation based on referral details in the cataract referral form (completed by community optometrists). Patients then underwent the nurse-led telephone assessment which has a pre-determined format to assess the patient’s medical history, social history and the ocular history, including their willingness to undergo cataract surgery.
Results of this consultation lead either to a successful listing of the patient for cataract surgery or referral for further doctor-led F2F consultation. Reasons for referral for further assessment in a doctor led clinic included issues such as complex cataract or patients with significant comorbidities requiring further workup.
Once added to the cataract surgery list, patients had their biometry session with a nurse or biometry technician scheduled. Once this has been completed, patients were then ready to undergo cataract surgery. Figure 1 below shows a diagram of the overall workflow of this preassessment pathway.
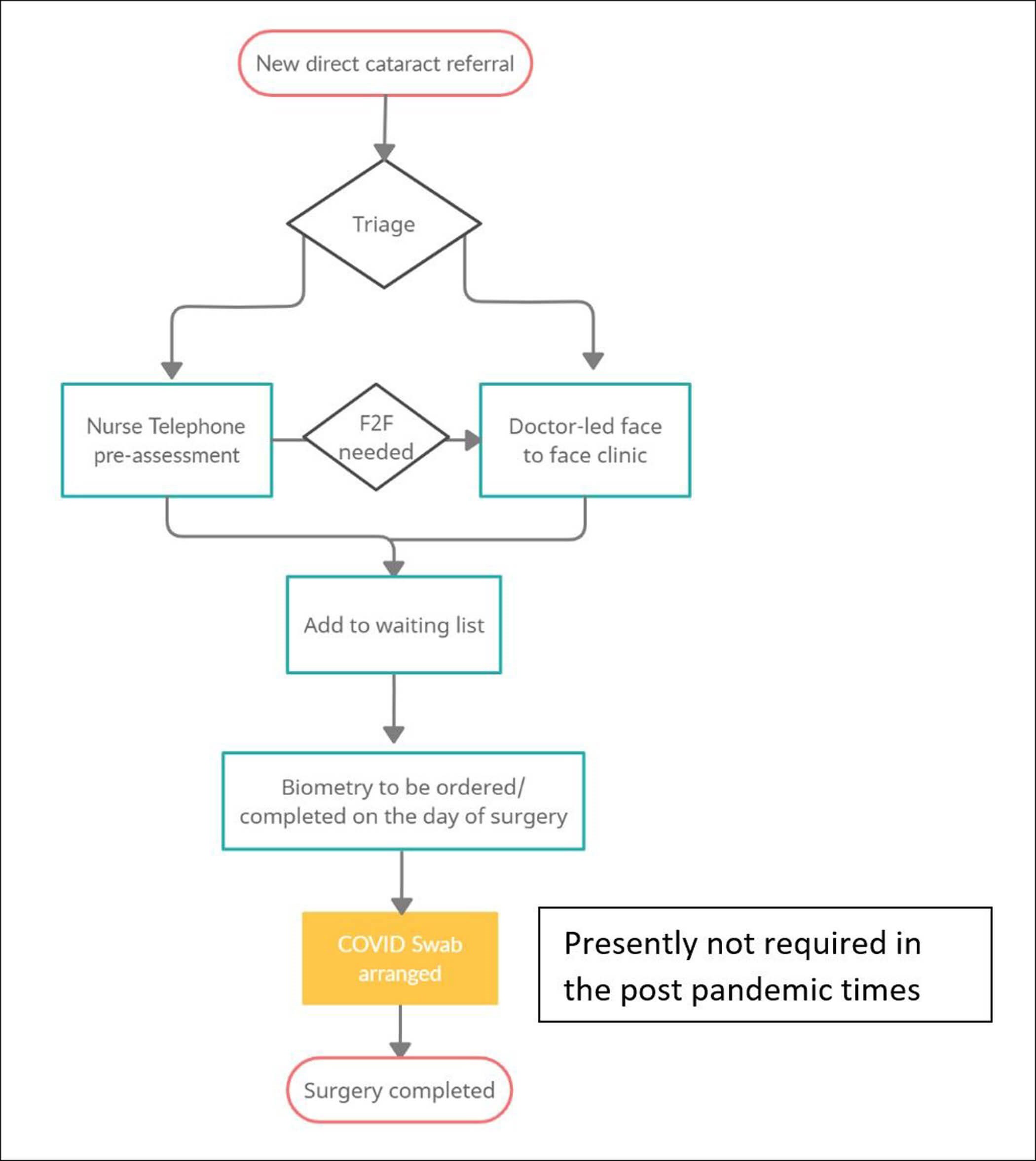
Figure 1: Telephone preassessment pathway.
Data extraction
Several variables were extracted from patient data via the EPIC database. This included patient characteristics (age and gender), cataract severity (listing visual acuity, cataract grade, cataract laterality) and ocular co-morbidities. Additionally, data on referral route and type, dates of referral and telephone preassessment, date of cataract surgery, listing outcomes as well as follow-up route.
Data analysis
The main outcomes used to assess the efficacy of the telephone preassessment pathway are:
- Listing rates / outcomes
- Qualitative data for patients that required further F2F appointments
- Completion of surgery
- Route of postoperative discharge and follow-up
Results
From April-June 2021, a total of 302 consecutive patients were retrospectively analysed. One patient did not attend the telephone preassessment and the remaining 301 were successfully contacted (99.7% compliance rate). The mean age was 76.4 years (SD, 9.4; range 39-95). One-hundred and seventy-eight (59.1%) of patients were female and 123 (40.9%) were male.
Almost all referred patients (289 of 301, 96.0%) had a listing visual acuity equal or worse than 6/12 Snellen’s acuity, which is used as the general threshold for cataract surgery. The remaining referred patients with a listing acuity better than 6/12 had either narrow angle glaucoma or significant anisometropia.
Referral routes
A large proportion of the referrals were from the community optometrists (176; 58.5%), while GP-led referrals only constituted a small percentage of referrals (2; 0.7%).
The remaining patients (123; 40.9%) were referred for telephone preassessment via internal hospital eye clinics. Most of the internal clinic referrals were from glaucoma (38; 30.9%), medical retina (40; 32.5%) and vitreoretinal (27; 22.0%).
Listing rates / outcomes
Of 301 patients, telephone preassessment resulted in a successful listing for cataract surgery in 264 patients, giving an overall listing rate of 87.7%. 20 patients (6.6%) required further F2F referral as determined by the nurse at telephone preassessment. 17 patients (5.6%) were not listed for surgery / deemed unsuitable for surgery at preassessment. This means that 93.4% of patients received a definitive listing outcome (for surgery / no surgery) following telephone preassessment.
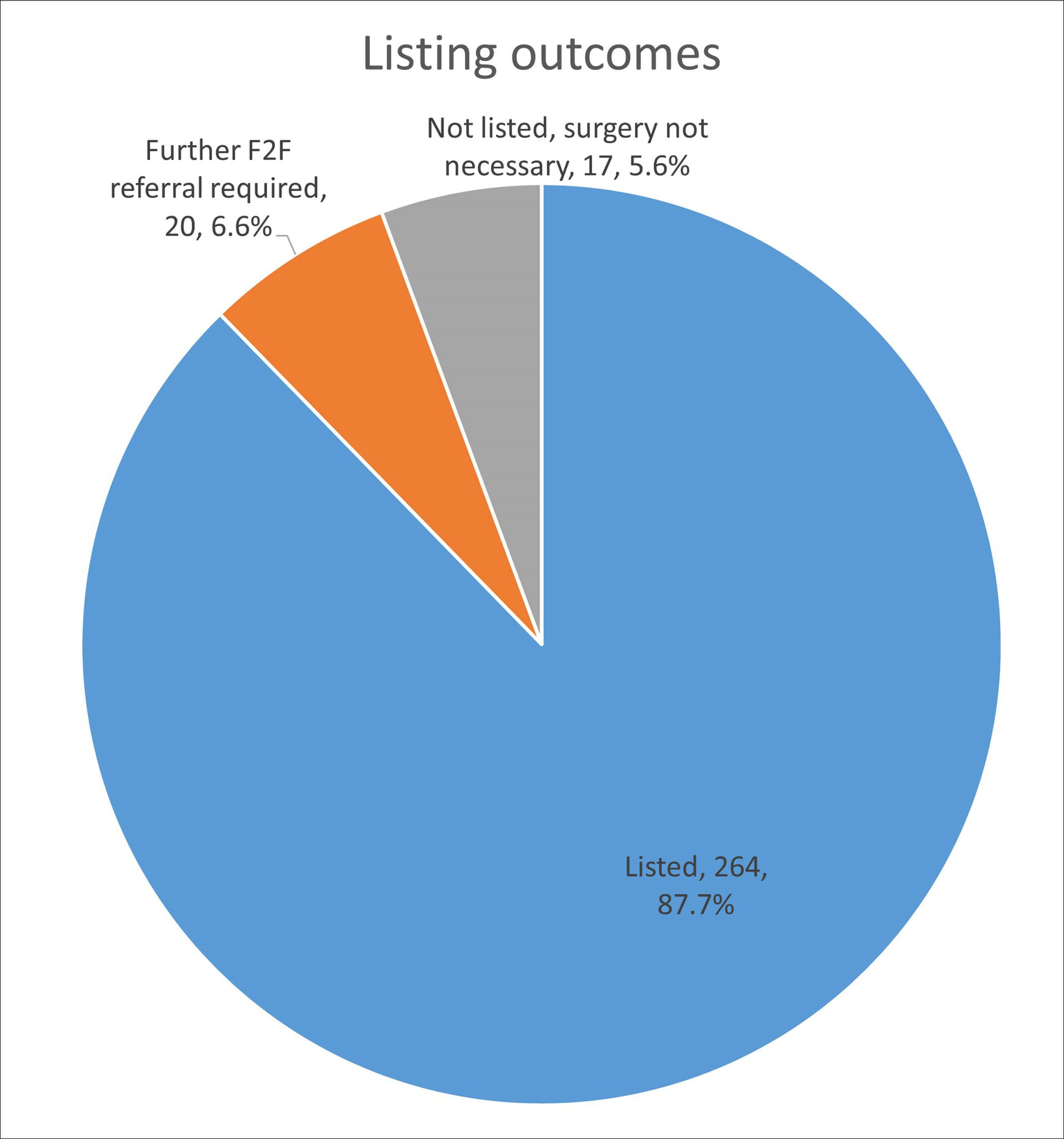
Figure 2: Listing outcomes for patients evaluated by telephone preassessment.
Of the 20 patients who required further F2F referral, 15 of them were referred from community optometrists and five of them were referred internally for cataract surgery. These patients largely had complex ocular co-morbidities requiring follow-up with a consultant for surgical planning. Nineteen out of 20 were listed for cataract surgery and underwent a successful cataract surgery. The one patient who did not undergo surgery had general comorbidities and passed away from systemic illness a few months later.
No patients experienced cancellations of surgery on the day of operation due to concerns from the surgical team / surgeon. A total of 93% (n = 246) patients listed via nurse led telephone preassessment had a successful cataract surgery. This demonstrated that the telephone preassessment was generally an effective means to list patients for cataract surgery, with no incorrect listings in our findings.
Eighteen of the 264 patients listed for surgery could not attend their cataract surgery appointment. This was due to numerous reasons not related to the quality of the telephone preassessment. This included patient choice to see private providers (3), patient death (4), current systemic illness (4), patient declining /deciding not to go ahead with surgery (6) and complex transport requirements (1).
The approximate time spent per patient in telephone preassessment was 30 minutes.
Route of discharge
Of the 246 patients who underwent cataract surgery after being listed via telephone preassessment, a total of 157 (63.8%) patients were discharged to a community optometrist-delivered postoperative discharge scheme and 89 (36.2%) patients were followed-up in the hospital.
Discussion
Our study provides evidence that a nurse-led telephone preassessment was largely safe and effective for patients referred for cataract surgery. This was demonstrated in our results which highlight that none of the patients were inappropriately referred for surgery, with a false positive rate for referral to nurse telephone pre-assessment of only 5.6% in our cohort.. The nurses were able to correctly identify the patients who required F2F assessments and there were no surgery cancellations on the day of intended surgery due to concerns related to the quality of preassessment.
The telephone assessment is useful to identify patients requiring doctor / consultant decisions regarding the course of care, which in our study was 6.6%. Thus, a majority of cases (93.4%) could be safely assessed by allied health professionals such as specialist nurses where we have the essential clinical details related to vision, refraction and ocular comorbidities listed in the referral form. Such a designated cataract referral form was used in our cataract pathway that incorporated community optometrists and enabled direct referrals to be sent to the hospital-based cataract service. The nurse-led telephone preassessment was made possible with such a designated referral form used in the Cambridgeshire cataract shared care scheme (Figure 3). The clinical details in the form enhances the quality of cataract referral, which in turn facilitates an effective triage and a telephone based preassessment.
A case series of 4966 patients by Subramanian ML, et al. shows that phone interviews (for preoperative cataract surgery assessment) were not associated with a higher number of unplanned admissions, mortality or surgery cancellations [5]. Telephone interviews in that study were also associated with a lower non-compliance rate. This is a positive outcome which we are able to show in our results as well, with no same day surgery cancellations and a high compliance rate in our sample. However, the abovementioned case series does not include assessment of the patient’s preoperative vision, refraction and ocular co-morbidities. The knowledge of these aspects in a designated cataract referral form would allow even more meaningful discussion on postoperative refractive targeting, offering realistic patient expectations and counselling for patients expecting cataract surgery. Furthermore, it saves on time required for such discussion on the day of surgery allowing for smooth workflow in high-volume cataract lists. In our study, we have incorporated such a referral form and all our nurses had details of the patient’s preoperative refraction, vision and comorbidities prior to undertaking the telephone preassessment.
Our study also highlights the numerous benefits of a telephone-based preassessment model. The scheme allows care to be conducted closer to home, it avoids unnecessary patient footfall to busy hospital eye clinics and allows nurses to work from home when conducting the telephone assessments. The biometry visit to the hospital was quick and easy that also allowed for technician-run biometry sessions to be incorporated into the cataract pathway, again reducing the demands on nurses or doctors having to undertake this test.
Thus, our study provides a framework of telephone preassessment which can be applied to other NHS trusts undergoing service improvement. Our results indicate that suitably trained nurses can manage preassessment for cataract surgery in place of a doctor-led F2F assessment. This improves the value of allied health professionals in the hospital while also allowing surgeons to focus on more complex patients. The GIRFT (Getting It Right First Time) cataract initiative is constantly thriving to standardise the NHS cataract pathway and our results could assist in supporting this change to provide cost savings for hospital eye services and safe care closer to home. This would be of clear benefit to a service such as cataract surgery, which has experienced increasing strain over the years as we experience the effects of an aging population [2].
Telephone assessment only works if there is qualifying data on patients at the time of referral. This enables effective triage of patients into the nurse-led telephone preassessment pathway or to F2F doctor appointments. In the Cambridge cataract shared care model, this data is recorded in the referral form, which is typically completed by community optometrists who have gained accreditation with the hospital eye service. A service level agreement between health commissioners, hospital eye services and community optometrists with key performance indicators is vital to achieve success, governance and cost savings in the cataract shared care scheme.
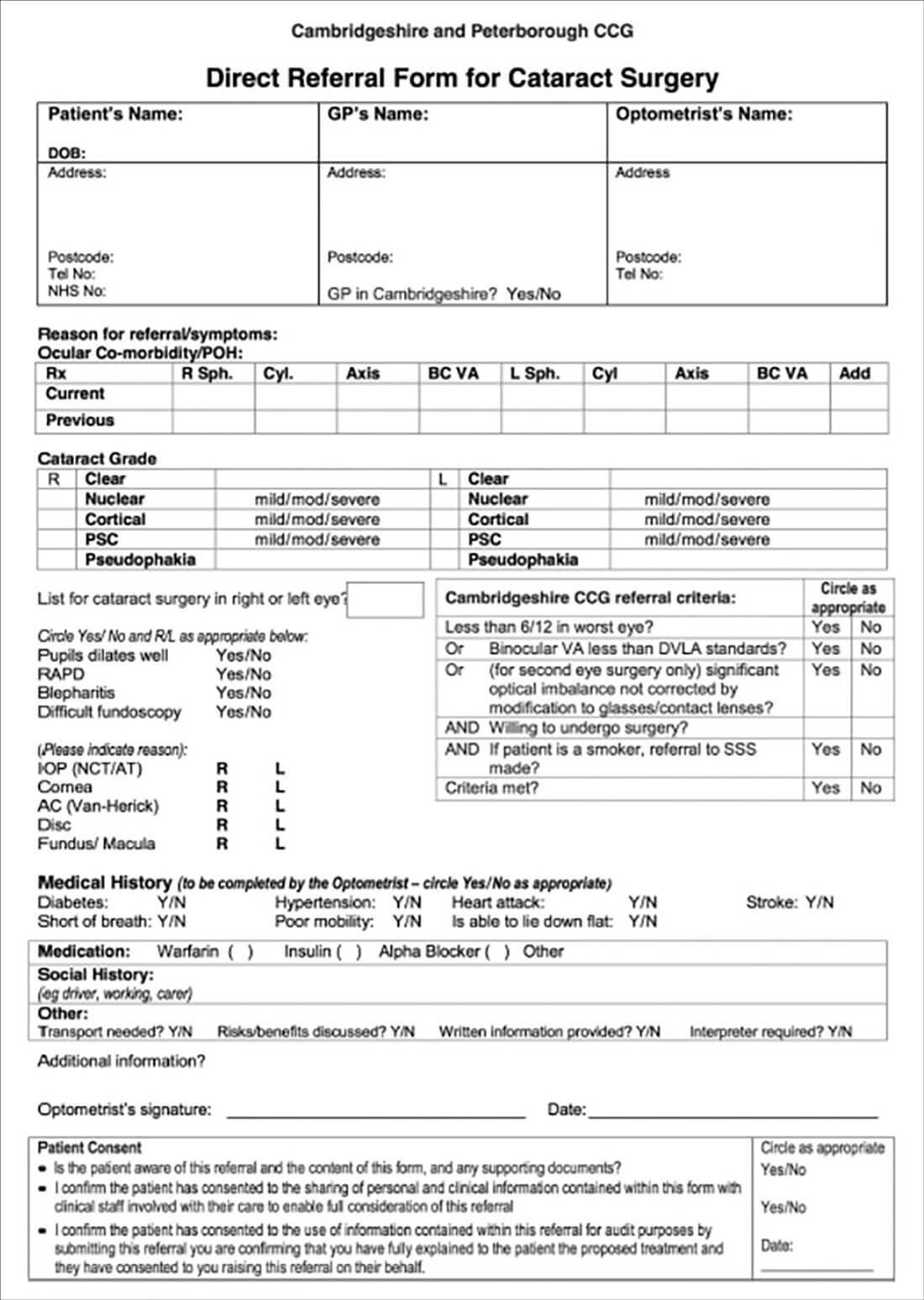
Figure 3: Cataract surgery referral form.
TAKE HOME MESSAGES
-
Nurse-led telephone preassessment is safe and effective in patient counselling and listing for cataract surgery when assisted by a designated cataract referral form by community-based optometrists. Patient attendance to the tele consultation was 99%, with 93% getting a definitive listing decision at the end of consultation.
-
There were no ‘on the day cancellations’ of surgery and 64% were discharged from the hospital eye service for community follow-up.
-
Cataract shared care model enables allied health professionals such as community optometrists and specialist nurses to participate in the cataract pathway.
-
Our results support a service level agreement between all stakeholders that provided cost savings for hospital eye services and safe care closer to home, in line with the GIRFT cataract initiative.
References
1. The Royal College of Ophthalmologists. National Ophthalmology Database Audit, Key Findings Summary 2017-2018 (2018).
https://www.nodaudit.org.uk/u/
docs/20/hfsjzvezyj/Key%20Findings
%20Summary%202019.pdf
[last accessed: April 2022]
2. Maubon L, Nderitu P, O’Brart D. Returning to cataract surgery after a hiatus: a UK survey report. Eye 2022;36,1761-6.
3. Voyatzis G, Roberts HW, Keenan J, et al. Cambridgeshire cataract shared care model: community optometrist-delivered postoperative discharge scheme. Br J Ophthalmol 2014;98(6):760-4.
4. Bowes OMB, Shah P, Rana M, et al. Quality indicators in a community optometrist led cataract shared care scheme. Ophthalmic Physiol Opt. 2018; 38(2):183-92.
5. Subramanian ML, Badami A, Vavrek F et al. Phone Interviews for Preoperative Medical Evaluation for Cataract Surgery. J Gen Intern Med 2019;34:1121-2.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME