Confounding and reverse causation in observational ophthalmic epidemiology
Traditional observational studies are inherently limited in establishing a causal effect of an exposure on an outcome of interest. One fundamental limitation is confounding, whereby causation is incorrectly attributed to a third variable that is independently related to both the exposure and outcome but does lie on the causal pathway between the two.
For example, numerous observational studies have reported an association between alcohol consumption and the risk of glaucoma [1-3]. However, people that drink significant amounts of alcohol are also more likely to smoke, and so estimates of the effect of alcohol consumption on glaucoma risk may be confounded by smoking. Randomisation minimises the influence of both measured and unmeasured confounding.
Reverse causation is another important limitation in traditional observational studies. This is where the association between an exposure and an outcome may arise (at least in part) from the effect of the outcome on the exposure, i.e., the opposite of the presumed direction of causality. For example, increased pro-inflammatory cytokine levels may be either a cause or consequence, or both a cause and consequence, of anterior uveitis. Inferences from conventional observational data will be limited in their ability to separate the causal effect of pro-inflammatory cytokines on uveitis from the converse effect of uveitis on pro-inflammatory cytokine levels. But what if there was a way to investigate the effect of an exposure on an outcome that is robust to the influence of confounding and reverse causality?
Mendelian randomisation: ‘nature’s randomised trials’
In a seminal paper in 2003, Smith and Shah, inspired by allogenic sibling bone marrow transplantation studies, proposed a novel epidemiological approach that came to be known as ‘Mendelian randomisation’ (MR) [4]. MR uses genetic variants identified from large-scale genome-wide association studies (GWAS) within an instrumental variable (IV) framework to make inferences about the causal effect of an exposure on an outcome (Figure 1).
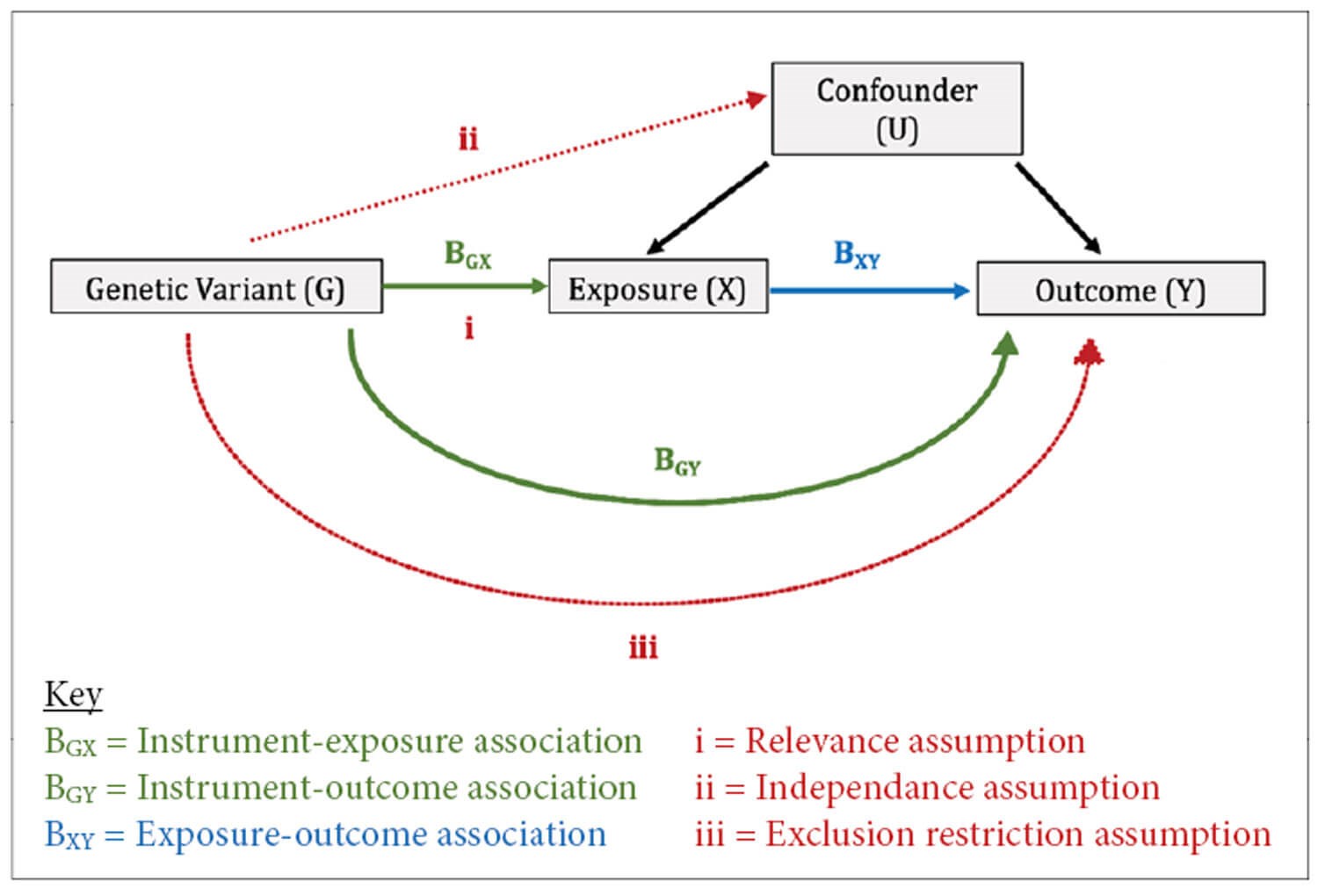
Figure 1: shows a direct acyclic graph for Mendelian randomisation (MR) that depicts the three instrumental variable (IV) assumptions, upon which the validity of the genetic variants as instruments rests: (1) Relevance: the genetic variants are associated with the exposure, (2) Independence: the genetic variants are independent of confounders, (3) Exclusion-restriction: the genetic variants influence the outcome only via the exposure (or factors downstream of the exposure). In the Wald ratio method, the instrument-outcome association (BGY) is divided by the instrument-exposure association (BGX) to produce a ratio estimate for each genetic variant. These ratio estimates are then combined in an inverse-variance weighted meta-analysis to produce a causal MR estimate of the effect of X on Y. Taken from Rajasundaram et al. 2022 [6].
By virtue of Mendel’s Law of Segregation and Law of Independent Assortment, the inheritance of genetic variants is random. This reduces the likelihood that the phenotypic effect of a particular genetic variant is related to, and thus confounded by, environmental factors. Accordingly, MR has been called ‘nature’s randomised trials’ [5]. Furthermore, germline genetic variation is non-modifiable by the environment and temporally precedes the onset of clinical outcomes, which in turn reduces the risk of reverse causation. Thus, under the classical assumptions of any IV analysis, MR offers an elegant method for investigating the effect of putative causal risk factors on common ophthalmological diseases that is less vulnerable to some of the fundamental weaknesses of conventional observational studies.
Myopia, intraocular pressure, and rhegmatogenous retinal detachment
With the increasing availability of summary-level genetic data pertaining to ocular phenotypes and ophthalmological disease, Mendelian randomisation is quickly becoming an invaluable tool in understanding the aetiology of common eye diseases. Han et al. leveraged UK Biobank genetic data involving over 240,000 people within an MR framework to investigate the causal effect of myopia and intraocular pressure (IOP) on the risk of rhegmatogenous retinal detachment (RRD) [7]. RRD is a potentially sight-threatening condition for which intervention is time-critical and so identifying causal risk factors may help us to predict and prevent the onset of RRD, as well as guiding potential therapeutic targets. They found that for each unit (diopter (D)) increase in genetically proxied mean spherical equivalent (MSE), the odds of retinal detachment decreased by 28% (95% CI = 26% to 31%) and for each unit (mmHg) increase in genetically proxied IOP, the risk of retinal detachment increased by eight percent (95% CI = 1.03 to 1.14). Thus, they provide genetic support for a causal effect of myopia and IOP on the risk of RRD.
The methodological value of MR here is that the relationship between myopia and RRD is likely to be confounded by cataract surgery in conventional observational studies because myopia increases the risk of cataract and cataract surgery is a risk factor for RRD. The random inheritance of the genetic variants used to proxy myopia, IOP and RRD in this study, as governed by Mendel’s First and Second Laws of Inheritance, makes these results robust to the impact of confounding by cataract surgery. Of course, like all empirical research methodology, MR has limitations, and these have historically centred around the three core IV assumptions of 1) relevance, 2) independence and 3) exclusion restriction (Figure 1).
The first assumption is testable, and several robust sensitivity analyses have been developed to interrogate the third assumption [5]. However, with respect to the second assumption, most MR studies involve unrelated individuals and are therefore semi-randomised. Future MR studies will require greater twin data and with-family study designs to minimise the influence of biases of population structure, thus making these studies truly randomised [8].
Concluding remarks
Mendelian randomisation is a powerful tool that offers great potential in disentangling association from causation when probing the aetiology of common eye diseases. As its implementation becomes increasingly popular, ophthalmologists would do well to gain a basic understanding of it.
References
1. Kahn HA, Milton RC. Alternative definitions of open-angle glaucoma. Effect on prevalence and associations in the Framingham eye study. Arch Ophthalmol 1980;98(12):2172-7.
2. Wise LA, Rosenberg L, Radin RG, et al. A prospective study of diabetes, lifestyle factors, and glaucoma among African-American women. Ann Epidemiol 2011;21(6):430-9.
3. Lamparter J, Schmidtmann I, Schuster AK, et al. Association of ocular, cardiovascular, morphometric and lifestyle parameters with retinal nerve fibre layer thickness. PLoS One 2018;13(5):e0197682.
4. Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 2003;32(1):1-22.
5. Thanassoulis G, O’Donnell CJ. Mendelian randomization: nature’s randomized trial in the post-genome era. JAMA 2009;301(22):2386-8.
6. Rajasundaram S, Rahman RP, Woolf B, et al. Morning cortisol and circulating inflammatory cytokine levels: a mendelian randomisation study. Genes (Basel) 2022;13(1):116.
7. Han X, Ong JS, An J, et al. Association of myopia and intraocular pressure with retinal detachment in European descent participants of the UK biobank cohort: a Mendelian randomization study. JAMA Ophthalmol 2020;138(6):671-8.
8. Davies NM, Howe LJ, Brumpton B, et al. Within family Mendelian randomization studies. Hum Mol Genet 2019;28(R2):R170-9.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME