The authors investigate what proportion of patients undergoing pars plana vitrectomy subsequently developed ocular hypertension or a diagnosis of glaucoma.
A systematic review carried out in 2017 including seven studies found that there is evidence that pars plana vitrectomy (PPV) is a risk factor for developing open angle glaucoma (OAG) and ocular hypertension [1]. However, the great heterogeneity of the studies included made interpretation of the results difficult.
Ocular hypertension following PPV is common, and some cases go on to develop glaucoma. Studies have shown that between 19-28% of cases go on to develop ocular hypertension following vitreoretinal surgery [2]. Chang has estimated that the risk of glaucoma following vitreoretinal surgery may be as high as 20% [3]. He postulates that the mechanism for vitreoretinal surgery leading to glaucomatous optic nerve damage may be due to increased oxygen levels in the vitreous leading to oxidative damage in the trabecular meshwork, with pseudophakic patients particularly at risk.
This study aimed to investigate what proportion of patients undergoing PPV subsequently developed ocular hypertension or a diagnosis of glaucoma within a UK Ophthalmology Department over a five-year period.
Methods
Study setting and design
A retrospective case notes analysis was carried out between October and December 2021 at Stoke Mandeville Hospital (SMH) Ophthalmology Department, UK. The case notes for all patients who underwent PPV between 2015 and 2020 were collected. These patients were identified by the diagnostic code provided by the doctor in clinic when completing an electronic outcome form on the electronic patient record. Those that were subsequently seen in the hospital’s glaucoma department were selected for review. Each case note was reviewed to collect patient demographic details, vitreoretinal intraoperative details and postoperative details, postoperative intraocular pressures (IOP), glaucoma diagnoses and other ocular pathologies.
Inclusion criteria
All patients undergoing a PPV between 2015-2020 who were subsequently reviewed in the glaucoma service.
Exclusion criteria
- Preoperative diagnosis of glaucoma
- Preoperative ocular anti-hypertensive medication
- Review in glaucoma service prior to PPV.
Results
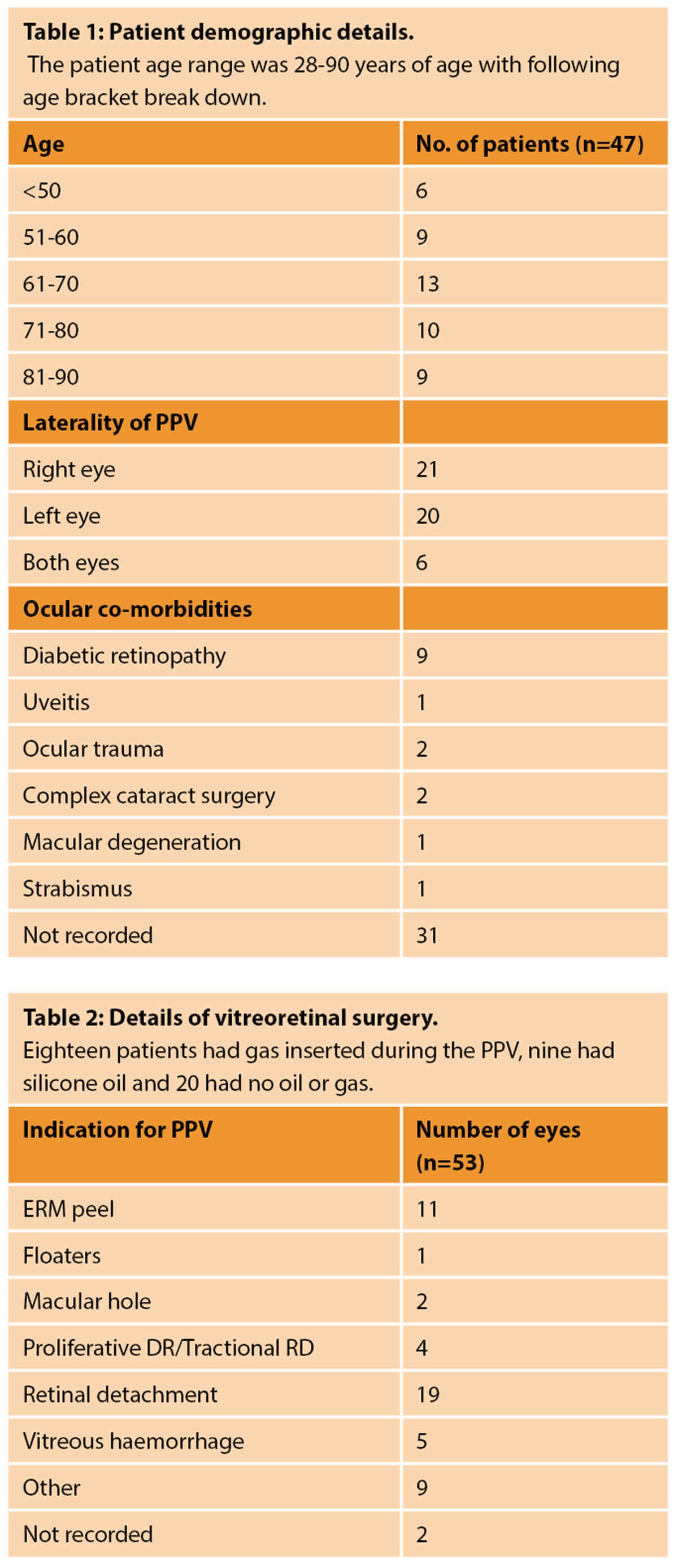
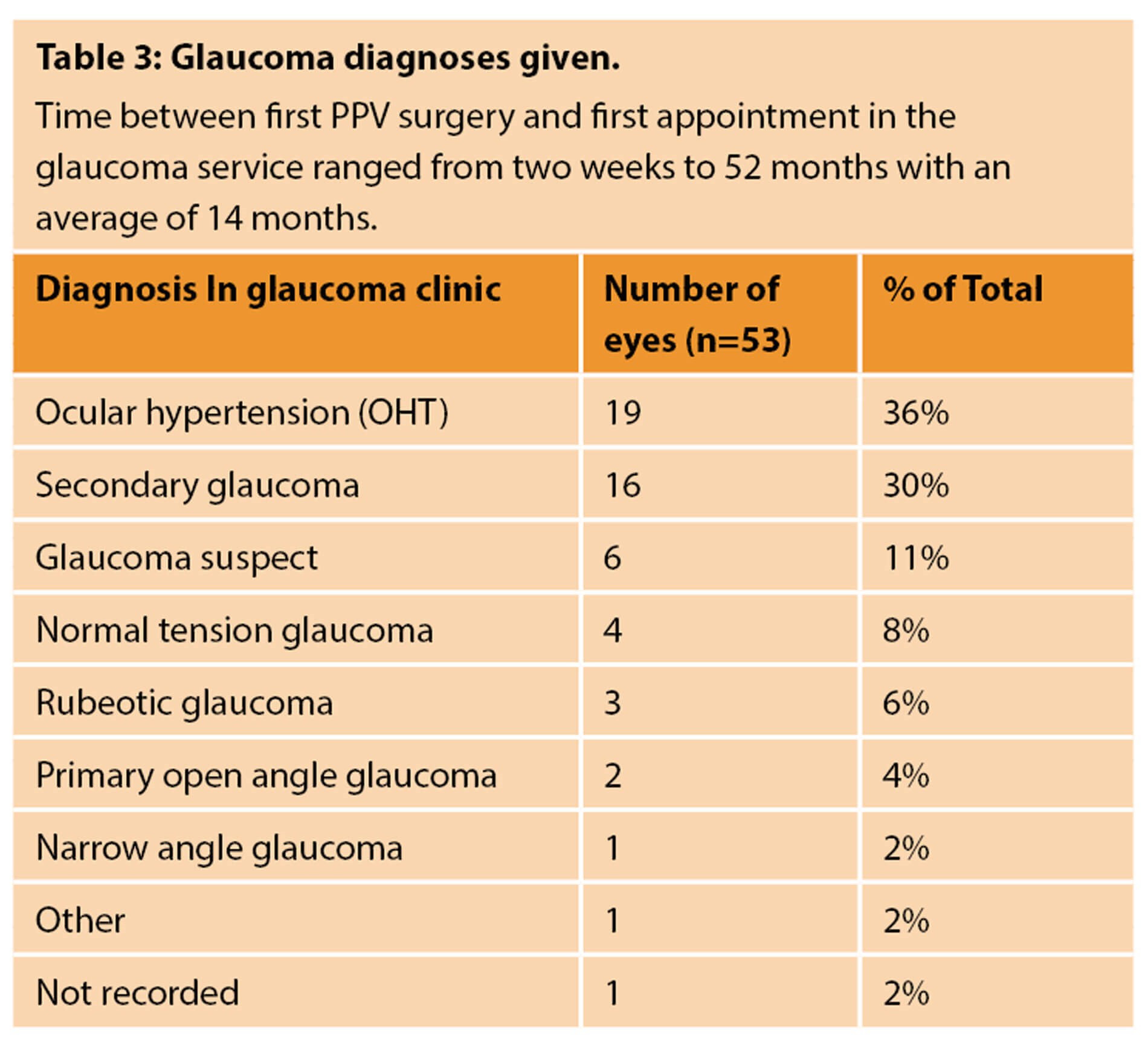
Seventy patients between 2015-2020 were recorded as being seen in the SMH glaucoma service following a PPV. This data set includes 80 eyes. However, of these, only 47 patients and 53 eyes were included in the analysis, as all others had a diagnosis of glaucoma or raised IOP prior to the PPV.
Glaucoma
Secondary glaucoma: Of the 16 patients diagnosed with secondary glaucoma, only six were diagnosed in the notes specifically as ‘secondary glaucoma due to ocular surgery’ following a PPV. However, in all 16 eyes, secondary glaucoma only existed in the eye that had undergone a PPV. Three eyes were diagnosed as secondary IOP rise due to postoperative steroids, one due to silicone oil, two due to uveitis-glaucoma-hyphema (UGH) syndrome, two with secondary glaucoma due to trauma from penetrating eye injury, and two eyes with secondary glaucoma following multiple complex retinal and corneal surgeries.
OHT: Of the 19 eyes diagnosed with OHT, all cases appear to be new cases of OHT diagnosed following a PPV. In 15 out of these 19 eyes there was no ocular hypertension diagnosed in the contralateral eye that did not undergo a PPV.
Glaucoma suspect: normal tension glaucoma (NTG) and primary open angle glaucoma (POAG): of the six eyes diagnosed as glaucoma suspects, four with NTG and two with POAG, again all diagnoses occurred following a PPV in the same eye.
Rubeotic glaucoma: All three eyes diagnosed with rubeotic glaucoma also had proliferative diabetic retinopathy (PDR). Existing proliferative diabetic retinopathy is known to increase the risk of neovascular glaucoma following a vitrectomy. Several recent observational studies have shown between 18-23% of eyes with PDR go on to develop neovascular glaucoma following PPV. Risk factors include preoperative high IOP, use of insulin and low HbA1c [4-6].
Postoperative IOP
Twenty-nine eyes (55%) were recorded as having a postoperative IOP spike, defined as an IOP of >20mmHg within first four weeks postoperatively. Twenty eyes did not have a postoperative IOP rise, and seven eyes did not have a postoperative IOP recorded.
Of the 29 eyes that did have a postoperative increase in IOP, 13 eyes were recorded as still having raised IOP at one month (IOP <20mmHg), and 13 continued to have raised IOP after three months. Three eyes had a normal IOP after one month.
Of the 29 eyes with postoperative raised IOP, 48% (n=14) went on to be diagnosed as OHT, 38% (n=11) as secondary glaucoma, 10% (n=3) as glaucoma suspects and 3% (n=1) as rubeotic glaucoma.
Other ocular pathology
The most common co-existing ocular pathology, other than the cause for the PPV, was diabetic retinopathy. Of the 53 eyes included in this study, 10 had a co-existing diagnosis of diabetic retinopathy. Three of these 10 went on to develop neovascular glaucoma.
Discussion
The most common glaucoma-related diagnoses following a PPV were:
- ocular hypertension (36%)
- secondary glaucoma (30%)
- glaucoma suspect (11%)
- NTG (8%)
Diagnoses of primary open angle glaucoma or narrow angle glaucoma were rare. Half of all eyes had a postoperative increase in IOP, and of these eyes the majority went on to have a diagnosis of ocular hypertension or secondary glaucoma.
Emergency and elective vitrectomy is a very common procedure in most eye units in the UK. Our study demonstrated that a significant proportion of patients developed OHT or glaucoma following uncomplicated vitrectomy; patients with elevation of IOP in the early postoperative period are particularly prone. Our study aims to increase awareness of this risk amongst ophthalmologists in general but particularly amongst vitreoretinal surgeons. We also believe that patients should be made aware of this potential risk during the consent process for vitrectomy. We would recommend that patients with raised IOP in the postoperative period are referred to the local glaucoma service for monitoring; patients with normal IOP in the postoperative period need to be warned of the risk of developing OHT or glaucoma and advised long-term monitoring by their optician.
We have introduced these recommended changes in our department. A warning of a potential postoperative rise in IOP is now a part of our consent process for vitrectomy. We hope to follow up this retrospective audit with a prospective study moving forwards and are in the process of collecting this data at present.
Learning points
- OHT and secondary glaucoma following a PPV were common in our glaucoma service.
- The association between PPV and glaucoma is not well recognised and is rarely discussed with patients prior to undertaking a PPV.
- It is important to raise awareness of this association and counsel patients on their increased risk of glaucoma prior to surgery.
- It is important to follow up patients post-PPV to monitor for any rise in IOP.
- Those with existing diabetic retinopathy are at increased risk of developing neovascular glaucoma which needs to be acknowledged by the clinician and discussed with the patient.
Limitations
This study has identified patients who were seen in the glaucoma service following a PPV, however, this chronological timeline does not necessitate cause and effect. Glaucoma and OHT are very common diagnoses in the UK ophthalmic outpatients department and as such a certain proportion of these patients would be likely to develop this condition anyway, regardless of previous vitreoretinal surgery. The data set is small and does not include a control group and as such we are unable to carry out statistical analyses to identify associations between PPV and glaucoma diagnoses. As with all retrospective case notes reviews some data is missing from the records.
References
1. Miele A, Govetto A, Fumagalli C, et al. Ocular hypertension and glaucoma following vitrectomy: A Systematic Review. Retina 2018;38(5):883-90.
2. Lalezary M, Kim SJ, Jiramongkolchai K, et al. Long-term trends in intraocular pressure after pars plana vitrectomy. Retina 2011;31(4):679-85.
3. Chang S. LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol 2006;141(6):1033-43.
4. Liang X, Zhang Y, Li YP, et al. Frequency and Risk Factors for Neovascular Glaucoma After Vitrectomy in Eyes with Diabetic Retinopathy: An Observational Study. Diabetes Ther 2019;10(5):1801-9.
5. Kwon JW, Jee D, La TY. Neovascular glaucoma after vitrectomy in patients with proliferative diabetic retinopathy. Med (United States) 2017;96(10):e6263.
6. Sakamoto M, Hashimoto R, Yoshida I, et al. Risk factors for neovascular glaucoma after vitrectomy in eyes with proliferative diabetic retinopathy. Clin Ophthalmol 2018;12:2323‑9.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME








