Age-related macular degeneration (AMD) is the primary cause of blindness in the developed world and is accountable for more than one half of sight impairment registrations within England and Wales [1]. AMD is prevalent in people aged 60 years and older and diagnoses are on the rise due to globally increasing longevity [2].
As a result, low vision services are expected to become overwhelmed with people who are visually impaired. In this programme of work, we aimed to shine a spotlight on the visual experience in people with non-neovascular AMD.
The existing literature uses a variety of terminologies and classification systems for AMD. It is generally agreed that AMD can be identified as one of two forms: the more common dry AMD (non-neovascular) and wet AMD (neovascular). Typically, dry AMD causes a slow, progressive and irreversible loss of vision and can be further categorised into three stages of varying severity: early, intermediate and late (geographic atrophy [GA]) [3].
Characteristics of early and intermediate AMD consist of the presence of macular drusen and retinal pigment epithelium (RPE) anomalies of the macula. If the disease progresses into GA, this will lead to central scotomas (blind-spots) and permanent loss of visual acuity. Symptoms associated with AMD include blurred vision, distortion and scotomas, but as early stage AMD is usually asymptomatic, it often goes unnoticed. There are a number of known risk factors associated with AMD, such as increasing age, smoking, a history of cataract surgery and family history [4].
Describing the visual experience of people with AMD
An accurate representation of visual symptoms experienced by people with dry AMD is important for raising awareness of the condition and educating patients. We explored whether typical images used to depict the vision of someone with AMD such as Figure 1 are a realistic example of what people with AMD see.

Figure 1: Example image frequently used for education about AMD. The image on the left shows ‘normal vision’.
The image on the right shows a typical portrayal of ‘vision with AMD’;
images such as this were found to be an inaccurate representation [5].
To do this, we developed a list of suitable descriptors to effectively describe the visual experience encountered by people with a range of AMD disease severity [5]. The most common descriptors of visual experience were ‘blurred’, ‘parts missing’ and ‘distorted’. Most people did not report the typical images illustrating a central ‘patch’ of distortion surrounded by a clear periphery to correctly represent their visual symptoms. This key finding highlighted the general misunderstanding of the true visual experience in people with AMD and the fact that the images currently used to educate people on the condition are unrealistic for many people suffering from AMD.
The impact of the continued use of these images may result in individuals misunderstanding the severity of their condition. This may conclude in people overlooking disease management strategies to minimise AMD progression such as self-monitoring vision and lifestyle changes.
‘Real-world’ vision testing
In AMD, everyday activities such as reading a book, looking for the desired product on a shop shelf, or recognising faces may become difficult and sometimes almost impossible [6]. This is due to loss of central vision. Hence, a diagnosis of AMD can have a big impact on an individual’s vision related quality of life (QoL) and can reduce their independence [7]. Armed with the knowledge that people with AMD are impaired in object recognition [8], facial recognition [9] and mobility [6], we aimed to develop measures that mimic ‘real-world’ visual function for those with AMD. In the Crabb Lab at City, University of London, we have conducted multiple investigations to assess whether computer-based tasks involving searching for objects, facial recognition and mobility could be a feasible measure for AMD and disease severity.
Searching for objects and dry AMD
Visual search is an important everyday function and people with AMD self-report difficulties in searching and finding things [10]. Visual search is ordinarily assessed within lab settings via synthetic targets and distractors. However, these measures are not easily comparable to real life visual search tasks and glaucoma patients reportedly find it more difficult to locate items in an everyday scene compared to synthetic search tasks [11]. Therefore, the assessments we designed in the Crabb Lab aimed to replicate ‘real-world’ visual tasks [12]. Participants searched for a target item within a computer displayed image of an everyday indoor or outdoor scene (Figure 2). We assessed the time it took for people with and without AMD to locate the item.

Figure 2: Example of photographs used in this experiment. In this image, participants were asked
to find the name of the street [10]. (Images were displayed at a higher resolution than shown here.)
Thirty-three people with healthy vision and 31 people with dry AMD, aged 60 years or older were involved in the study. All participants were screened for cognitive defects, eye diseases and assessed for AMD severity [3]. We found that on average, median search durations for people with AMD were almost twice as long as those for people with healthy vision. A large number of the participants with AMD, including all of those classified as having GA in their better eye performed outside the 90% limit established as ‘normal’ performance by the people with healthy vision. Our results highlighted the impairment of a GA diagnosis with this type of everyday task. Moreover, some people with intermediate AMD may have more difficulties with these sorts of activities than previously believed.
Recognising faces and dry AMD
Face recognition is another everyday activity that people with AMD may struggle with. This can lead to embarrassment or nervousness in social situations which, in turn, can lead to social segregation [13]. A study assessing face recognition in people with AMD found that 29 out of 30 people surveyed reported difficulty recognising familiar faces in the street and a third of those experienced embarrassment [9]. Furthermore, people with AMD also struggle deciphering facial expressions, reporting missing elements of conversation as a result [9]. We conducted an investigation to assess face recognition specifically in dry AMD [14]. We used a computer-based test featuring an adapted version of the Cambridge Face Memory Test (15) which prompted participants to choose the face they had previously been shown from a selection of faces (Figure 3).
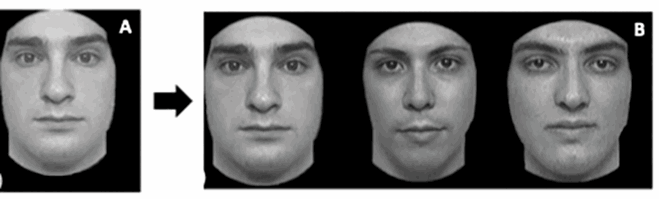
Figure 3: An example task from the Cambridge Face Memory Test. Participants were asked to familiarise
themselves with a face (A). Participants were then asked to tell the operator
which face matched the one they had just viewed (B) [14].
As before, all people involved in the study were screened for cognitive defects, other eye diseases and AMD disease severity [3]. This time, only five participants (four with GA) performed outside the 90% limit established as ‘normal’ performance by the people with healthy vision. Notably, individuals with GA who had foveal damage and larger lesions scored worse than those with smaller lesions and no foveal involvement. With regards to group differences, those with GA correctly identified fewer faces than the early and intermediate AMD groups. Our results indicated that people with early and intermediate dry AMD perform as well as people with healthy vision on a face recognition task and may not have obvious difficulties with face recognition until the disease has progressed into GA.
In comparison, people with GA (particularly those with larger lesions and atrophy in the fovea) are more likely to have difficulty recognising faces. Moreover, these results show a strong association between worsening contrast sensitivity and poorer performance in face recognition tasks and supports existing evidence suggesting that contrast sensitivity may be useful as a predictor for real-world visual function in people with AMD [14].
Mobility and dry AMD
Mobility is crucial for well-being and is widely believed to be associated with improved physical and mental health [16]. The negative impact of AMD on mobility has been extensively documented and has been described as the most frequent subject of published studies on real-world visual function in AMD [6]. However, the majority of this research is focused on wet AMD.
There are multiple ways of assessing mobility in people with AMD including self-report measures [17] and mobility tasks in lab-settings [18]. After reviewing the literature, we realised there were limited studies on the association of anxiety with mobility in people with AMD. We deemed this important because anxiety may result in decreased willingness to retain mobility. Therefore, we aimed to assess self-perceived anxiety and concern associated with everyday mobility situations in people with dry AMD using a computer-based test to identify any anxiety predictors. Specifically, we were looking to measure the effect of AMD severity on mobility anxiety [19]. Our test consisted of a series of 18 short videos (Figure 4). Participants were asked to press down on a button whenever they felt the footage illustrated a situation that induced anxiety. The pressure exerted on the button was then assessed and related to answers on a health-related QoL questionnaire.
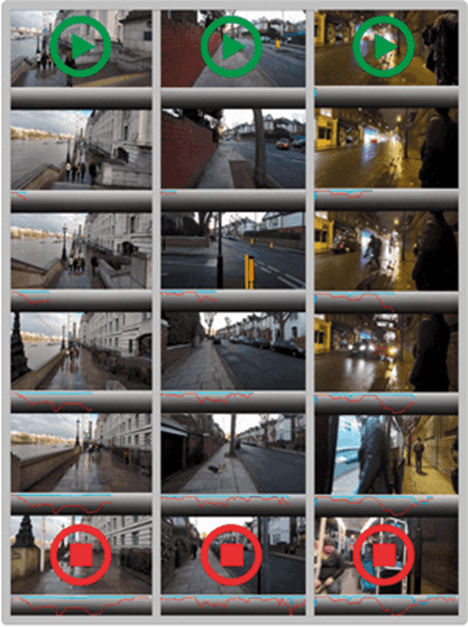
Figure 4: Example still shots from three of the movies with corresponding pressure traces.
Lines represent the mean responses from people with No / Early AMD (blue) and Intermediate AMD / GA (red) [19].
Thirty people were included in the study and as before, people with AMD were assessed for disease severity [3]. In certain videos, specific events triggered more anxiety in people with intermediate AMD and GA compared to those with no and early AMD. Four such videos involved navigating stairs and others included avoiding cyclists on a pathway, walking along a cliff path and navigating a crowd and then crossing a road at night [19]. Our results supported previous evidence that people with intermediate AMD experience more impairment in environments of low luminance than those without AMD [20]. Overall, participants with intermediate AMD or GA recorded greater pressure than those with early and no AMD. Hence, this study suggested that people with intermediate and GA experience higher levels of anxiety associated with mobility. Moreover, this computer-based test has proved to provide a ‘safe’ environment for testing mobility anxiety, which is removed from physical obstacle courses, but retains a level of ‘real-world’ applicability.
What we found
We have successfully investigated the use of computer-based tests to assess patient relevant aspects of visual function including visual search, face recognition and feelings about mobility. Furthermore, we found that the tasks are engaging and our participants enjoyed doing them. The fact that these tests are not simply clinical charts with synthetic optotypes, but surrogates of real-world situations may be the reason for this. In addition, as our tests are able to distinguish between grades of AMD disease severity, we would argue that the assessment of problems with ‘real-world’ visual function has the potential to be used in trials and the clinic. Of course, more work is needed to take the tests out of our laboratory. One way to do this would be to offer them as a battery of assessments on a tablet platform. Doing this would increase their accessibility as they can be easily conducted outside of low vision clinics such as in waiting rooms within hospitals and residential care homes.
Our investigation into self-reported description of vision loss in dry AMD identified frequent descriptors used by people with dry AMD as ‘blurred’, having ‘missing parts’ and ‘distorted’. Clinicians may subsequently use these findings to aid the diagnosis of dry AMD. Additionally, our findings have identified that the images commonly used to illustrate the visual experience of people with dry AMD are not reflective of what people with dry AMD truly see. These results should be useful in future patient management and educating the public about the everyday effects of AMD.
References
1. Quartilho A, Simkiss P, Zekite A, et al. Leading causes of certifiable visual loss in England and Wales during the year ending 31 March 2013. Eye 2016;30(4):602-7.
2. Klein R, Chou C-F, Klein BEK, et al. Prevalence of age-related macular degeneration in the US population. Arch Ophthalmol 2011;129(1):75.
3. Ferris FL, Wilkinson CP, Bird A, et al. Clinical classification of age-related macular degeneration. Ophthalmology 2013;120(4):844-51.
4. Chakravarthy U, Wong TY, Fletcher A, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol 2010;10(1):31.
5. Taylor DJ, Edwards LA, Binns AM, Crabb DP. Seeing it differently: self-reported description of vision loss in dry age-related macular degeneration. Ophthalmic Physiol Opt 2018;38(1):98-105.
6. Taylor DJ, Hobby AE, Binns AM, Crabb DP. How does age-related macular degeneration affect real-world visual ability and quality of life? A systematic review. BMJ Open 2016;6(12):e011504.
7. Cahill MT, Banks AD, Stinnett SS, et al. Vision-related quality of life in patients with bilateral severe age-related macular degeneration. Ophthalmology 2005;112(1):152-8.
8. Tran THC, Rambaud C, Despretz P, Boucart M. Scene Perception in Age-Related Macular Degeneration. Investig Opthalmology Vis Sci 2010;51(12):6868.
9. Tejeria L, Harper RA, Artes PH, Dickinson CM. Face recognition in age related macular degeneration: Perceived disability, measured disability, and performance with a bioptic device. Br J Ophthalmol 2002;86(9):1019-26.
10. Taylor DJ, Smith ND, Crabb DP. Searching for objects in everyday scenes: Measuring performance in people with dry age-related macular degeneration. Investig Ophthalmol Vis Sci 2017;58(3):1887-92.
11. Smith ND, Crabb DP, Garway-Heath DF. An exploratory study of visual search performance in glaucoma. Ophthalmic Physiol Opt 2011;31(3):225-32.
12. Crabb DP, Taylor DJ. Searching for unity: Real-world versus item-based visual search in age-related eye disease. Behav Brain Sci 2017;40:e135.
13. Yardley L, McDermott L, Pisarski S, et al. Psychosocial consequences of developmental prosopagnosia: A problem of recognition. J Psychosom Res 2008;65(5):445-51.
14. Taylor DJ, Smith ND, Binns AM, Crabb DP. The effect of non-neovascular age-related macular degeneration on face recognition performance. Graefe’s Arch Clin Exp Ophthalmol 2018;256(4):815-21.
15. Duchaine B, Nakayama K. The Cambridge Face Memory Test: Results for neurologically intact individuals and an investigation of its validity using inverted face stimuli and prosopagnosic participants. Neuropsychologia 2006;44(4):576-85.
16. Sengupta S, Nguyen AM, van Landingham SW, et al. Evaluation of real-world mobility in age-related macular degeneration. BMC Ophthalmol 2015;15(1):9.
17. van Landingham SW, Massof RW, Chan E, et al. Fear of falling in age-related macular degeneration. BMC Ophthalmol 2014;14:10.
18. Hassan SE, Lovie-Kitchin JE, Woods RL. Vision and mobility performance of subjects with age-related macular degeneration. Optom Vis Sci 2002;79(11):697‑707.
19. Taylor DJ, Jones PJ, Smith ND, et al. Measuring real-time anxiety during simulated mobility scenarios in people with non-neovascular age-related macular degeneration (AMD). Invest Ophthalmol Vis Sci 2018;59(9):1290.
20. Wu Z, Guymer RH, Finger RP. Low luminance deficit and night vision symptoms in intermediate age-related macular degeneration. Br J Ophthalmol 2016;100(3):395-8.
Web: www.staff.city.ac.uk/crabblab/#/
Twitter: https://twitter.com/crabblab
Declaration of competing interests: David Crabb has been recipient of unrestricted research grants from Allergan, Roche, Novartis, Santen and Centervue, has been paid speaker fees from Allergan, Roche and Santen and consultancy fees from Allergan.
COMMENTS ARE WELCOME