The need for eyecare services in low- and middle-income countries
Recent global estimates (2020) suggest that there is more than a three-fold difference in the prevalence of all categories of visual loss (presenting visual acuity <6/12 in the better eye) between South Asia (over 11%) and high-income countries (almost 3%). The regions with the highest number of people affected are in Asia, North Africa, the Middle East, and Western sub-Saharan Africa regions, reflecting the large populations and / or the higher prevalence in these regions.
Globally, 43 million people are blind (<3/60 in the better eye), 552 million are vision impaired (6/12 to 3/60) and 510 million adults have near vision impairment [1]. Overall, 1062 million people are affected – almost one in seven of the global population. Approximately 90% live in low- and middle-income countries (LMICs) and 55% are women. Cataract and uncorrected refractive errors, which are readily treatable, together account for almost 50% of blindness and over 80% of mild / moderate vision impairment (<6/18-3/60) [1].
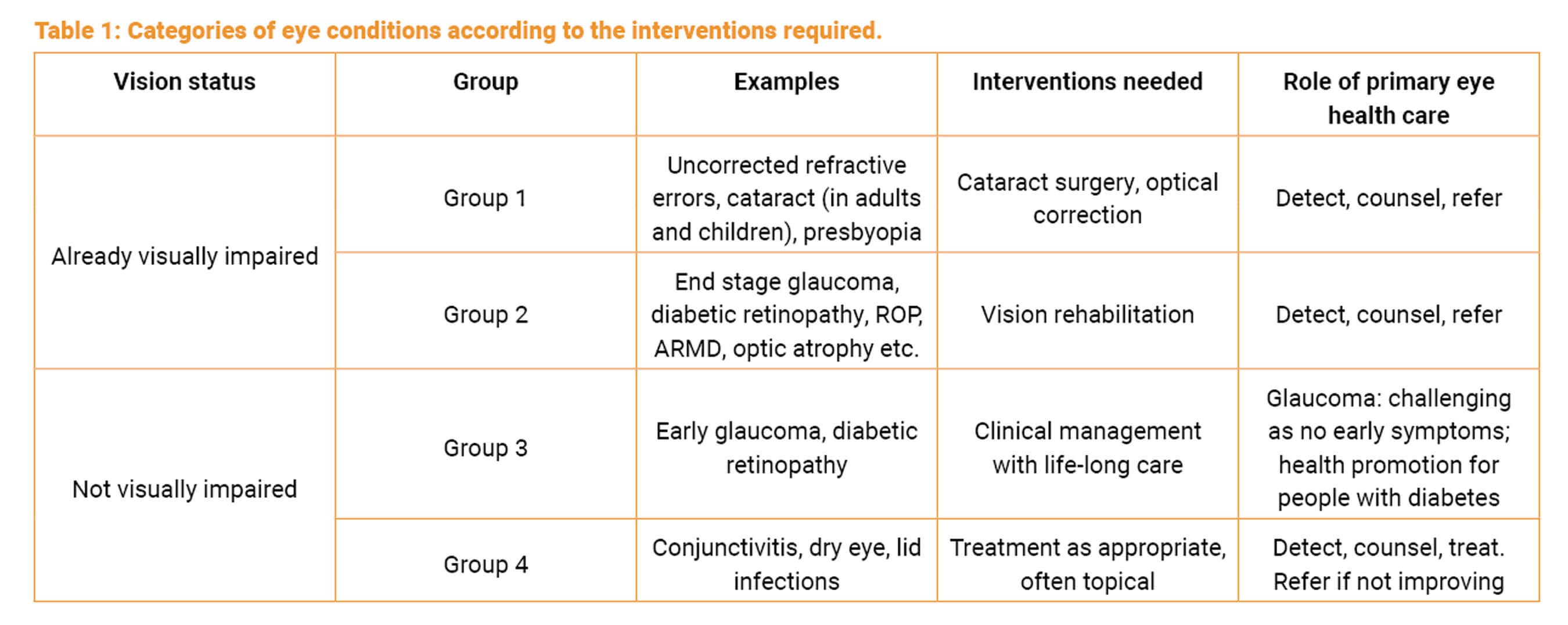
In addition to the large number of people with vision loss where sight can be restored, there are other eye conditions which require intervention (Table 1) [2].
There are some data on Group 3 conditions:
- 76 million people are estimated to have glaucoma, the majority of whom have not been diagnosed.
- 463 million people have diabetes, 160 million of whom have diabetic retinopathy [1].
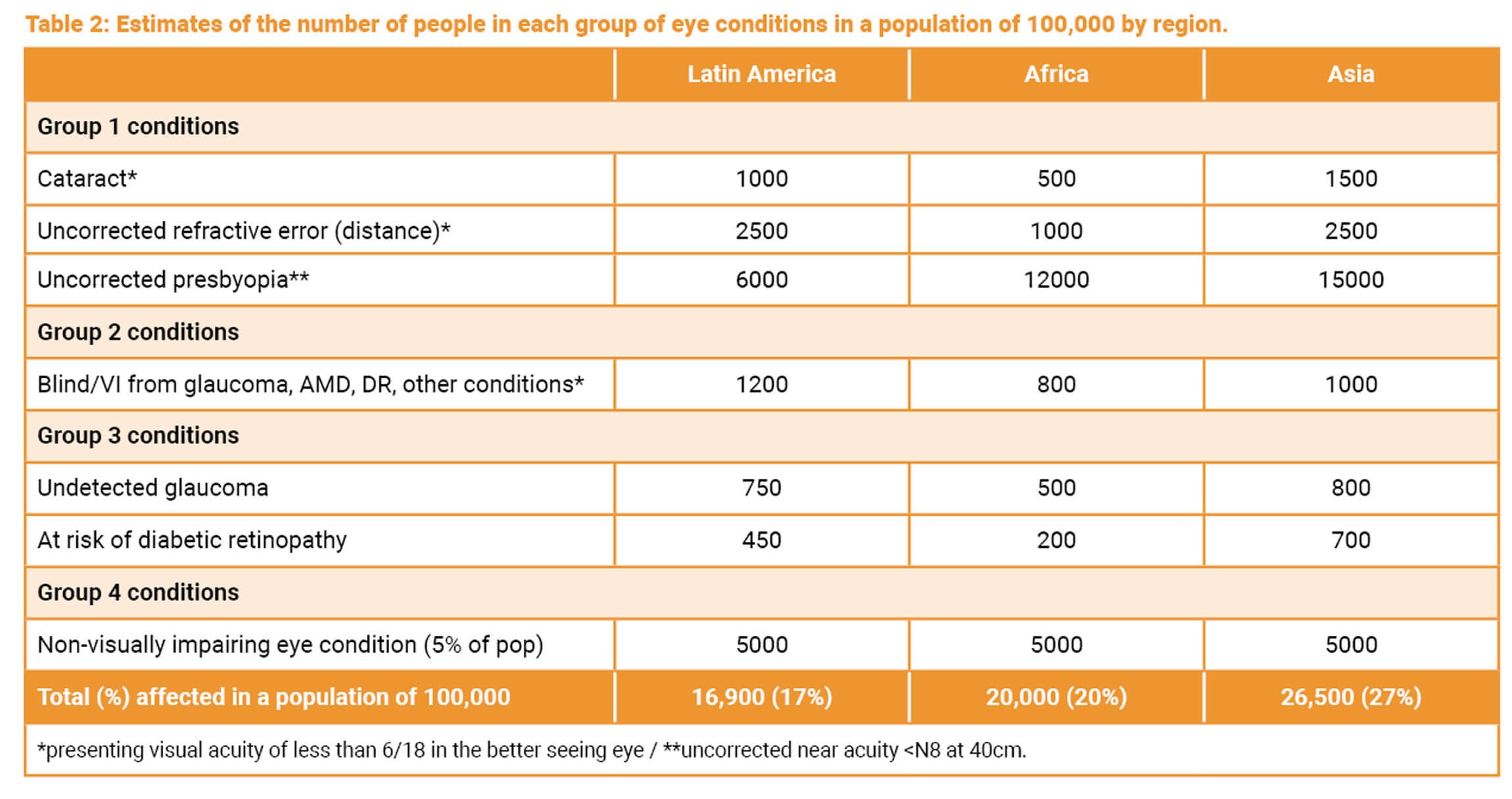
There are limited data on Group 4 conditions, largely because they are not yet included in population-based surveys. Despite the limited data, it is possible to estimate the number of people who need eyecare services per 100,000 population in different world regions using a range of assumptions (Table 2) [2].
To meet the need at a population level, eyecare services are required at each level of service delivery, i.e. at primary, secondary and tertiary levels. In low- and middle-income settings it is vital that services are taken as close as possible to communities, as inequitable access to care is a major issue. For example, in Nigeria, non-literate, rural women have a 7.3-times higher prevalence of cataract blindness than literate urban women [3]. In Nigeria and Sri Lanka, 48% of cataract blindness is among unmarried women (mostly widows) [4].
Primary eye health care
The World Health Organization (WHO) and other bodies are increasingly recognising and advocating for better primary health care to improve population health. WHO defines primary health care as “a whole-of-society approach to health that aims to maximise the level and distribution of health and well-being” through three components [5]:
a. Primary care and essential public health functions as the core of integrated health services
Primary care refers to clinical services delivered by healthcare professionals working in the community. In high-income countries, this care may be provided by family physicians; in low-income settings, general nurses or clinical officers provide these services in primary health clinics. This means that the type of care delivered at this level is very context specific.
"A whole-of-society approach to health that aims to maximise the level and distribution of health and well-being [5]"
Essential public health functions and action can include a range of activities, such as screening for disease or risk factors for disease such as hypertension, and specific preventive measures such as immunisation. Integrated services means that primary care is the essential, broad base of accessible healthcare for a population, with good referral mechanisms from primary to secondary level.
b. Multisectoral policy and action
This component is included because many underlying factors increase the risk of illness, such as overcrowding, air pollution, unclean water, poor sanitation and unhealthy food, as well as lack of public transport to access care. Policies are needed to ensure that these underlying factors are addressed. To be effectively implemented, these policies need political will and adequate financing.
c. Empowered people and communities
People who are empowered know what causes disease, know what to do to remain healthy, where to go when they become sick, and how to include those who are disabled. Empowered people have the knowledge (health literacy) and ability (agency) to bring about the changes required.
Activities to improve health literacy, create a healthy environment, and encourage government policies that support health are known as health promotion. Primary eye healthcare (as opposed to primary eyecare) should, therefore, include providing basic eyecare services as well delivering the two components of health promotion (Figure 1) [6].
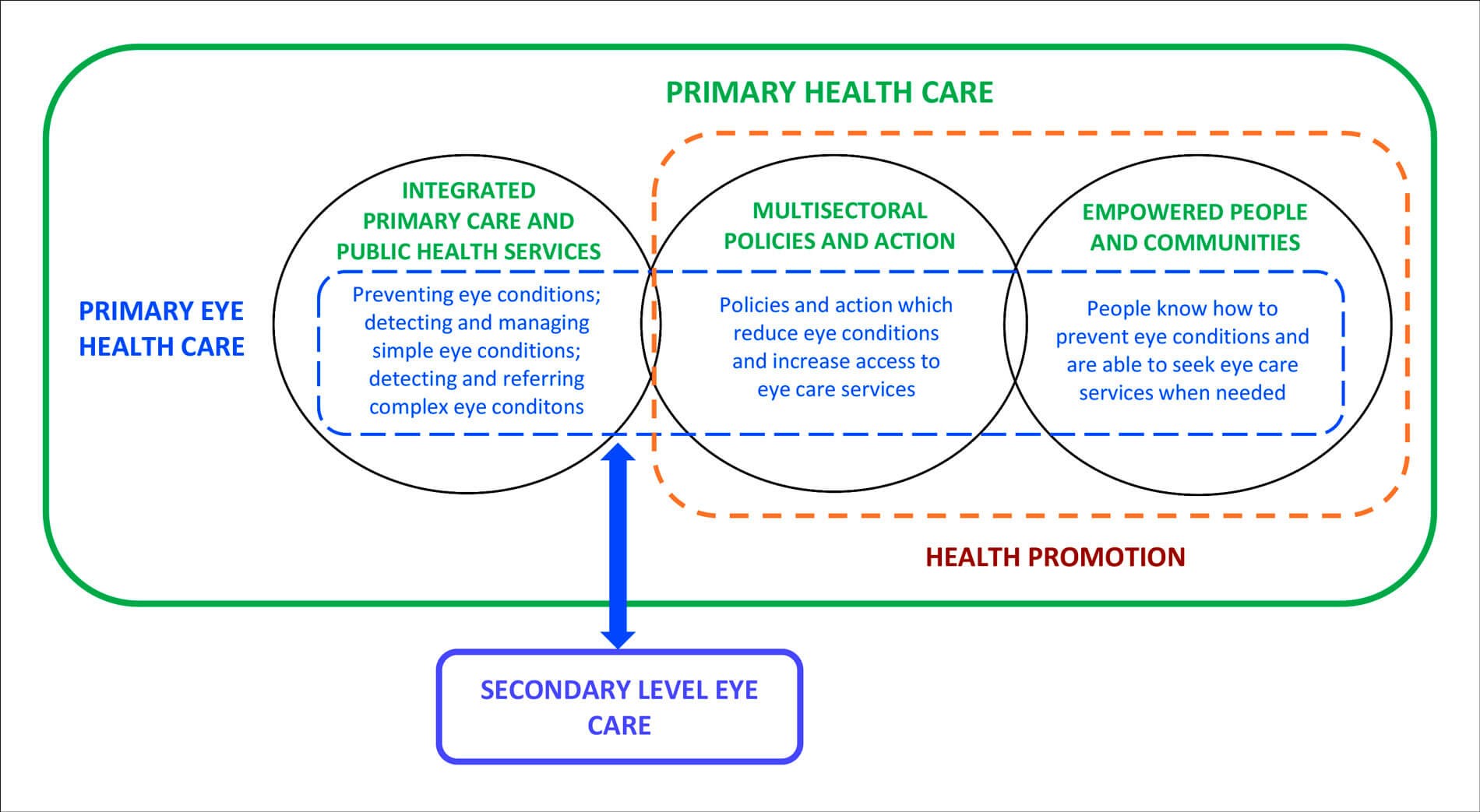
Figure 1: Schematic representation of primary eye healthcare [6].
As shown in Table 1, primary eye healthcare has the potential to play a major role in reducing avoidable vision loss, particularly from cataract and uncorrected refractive errors. Managing simple eye conditions, such as conjunctivitis, at primary level would also reduce the burden on secondary and tertiary facilities, allowing staff to focus on more complex conditions.
Integrating eyecare into primary healthcare in LMICs
Including primary eye health care in policies for primary healthcare and in training curricula for primary healthcare workers has many advantages, such as greater coverage and sustainability, as the minimal additional cost of training in eyecare is borne by the training institutions. However, most examples in low-income countries include in-service training of staff who are already in post, but the cost of training limits the coverage of this approach. In addition, the scope is also limited, as eye health promotion is not usually included.
Another approach to delivering primary eyecare is vision centres, which are usually provided and managed by large, non-governmental providers of eyecare, such as Aravind Eye Care System and LV Prasad Eye Institute in India. Vision centres are usually staffed by eyecare professionals such as optometrists, and in some cases the centres are linked by telemedicine to the base hospital [7]. This approach can be very effective but is not replicable in Africa where the majority of healthcare is provided by governments or private providers.
Peek Vision is another approach to bringing eyecare closer to people [8]. Community or primary level health workers are trained to screen the visual acuity of community members or school children using a mobile phone application, with referral of those who fail to centres with eyecare professionals. Large-scale programmes are being implemented in Asia and Africa, and over 2,000,000 people have been screened to date. In Pakistan, the Peek programme led to fewer patients with minor eye complaints attending secondary level eyecare services.
Examples of primary eyecare in Africa
a. Rwanda
In Rwanda, primary eyecare has been a priority for over 20 years. Services are fully integrated into the government health system, including a training curriculum, essential medicines and technology, and eye conditions are included in the health management information system and health insurance scheme. The provision of spectacles has been supported by a non-government organisation. A recent evaluation showed that over 2000 nurses had been trained and almost a million eye examinations took place over a four-year period [9].
In 2020, the WHO Regional Office for Africa (AFRO) launched a primary eyecare package for Africa [10], based on the Rwanda curriculum. It includes five management algorithms for common presenting complaints (e.g. red eye; loss of vision) and health messages for eye health promotion.
b. Nigeria
A key challenge of integrating eye health care into primary healthcare is that the services delivered may be limited by the capacity of the health system at primary level.
We recently undertook a study in Nigeria to determine the capacities needed to deliver the WHO AFRO package and to assess capacity gaps at primary level. The study identified many limitations, such as understaffing, lack of medication, inadequate supervision, a major focus on maternal and child health and limited health promotion activities. Few adults attended the 48 study facilities, and if patients with eye conditions did present, their attendance was not recorded, and there were no formal referral mechanisms [11–14].
"In Nigeria there are policies for strengthening general primary health care, which if implemented would go a long way to addressing [capacity] gaps"
However, in Nigeria there are policies for strengthening general primary health care, which if implemented would go a long way to addressing these gaps. A further study entailed interviews with policy makers who fully endorsed the inclusion of the WHO AFRO package into the training curriculum of senior primary health workers at national level, as they recognised the huge unmet need for eyecare at the primary level [15].
c. Tanzania
Eyecare for children is now fully integrated into the WHO / UNICEF Integrated Management of Newborn and Childhood Illness (IMNCI) in Tanzania. IMNCI is the blueprint for general child health in over 100 countries. This came about as a result of a series of studies and a window of opportunity for policy change [16–18]. The training curriculum includes fundal / red reflex testing to detect cataract and retinoblastoma, and all the in-service training is being undertaken by the Ministry of Health. We anticipate that other countries will also adopt this approach, and our goal is that global IMNCI recommendations will eventually include eyecare for children.
Conclusion
Bringing basic eyecare and eye health promotion closer to people through integration into government primary-level health policies and services needs to be the bedrock of eyecare delivery and an important component of strengthening the eye healthcare system, so that “no-one is left behind”.
References
1. Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9(4):e489–e551.
2. Gilbert C, Piyasena MP. Why is primary eye health care needed? Community Eye Health 2021;34(113):67–9.
3. Ramke J, Zwi AB, Lee AC, et al. Inequality in cataract blindness and services: moving beyond unidimensional analyses of social position. Br J Ophthalmol 2017;101(4):395–400.
4. Ramke J, Kyari F, Mwangi N, et al. Cataract Services are Leaving Widows Behind: Examples from National Cross-Sectional Surveys in Nigeria and Sri Lanka. Int J Environ Res Public Health 2019;16(20):3854.
5. Operational framework for primary health care: transforming vision into action (2020). World Health Organization.
https://www.who.int/publications/
i/item/9789240017832
6. Gilbert C, Faal H, Allen L, Burton M. What is primary eye health care? Community Eye Health 2021;34(113):70–2.
7. Misra N, Khanna RC, Mettla AL, et al. Role of teleophthalmology to manage anterior segment conditions in vision centres of south India: EyeSmart study-I. Indian J Ophthalmol 2020;68(2):362–7.
8. Peek Vision.
https://peekvision.org
9. Yip JLY, Bright T, Ford S, et al. Process evaluation of a National Primary Eye Care Programme in Rwanda. BMC Health Serv Res 2018;18(1):950.
10. Primary Eye Care training manual. World Health Organization AFRO region.
https://www.afro.who.int/publications/
primary-eye-care-training-manual
11. Aghaji A, Burchett HED, Hameed S, Gilbert C. Assessing the capacity of primary health care facilities in Nigeria to deliver eye health promotion: Results of a mixed-methods feasibility study. PLOS Glob Public Health 2022;2(11):e0000645.
12. Aghaji A, Burchett HED, Mathenge W, et al. Technical capacities needed to implement the WHO’s primary eye care package for Africa: results of a Delphi process. BMJ Open 2021;11(3):e042979.
13. Aghaji A, Burchett HED, Oguego N, et al. Primary health care facility readiness to implement primary eye care in Nigeria: equipment, infrastructure, service delivery and health management information systems. BMC Health Serv Res 2021;21(1):1360.
14. Aghaji A, Burchett HED, Oguego N, et al. Human resource and governance challenges in the delivery of primary eye care: a mixed methods feasibility study in Nigeria. BMC Health Serv Res 2021;21(1):1321.
15. Okolo EO HS, Aghaji A, Gilbert CE. Acceptability of preservice training of primary health care workers in Nigeria using the World Health Organization AFRO Primary Eye Care Package. Prim Health Care Res Dev. Submitted.
16. Mafwiri M, Malik AN, Gilbert C. Integrating child eye health within primary health care: a case study. Community Eye Health 2017;30(100):78–9.
17. Malik ANJ, Mafwiri M, Gilbert C. Integrating primary eye care into global child health policies. Arch Dis Child 2018;103(2):176–80.
18. Malik ANJ, Mafwiri M, Gilbert C, et al. Integrating eye health training into the primary child healthcare programme in Tanzania: a pre-training and post-training study. BMJ Paediatr Open 2020;4(1):e000629.
19. Primary eye health care: the foundation for universal access to eye health (2021). Community Eye Health Journal.
https://www.cehjournal.org/article/primary
-eye-health-care-the-foundation-for
-universal-access-to-eye-health/
[All last accessed November 2023]
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME














