The prevalence of certain retinal conditions such as diabetic retinopathy and age-related macular degeneration (ARMD) is projected to grow substantially over the next decades. Estimates for the projected growth in burden on eye services for diabetic retinopathy and neovascular ARMD in the UK are approximately 60% over the next 20 years.
Intravitreal anti-vascular endothelial growth factor agents (anti-VEGF) are an effective treatment for macular oedema and have become the primary treatment modality, and the most common intraocular procedure, worldwide. Patients undergoing treatment require multiple hospital visits, putting considerable strain on resources and capacity. Doctor shortages are set to compound the problem. In the UK, a clear policy has been set to expand the roles of healthcare professionals, to help plug the gap. These new roles, along with virtual clinics, have been proposed as part of the solution in increasing service capacity.
With the introduction of virtual clinics into ophthalmology, and the ever-growing demand for patients to be seen, the career progression opportunities for an ophthalmic photographer have never looked more exciting. Ophthalmic photographers are highly trained individuals who are exposed to a variety of retinal pathology through imaging.

Figure 1: The specialist ophthalmic imaging team at the Leicester Royal Infirmary Hospital
pictured from left to right: Andrew Farmer, Kayleigh Parker and Lee Daines.
A new role within University Hospitals of Leicester NHS Trust has been created that allows experienced ophthalmic photographers Kayleigh, Andy and Lee (Figure 1) to expand their role in becoming ‘specialist ophthalmic photographers’. This opportunity has allowed the specialists to participate in dedicated specialist medical retina virtual clinics by independently interpreting optical coherence tomography (OCT) images, making clinical decisions regarding patients’ treatment pathway, and communicating the chosen outcome with the patients.
The issue of clinical negligence was discussed extensively within the department and trust. The introduction of the new role was made possible by initiating a quality improvement project by the Medical Retina Consultants Rossella Anzidei and Vasilis Konidaris, who produced a comprehensive policy document, detailing the proposal. This was submitted to the relevant heads of departments, and the Trust Audit / Quality Improvement Department. Formal approval as a quality improvement project was obtained before commencement.
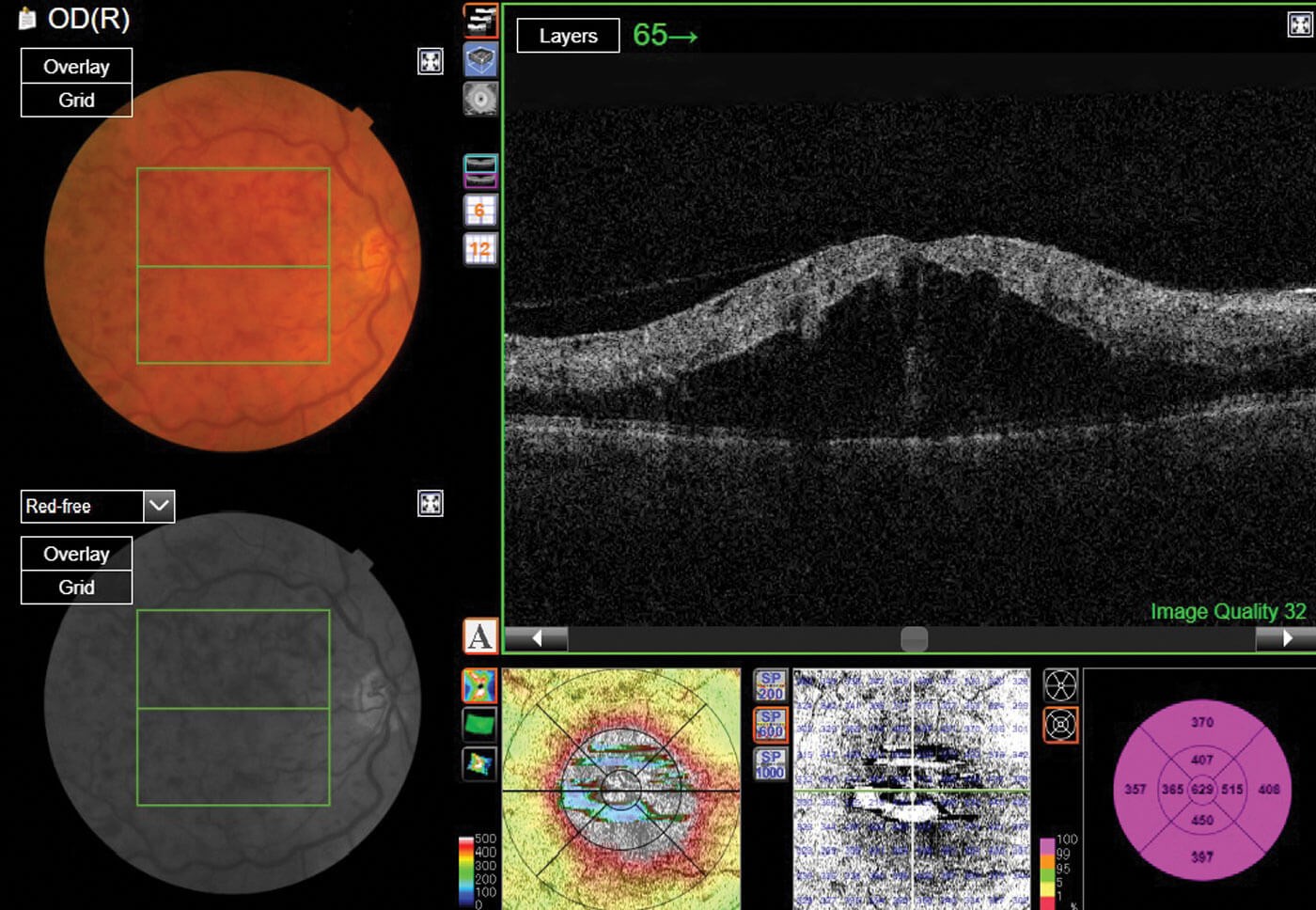
Figure 2: An optical coherence tomography (OCT) scan of a branch retinal vein occlusion (BRVO).
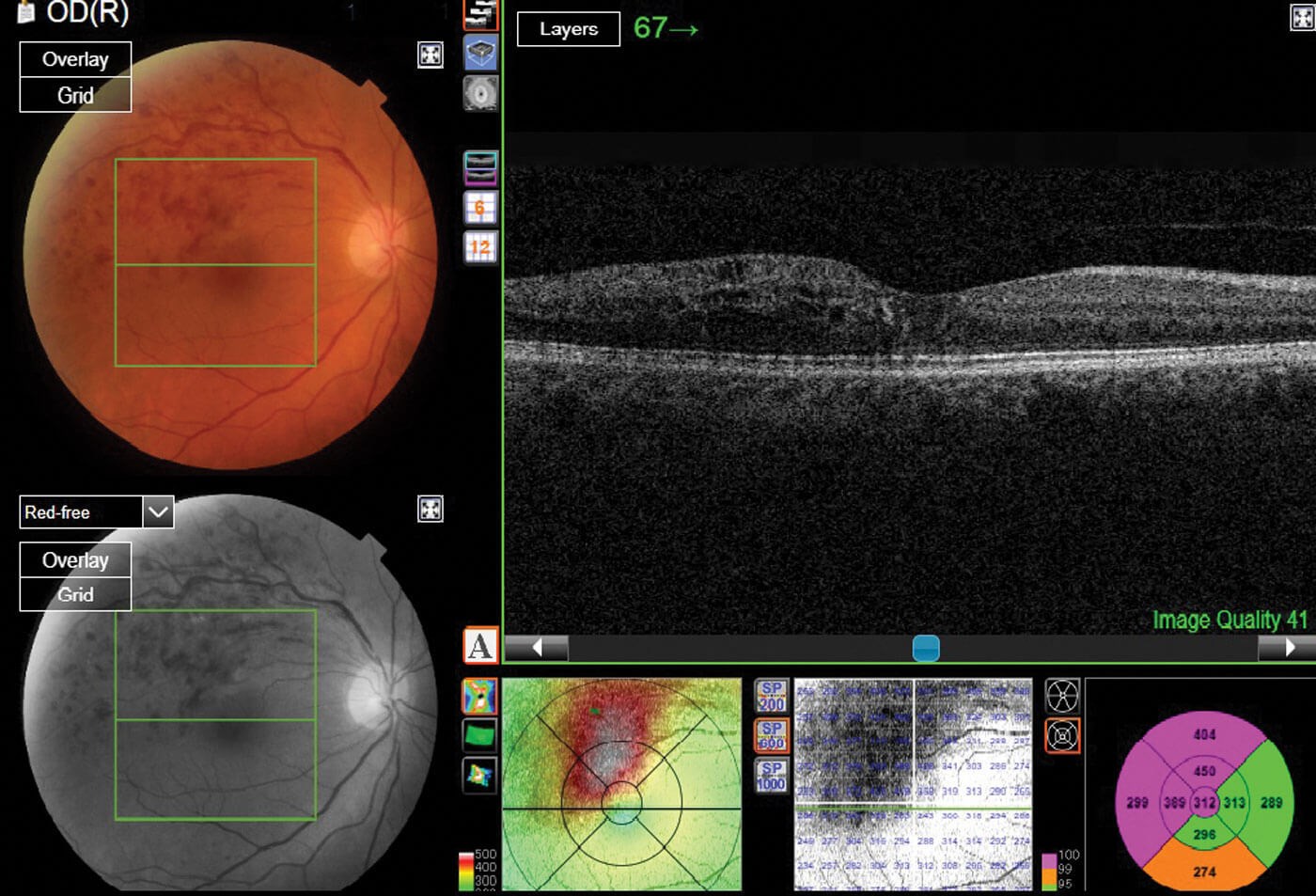
Figure 3: An optical coherence tomography (OCT) scan depicting a central retinal vein occlusion (CRVO).
Ensuring the highest standards of patient care and safety were of the utmost importance throughout this process, and a rigorous training programme was established. The relevant literature (online and OCT atlas book) was reviewed by the team. Following that, weekly meetings were established, where we went through individual patient cases, reviewing the notes and the OCT scans (Figures 2 & 3) with the consultants, discussing the findings and the rationale for decisions to treat or monitor. Then, documentation in the notes, and the clinical outcome completed. Treatment pathways have been established, to assist the decision to treat or monitor. A training competency booklet and evidence portfolio was created, requiring independent assessment of 100 cases. For each assessment six key criteria were required to be met: specialists had to be able to demonstrate a good knowledge of the anatomy and physiology of the eye as well as a good knowledge of various eye conditions; be able to assess the OCT scan and ensure the correct treatment pathway is chosen; work independently and accurately record their findings and, finally, complete any paperwork required and dictate letters.
To enable assessments to take place, a scoring system for each of the above criteria ranging from zero to four was created; a score of two or higher was required in order to show a competent and safe level of practice. A score of 0-1 demonstrated an unsafe or low level competence and therefore was deemed as un-passable, whereas a score of 2-4 displayed competent or even expert practice. Upon successful completion of the competency training package, the specialists were able to undertake all of these duties independently with the consultants selecting notes randomly to ensure no adverse events had occurred.
Upon initial appointment into our role, the virtual clinics assigned to us involved assessing common medical retina conditions, including ARMD, central and branch retinal vein occlusions, and diabetic macular oedema. These patients were previously diagnosed following a clinic appointment or had already been on a treatment pathway. As specialists, we would assess the OCT and document any findings within the patients’ notes. This not only includes interpretation of the OCT images, but also incorporates comparing visual acuity fluctuations, any prior intravitreal treatments commenced, with the quantity and dates of these noted.
Auditing has played an important part in monitoring the progress and safety of the role. The aim has been to check that the outcomes provided by the specialists match those of the consultants. To date, we have been audited twice with the consultants reviewing 10% of the assessed notes. The results have revealed a 99% agreement outcome, and has concluded that we are practising safely.
As the role has progressed and proven to be a success and an asset within the ophthalmology department, further opportunities have presented themselves. Following additional training a new virtual hydroxychlroroquine screening clinic was created, which was assigned to the specialists. Moreover, during the COVID-19 pandemic, the need to reduce face-to-face appointments has driven the creation of virtual clinics to screen new referrals from community optometrists to the medical retina service, before accessing face-to-face clinics. With the introduction of this virtual clinic, patients are booked for a vision test and an OCT, which is reviewed within 48 hours by the specialist ophthalmic photographers. The patients are triaged according to the imaging findings to either an appropriate face-to-face clinic, referred for treatment, or discharged with a leaflet explaining how to self-monitor their vision and contact numbers for any inquiries.
The introduction of this extended role has been immensely advantageous to our department. It has helped to increase patient capacity, which is beneficial at any given time within a busy ophthalmology department. Additionally, COVID-19 has had an unparalleled impact on all NHS services, making this need even greater. Patient waiting times have been reduced, as virtual clinics have reduced the need to be seen by a clinician at every appointment, which in turn has improved departmental efficiency. The three specialists are able to take on a greater workload on a weekly basis, ensuring patients receive their treatment within the correct timescale. The number of virtual clinics conducted has increased by 70%, reducing waiting times for patients.
Providing ophthalmic photographers with the opportunity to expand their job role has two clear benefits. Firstly, this novel role is financially efficient for the department, as upskilling photographers is less costly than afflicting greater demand upon the consultants’ time or employing more doctors to take on this workload. Secondly, it has provided development opportunities within the Ophthalmic Imaging department, as experienced ophthalmic photographers are being provided with the opportunity to enhance their careers further. It has also provided structure within the Imaging department as the role bestows a supervisory status upon the specialists. Their knowledge and skills are an asset to the ophthalmic photography team, providing guidance to the junior members.
Results derived from our clinical practice were presented at national and international conferences and published in peer-reviewed international journals. The outcomes of the implementation of virtual clinics were published in a peer-reviewed journal, cited by the Royal College of Ophthalmologists. Moreover, the Leicester example of the medical retina service led to a publication of a leaflet distributed to all ophthalmology departments in the UK. The approval of this new role has also gained recognition. The retinal team was awarded the ‘Caring at its Best’ award for innovative ways of working by the University Hospitals of Leicester NHS Trust.
Looking to the future, I anticipate that virtual clinics will only become more prevalent, due to the volume of patient throughput and as a result of the impact of COVID-19. As a result, I believe we as specialists will play a pivotal role in helping to sustain this demand by increasing our clinic workload, ensuring patients can be treated for their sight-threatening conditions in the appropriate timescale required.
“There is nothing permanent except change” (Heraclitus, c. 500 BC). These changes, within Leicester’s medical retina service, have propelled us on a path to achieve clinical excellence. A successful launch of this role in Leicester has demonstrated that there is a place within ophthalmology to extend the careers of an experienced and well-trained ophthalmic imagers to assess certain retinal conditions within the setting of virtual clinics. This exciting opportunity is now seemingly changing the shape of the career of an ophthalmic photographer and opening up a new sector to explore, paving the way for a future full of possibilities.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






