There is a national shortage in the UK in corneal graft material [1,2]. The majority (69%) of corneal transplants in the UK are partial thickness, with 35% being Descemet membrane endothelial keratoplasty (DMEK) [2]. During the preparation of the donor tissue used for DMEK surgery, the remainder of the tissue, other than the donor Descemet membrane and endothelium, is generally discarded.
There are suggestions that a single donor cornea can be used for two different patients by combining DMEK and deep anterior lamellar keratoplasty (DALK) procedures on the same surgery day [3]. However, DALK cases may not always be listed or required in another patient at the time of the DMEK case, and this practice is generally not routinely performed in the UK. Thus, for the majority of DMEK cases, following the preparation of the donor material, the remaining donor tissue (epithelium, Bowman’s and stroma) is discarded.
A further impact of reduced tissue availability is the effect on training of trainees and cornea fellows. This may subsequently have a detrimental impact on future corneal consultants struggling to get adequate surgical experience prior to starting their posts.
Simulation is routinely being incorporated into ophthalmology training to allow trainees to learn and develop their surgical skills in a safe environment. It has been shown that simulation can reduce the learning curve of difficult surgical techniques, accelerate the rate for trainees to achieve surgical competency, and treat patients safely and effectively [4,5,6]. These include virtual reality simulation, dry labs on artificial eyes and wet labs on animal specimens and human donor tissue. Most of these teaching techniques do not include corneal transplant surgery.
Virtual reality simulation is most commonly used for cataract surgery and is being extended into other ophthalmology subspecialties such as vitreoretinal simulation. These are particularly good at improving visual techniques such as continuous capsulorhexis, however there are currently no models available for corneal surgery.
Dry labs are also used in training with the plastic eyes. These are useful at developing corneal suturing techniques and hand positioning and they can be used to practise trauma repair. However, the model eye does not reflect the feel of a human cornea and they do not have the ability to operate on individual layers of the cornea, such as practising descemetorhexis technique and understanding planes of the tissue.
Wet labs are available which use both animal and human tissue. Human donor tissue to train on is available from NHS blood and transplant services. It is tissue that has not met the stringent criteria for use of transplants in patients (for example with an inadequate cell count). It provides realistic skills for preparation of both DALK and DMEK grafts [7], however it is expensive and therefore not carried out frequently, meaning one does not get the opportunity to continue to develop and refine these skills.
We present a teaching technique whereby the remainder of the corneal donor tissue not used for the DMEK surgery can be used for training purposes, without the use of any additional resources.

Figure 1: Kit used for DMEK preparation.
The technique
Following the preparation of the donor tissue for DMEK surgery, rather than discarding the remainder of the donor tissue, this tissue can be effectively used for providing training in theatre at the end of the list under consultant supervision. The instruments from the case are kept aside (Figure 1) and are used for the training to avoid having to use any further kit.
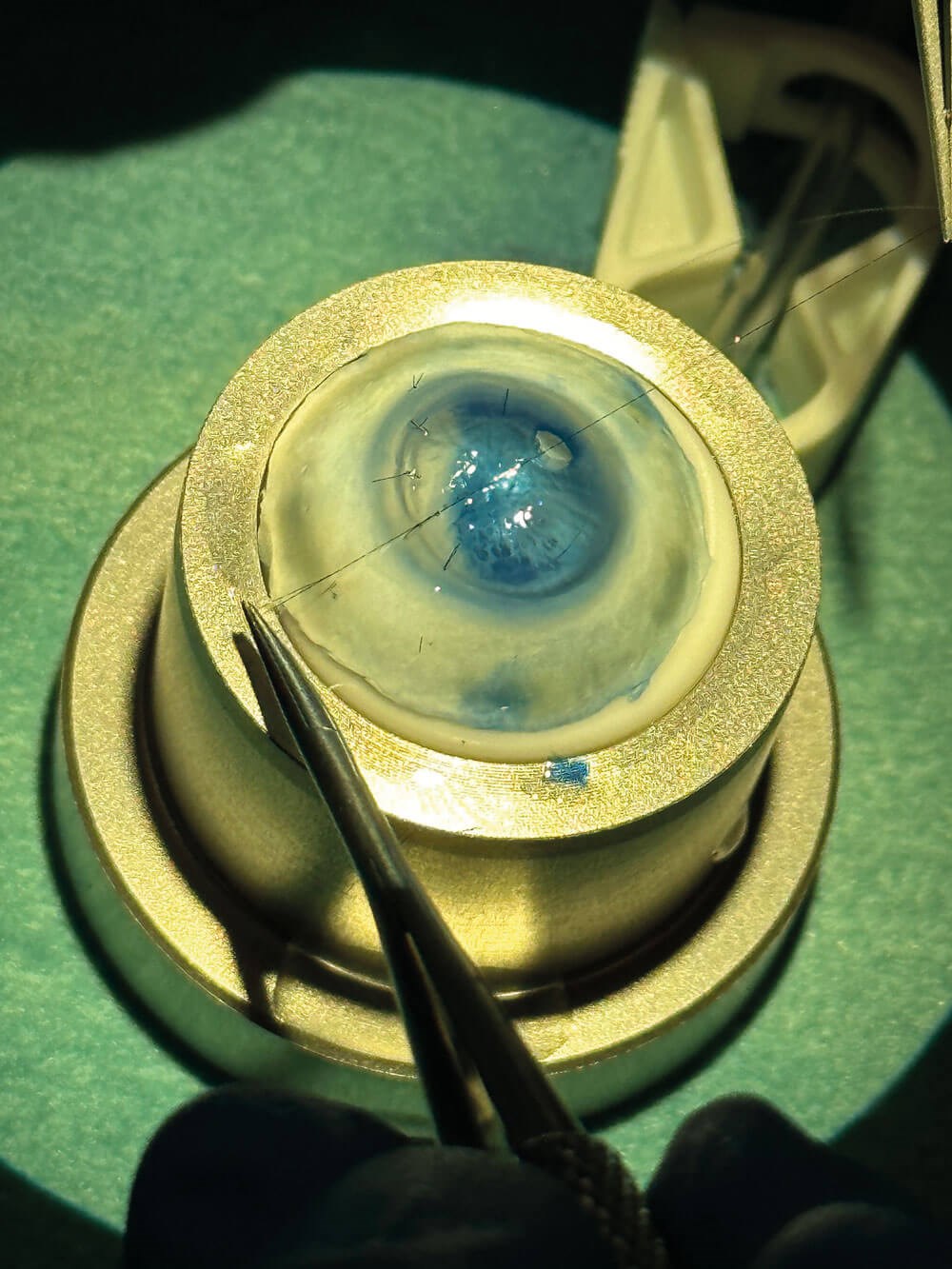
Figure 2: Surgical skills training using remainder of the DMEK preparation kit.
Trainees can enhance their corneal surgical skills in graft preparation and suturing on this remaining donor tissue. The skills include attaching the corneal button to the suction device (Figure 2); practising raising the edge of Descemet membrane to ensure the correct plane is achieved; and peeling the remaining Descemet membrane. The remaining edge of the tissue can be used to practise loading tissue into the loading device and injecting it.
A further use is to practise cornea suturing by placing the tissue on the device with the epithelium facing upwards. A simulated penetrating laceration can be created, and cornea suturing techniques can be practised to close up this wound. The other ‘clean’ end of the 10-0 nylon suture can be used, again avoiding the use of further kit.
Cornea suturing and repair of penetrating injury are an invaluable skill that many trainees may not have sufficient exposure to and this technique therefore provides a valuable teaching opportunity. Furthermore, since this is using actual human donor cornea material, the experience of tissue handling is as close to reality as can be achieved in a simulated setting.
Given the national shortage of donor cornea graft material and the impact this has on training, the teaching technique presented may provide trainees nationally an opportunity to develop cornea suturing and transplant skills, using tissue that would otherwise be discarded. This helps provide an invaluable training opportunity to aspiring cornea surgeons without using any additional resources or material, thus providing an effective and sustainable teaching strategy.
References
1. Gaum L, Reynolds I, Jones M, et al. Tissue and corneal donation and transplantation in the UK. Br J Anaesth 2012;108:i43–7.
2. Cornea Activity. Organ and Tissue Donation and Transplantation Activity Report 2022/23.
https://nhsbtdbe.blob.core.windows.net/
umbraco-assets-corp/30189/
section-10-cornea-activity.pdf
3. Cursiefen C, Heindl LM, Bachmann BO, Kruse FE. Split Donor Cornea Transplantation by Combined DMEK and DALK Surgeries: A New Strategy to Reduce Corneal Donor Shortage. Invest Ophthalmol Vis Sci 2010;51(13):1618.
4. Ferris JD, Donachie PH, Johnston RL, et al. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of EyeSi virtual reality training on complications rates of cataract surgery performed by first and second year trainees. Br J Ophthalmol 2020;104:324–9.
5. McCannel CA, Reed DC, Goldman DR. Ophthalmic surgery simulator training improves resident performance of capsulorhexes in the operating room. Ophthalmology 2013;120:2456–61.
6. Almaliotis D, Almpanidou S, Athanasopoulos GP, et al. The contribution of wet labs in the education of ophthalmologists. Ann Med Surg 2021;72:103034.
7. Parekh M, Ruzza A, Rovati M, et al. DMEK surgical training: An instructional guide on various wet-lab methods. Surv Ophthalmol 2023;68(6):1129–52.
[All links last accessed January 2024]
Declaration of competing Interests: None declared.
COMMENTS ARE WELCOME







