Ophthalmic viscoelastic devices (OVDs) are essential in many different stages of cataract surgery. This article discusses the categories of OVDs and their respective properties, and highlights their uses in different scenarios faced in cataract surgery.
Ophthalmic viscoelastic devices are gel-like substances that have become an essential part of any intraocular surgery [1]. The dual properties of OVDs allows them to behave similarly to both a solid and a fluid, though it can be dependent on the conditions during surgery [2]. From the beginning of cataract surgery to the end, OVDs can be used in all stages of the procedure, hence understanding the benefits, the properties and the application of these devices is paramount for any ophthalmic surgeon.
A brief history
Hyaluronate was initially discovered in 1934 by Karl Meyer and John Palmer, through isolating the molecule from the vitreous of cows [1]. Balazs subsequently developed the first sodium hyaluronate viscoelastic that was injected intraocularly in 1972 [2]. This development led to the first OVD that was later approved by the Food and Drug Administration in the US, under the brand Healon in 1983 [2]. Advancements within OVDs progressed rapidly in the 1990s and 2000s, and modern OVDs can now comprise of a various combination of constituents, such as sodium hyaluronate, chondroitin sulphate, and hydroxypropyl methylcellulose [2]. Safety and performance standards were implemented from 1995 to 2000 to guide approval requirements of OVDs [2]. Prior to the use of viscoelastic devices, complications were more prevalent, and thus the implementation of OVDs intraoperatively has undoubtedly improved surgical safety [1].
Ophthalmic viscoelastic devices today
In modern intraocular surgery, the roles of OVDs include stabilising the anterior chamber, protecting the corneal endothelium and reducing damage from shock or other forces that may occur during the procedure [1,3]. It is typically used before the formation of the capsulorhexis, to aid removal of epinucleus or cortex, and to inflate the capsular bag before insertion of the intraocular lens. Nowadays, there are three main classes of OVDs that are categorised based on their properties: cohesive, dispersive, and viscoadaptive [4].
Cohesive viscoelastic devices
Cohesive viscoelastic devices (CVDs) are generally high-viscosity substances, due to the higher molecular weight and longer chained molecules of its constituent parts [6]. It has a high surface tension, allowing it to act more similarly to a gel rather than a liquid, and thus it is easily aspirated [6]. Owing to these properties, CVDs are optimal for creating spaces within the eye, as well as maintaining pressure on structures where needed. Healon is considered a cohesive viscoelastic, and some other examples of include ProVisc and AmVisc [1].

ProVisc (Cohesive OVD).
Cohesive viscoelastics can stabilise the anterior chamber, which reduces the fluctuation of pressure. During the formation of the capsulorhexis, a stable pressure is particularly important, as a sudden change in pressure can result in an uncontrolled extension of the rhexis. For novice surgeons, there is sometimes the tendency to inadvertently press on the posterior lip of the main wound during capsulorhexis formation, which allows the CVD to extrude from the main wound. In these instances, it is prudent to re-instil more cohesive viscoelastic to maintain the pressure and minimise the risk of a complication early-on.
Given the ability for CVDs to create space, it is also typically used when inflating the capsular bag before the insertion of the intraocular lens or a capsular tension device. It can also be used in deepening a shallow anterior chamber.
In patients with small pupils despite instillation of mydriatics, CVDs can firstly help with enlarging the pupil due to its ability to apply pressure on the iris to widen the pupillary aperture. If the pupil is still not large enough despite the injection of a CVD, then the same viscoelastic can also be used to aid the insertion of a Malyugin ring or iris hooks. The OVD helps to create space between the iris and lens to fit the pupil expansion device and helps prevent accidental damage to the adjacent anterior lens capsule.
Dispersive viscoelastic devices
Dispersive viscoelastic devices (DVDs) generally have a lower viscosity, lower molecular weight, shorter molecular chain and are more fluid-like compared to CVDs [3,7]. As a result, the molecules do not adhere to one another compared to CVDs, which allows it to disperse better and to coat surfaces. However, this characteristic also means that it is more difficult to aspirate all the OVD, as it tends to fragment. This can increase the risk of viscoelastic retention if care is not taken to ensure complete removal.
Viscoat is an example of a commonly used dispersive viscoelastic and comprises of chondroitin sulphate and sodium hyaluronate [8]. Not only does the physical fluid-like properties aid Viscoat in coating ocular structures, but the negative electrical properties of this OVD also contributes to its adherence to the positively-charged intraocular structures [8]. Ocucoat and Endocoat are also examples of other types of dispersive viscoelastiscs [9].

Viscoat (Dispersive OVD).
Due to the strong ability of DVDs in coating surfaces, it is particularly effective in protecting the corneal endothelium, especially when it forms part of the outer layer of the soft-shell technique, pioneered by Arshinoff [7]. This technique aims to optimise the properties of both dispersive and cohesive OVDs. It involves first injecting a dispersive viscoelastic into the anterior chamber after the corneal incisions, followed by a second injection of a CVD underneath the DVD. This is to push the DVD closer to the posterior corneal surface and to coat it more evenly. Due to the lower molecular weight and the more fluid-like properties of DVDs, they are typically more difficult to aspirate and thus maintaining its protective effect to the corneal endothelium, which is particularly important during phacoemulsification and removal. The use of both types of viscoelastic devices allows for space to be created and the pressure to maintained within the anterior chamber, while maintaining corneal endothelium protection [7,9].
In certain types of difficult cataracts, such as posterior polar cataracts, dispersive viscoelastics can be used for viscodissection to provide additional control during the separation of an often tightly adherent cataract from the posterior capsule [10]. This is especially salient when hydrodissection and nucleus rotation are often contraindicated in the removal of posterior polar cataracts.
Dispersive viscoelastics are also useful during instances of complications within cataract surgery. In some cases of posterior capsular rupture, where the bag may still be partially intact, it is possible to tamponade the rupture with a DVD [11]. The instillation of the DVD should be done before the removal of the instrument providing irrigation to ensure a successful tamponade. By making use of an OVD with a good ability to coat the posterior capsule, this technique can prevent any unremoved lens fragments from falling into the posterior segment or any vitreous prolapse through the rupture [4,11].

Viscoadaptive viscoelastic devices
These are OVDs which can have different properties depending on the flow rate and pressure that the viscoelastic is subjected to. This can differ from different brands of viscoelastics. Healon 5 and MicroVisc are some examples of viscoadaptive OVDs [1].
For example, Healon 5 has an extremely high viscosity at rest, and acts similarly to a CVD at slow flow rates [5]. This renders it easily removed at lower flow rates, as OVDs tend to coalesce. At higher flow rates, it fragments more easily and is more difficult to be removed, which can provide some degree of protection to ocular structures, such as during phacoemulsification [1,5]. These OVDs have some of the benefits of both cohesive and dispersive viscoelastics, with better coating ability at higher flow rates as well as easier removal at low flow rates [1,5].

Healon V (Viscoadaptive OVD).
Despite this, there has been reports in the literature that suggest viscoadaptives can be still difficult to remove, especially after the intraocular lens has been placed [12]. Viscoadaptive OVDs can also vary between brands and makes and therefore will have different properties depending on the flow rate for which it has been designed. As a result, it is important for the surgeon to be cognisant of this to allow for an adjustment period when using a new viscoadaptive OVD.
Applications to your practice in cataract surgery
There is no doubt of the importance of using OVDs during cataract surgery, and their uses are numerous. However, knowing when and how to use the correct OVD is equally important, which highlights the necessity of having a good understanding of the basic properties of these devices.
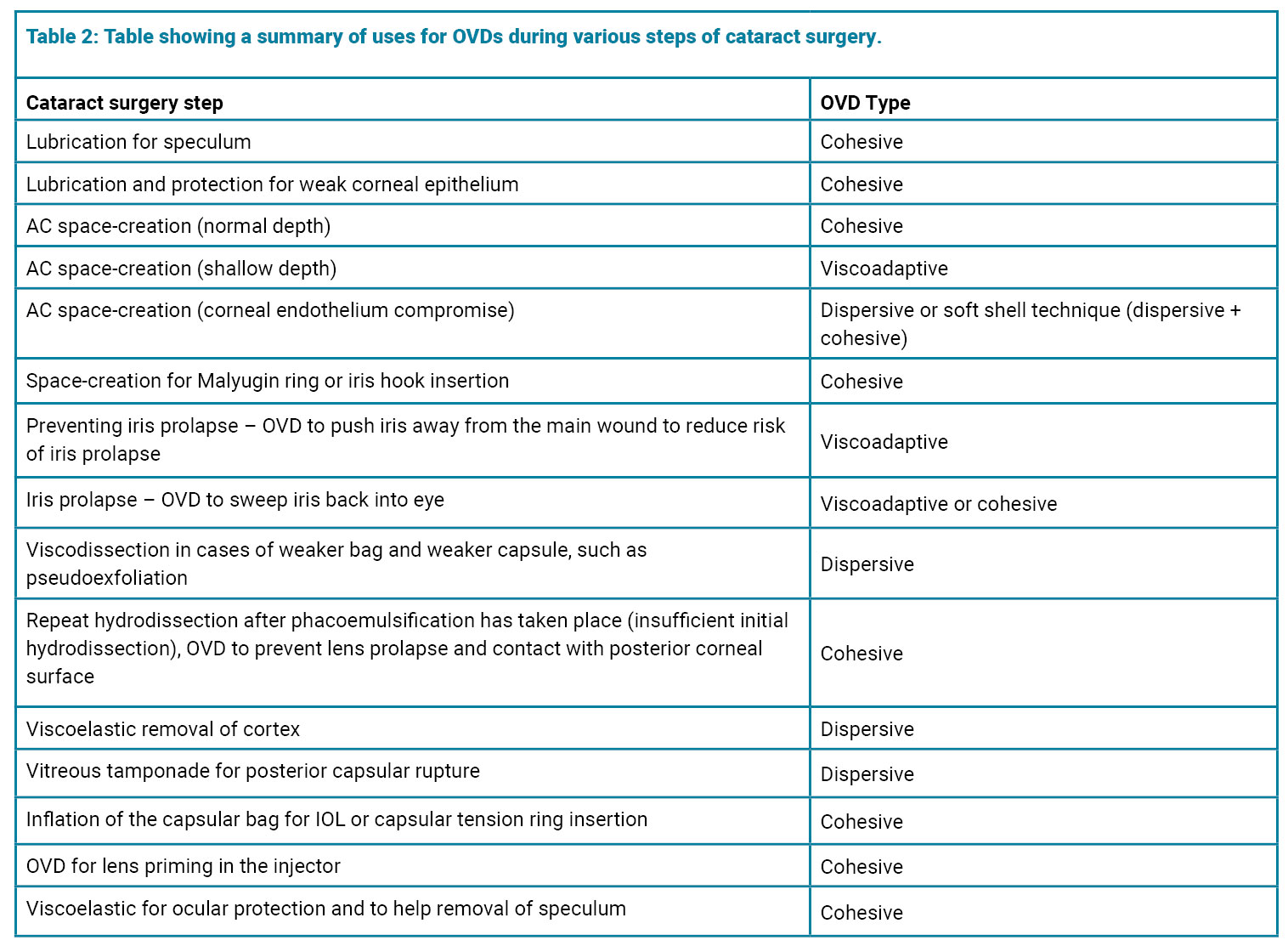
During my own theatre sessions, I examined different types of OVDs and their physical properties. The cohesiveness, viscosity and fragmentation of the different categories of OVDs are apparent even to the naked eye, which emphasises the difference in their characteristics. Although there is no perfect OVD, selecting the most appropriate OVD for particular steps of cataract surgery will naturally improve your surgical practice. The table below shows a summary of potential uses of OVDs during various stages of cataract surgery and complications.
Ultimately, the benefits of using OVDs are numerous, and innovations of these devices are continually changing. The applications of OVDs are increasing not just in cataract surgery, but also other subspecialties, such as anterior segment, glaucoma and vitreo-retinal surgery. Within cataract surgery, the preference of which OVD to use can vary from surgeon to surgeon, which can be elicited through trial and error. Having a better understanding of the properties of different ophthalmic viscoelastic devices will aid your overall decision-making during surgery, and help you become a better surgeon.
References
1. Borkenstein AF, Borkenstein EM, Malyugin B. Ophthalmic Viscoelastic Devices (OVDs) in Challenging Cases: a Review. Ophthalmol Ther 2021;10(4):831–43.
2. Scholtz SK, Auffarth GU. From Simple Liquids to Surgical Instruments: On the History of Ophthalmo-Viscoelastic Devices (OVD). Archiwum Historii i Filozofii Medycyny 2012:16–25.
3. Bissen-Miyajima H. Ophthalmic viscoelastic devices. Curr Op Ophthalmol 2008;19(1):50–4.
4. Kaur K, Gurnani B. Viscoelastics. StatPearls [Internet] 2023:
https://pubmed.ncbi.nlm.nih.gov/35201717/
[Link last accessed Dec 2024}
5. Higashide T, Sugiyama K. Use of viscoelastic substance in ophthalmic surgery — focus on sodium hyaluronate. Clin Ophthalmol 2008;2(1):21–30.
6. Storr-Paulsen A, Norregaard JC, Farik G, Tårnhøj J. The influence of viscoelastic substances on the corneal endothelial cell population during cataract surgery: a prospective study of cohesive and dispersive viscoelastics. Acta Ophthalmol Scand 2006;85(2):183–7.
7. Arshinoff SA. Dispersive-cohesive viscoelastic soft shell technique. J Cataract Refract Surg 1999;25(2):167–73.
8. Hsiao CW, Cheng H, Ghafouri R, et al. Corneal Outcomes Following Cataract Surgery Using Ophthalmic Viscoelastic Devices Composed of Chondroitin Sulfate-Hyaluronic Acid: A Systematic Review and Meta-Analysis. Clin Ophthalmology 2023;17:2083–96.
9. Yildirim TM, Auffarth GU, Son HS, et al. Dispersive viscoelastic devices demonstrate greater efficacy in protecting corneal endothelium in vitro. BMJ Open Ophthalmol 2019;4(1):e000227.
10. Siatiri H, Moghimi S. Posterior polar cataract: minimizing risk of posterior capsule rupture. Eye 2005;20(7):814–6.
11. Chakrabarti A, Nazm N. Posterior capsular rent: Prevention and management. Indian J Ophthalmol 2017;65(12):1359.
12. Oshika T, Bissen-Miyajima H, Fujita Y, et al. Prospective randomized comparison of DisCoVisc and Healon5 in phacoemulsification and intraocular lens implantation. Eye 2010;24(8):1376–81.
Declaration of competing interests: None declared.






