Giant cell arteritis (GCA) is an immune mediated granulomatous inflammatory disease that affects muscular middle or large sized arteries. It is considered as a continuation of polymyalgia rheumatica (PMR) when the severity of the disease has increased.
It is the most common of all the vasculitides. Common signs and symptoms include headaches, shoulder pain, fever and night sweats, jaw claudication, raised inflammatory markers, mild anaemia, temporal tenderness and blurred or double vision.
GCA and ophthalmology
Many ophthalmologists and emergency eye clinics are the first port of call for GCA suspects. This is due to the fact that the loss of vision in GCA is severe and irreversible. GCA has several ocular manifestations. These include:
Ischaemic optic neuropathy: this is the most severe form and can usually lead to permanent and severe loss of vision. This could be anterior (AAION) which is the more common type or posterior (PION) which is far less common.
Central retinal artery occlusion (CRAO): can happen in the context of GCA if the inflammatory process affects the central retinal artery and lead to severe loss of vision.
Ocular ischaemia syndrome (OIS): can happen if the inflammatory process affects the ophthalmic artery and can lead to retinal ischaemia, anterior chamber inflammation and neovascularisation.
Ocular motility abnormalities: such as cranial nerve (CN) palsies, most commonly VI CN palsy but also III and possibly IV cranial nerve palsies.
Other rare manifestations: such as scleritis.
Dilemmas in GCA diagnosis
GCA is a clinical diagnosis. The clinician can overrule any investigation result if the clinical suspicion is high. The problem with signs and symptoms of GCA and its diagnostic tests is that most of them are non-specific and can be positive in various conditions.
Headaches and GCA: if you ask almost any person if they have headaches, the answer almost certainly is yes. It is the character of the headache that can point the clinical towards GCA type headaches or common migraine and tension headaches.
Raised inflammatory markers and GCA: raised erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can happen in any inflammatory, infectious or malignant condition. It is important to ask patients if they have any infection anywhere in their body such as urinary infections, respiratory infections, sinusitis, diabetic ulcers, etc.
Jaw claudication and GCA: it is important to ask specific and clear questions when investigating GCA. Jaw claudication is not jaw pain such as the one noted in temporomandibular joint (TMJ) problems.
Swollen optic nerve and GCA: it is important to assess the appearance of the swollen optic nerve, the prodromal symptoms prior to the loss of vision, the current visual functions and the status of the other optic nerve (crowded, disc-at-risk or not). This can usually help differentiate non arteritic anterior ischaemic optic neuropathy (NAION) from AAION.
CRAO and GCA: if a thrombus is seen in the context of CRAO then it is not GCA related. It is extremely rare for GCA to cause branch RAO as such arteries are not middle size muscular arteries.
Case studies
Case 1:
A 70-year-old patient was referred to the eye emergency clinic with sudden onset loss of vision in his left eye. He did not have any headaches or temporal tenderness. His vision in the affected eye was reduced to hand movements only. Fundus examination showed CRAO with mildly swollen optic nerve. His inflammatory markers were mildly raised (ESR: 26, CRP 25) so colleagues at the eye emergency clinic suspected that he has GCA and he was started on steroids.
If you look carefully to his fundus photo below, it clearly shows multiple emboli suggesting that his CRAO is not GCA related and his raised ESR and CRP are due to a different cause.

Figure 1: Left CRAO with multiple emboli suggesting that it is not GCA related.
Case 2:
A 55-year-old man was seen in eye emergency clinic having been transferred from another hospital complaining of two weeks blurred vision in both eyes (left > right). His vision was 0.0 LogMAR (6/6 Snellen) in the right and 0.4 LogMAR (6/15 Snellen) in the left. He had reduced colour vision both eyes and constricted field defect left eye on confrontation. There was no relative afferent pupillary defect (RAPD) reported. Aside from small crowded discs, the rest of the ocular examination was unremarkable.
His past medical history was significant and complex, with known metastatic renal cell carcinoma (on long-term oral dexamethasone) with known metastatic lesions in his bones. An MRI scan was requested and was reported by the neuroradiologist as normal.
His inflammatory markers were raised on admission CRP 114, ESR 47, however, he had a normal white cells blood count and platelets but no obvious source of infection. These inflammatory markers have significantly reduced following a dose of Tazocin. He denies any GCA symptoms and no tenderness on palpation of temporal arteries.
His ophthalmic history includes a left-sided NAION in 2012 with a residual visual field loss. The main concern in this patient was whether there is an arteritic element to his complaint that was masked by his chronic steroid use.
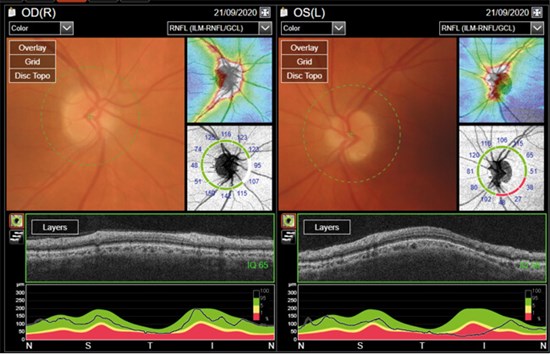
Figure 2: The patient showed no obvious optic nerve swelling.
This is a complex situation, however, there is no obvious optic nerve swelling (Figure 2) and no transient visual obscurations. The reduced vision in the left eye could be explained by the previous NAION. There are no signs of GCA at the moment and the raised inflammatory markers are likely to be malignancy related with possible underlying infection process as they responded well to Tazocin.
Conclusion
GCA is a serious and potentially blinding condition. It is important to suspect and treat in all relevant circumstances but it equally important to remember that all the above signs and symptoms are nonspecific and can happen in a multitude of conditions. This is important to avoid over treatment with high doses of steroids with all the possible side-effects and complications that come with such treatment. Good, detailed history and attention to detail is key, and assessing the level of suspicion before committing to treatment is very important in order to avoid over treatment or missing a diagnosis with subsequent loss of vision.
Close relationship with rheumatology colleagues with a clear and urgent referral pathway is very important in managing these complex cases safely.
References
1. Mackie SL, Dejaco C, Appenzeller S, et al. British Society for Rheumatology guideline on diagnosis and treatment of giant cell arteritis. Rheumatology 2020;59(3):e1-e23.
2. Miller NR, Arnold AC. Current concepts in the diagnosis, pathogenesis and management of nonarteritic anterior ischaemic optic neuropathy. Eye (Lond) 2015;29(1):65‑79.
3. El-Dairi MA, Chang L, Proia AD, et al. Diagnostic algorithm for patients with suspected giant cell arteritis. J Neuroophthalmol 2015;35(3):246-53.
4. Hayreh SS, Podhajsky PA, Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol 1998;125(4):509-20.
5. Hayreh SS, Podhajsky PA, Raman R, Zimmerman B. Giant cell arteritis: validity and reliability of various diagnostic criteria. Am J Ophthalmol 1997;123(3):285-96.
6. Baig IF, Pascoe AR, Kini A, Lee AG. Giant cell arteritis: early diagnosis is key. Eye Brain 2019;11:1-12.
7. Rana AQ, Saeed U, Khan OA, et al. Giant cell arteritis or tension-type headache?: A differential diagnostic dilemma. J Neurosci Rural Pract 2014;5(4):409-11.
8. Ing EB, Miller NR, Nguyen A, Su W, et al. Neural network and logistic regression diagnostic prediction models for giant cell arteritis: development and validation. Clin Ophthalmol 2019;13:421-30.
COMMENTS ARE WELCOME





