Introduction
In this article I will try to summarise some of the definitions, tests and assessments performed in the strabismus clinic to assess patient binocular potential. This is a key feature of strabismus assessment, especially in adults, and it will significantly guide and influence the management options and plans.
Definition of BSV [1]
Binocular single vision is the patient’s ability to use both eyes simultaneously to achieve a single image perception. It involves the simultaneous perception of the two images, one from each fovea (bifoveal) and the absence of any manifest deviation. It can be classified to three grades according to Worth’s classification:
- Simultaneous perception
- Fusion
- Stereopsis.
Grades of BSV [1]
a. Simultaneous perception: the ability to see an image from each eye at the same time.
b. Fusion:
i. Sensory fusion is the ability to interpret the two similar images as one.
ii. Motor fusion is the ability to maintain the single image during the divergence and convergence movements. This is measured by the fusional ranges.
c. Stereopsis: is the perception of depth of objects due to fusing images that stimulate disparate retinal elements.
Loss of fusion [1,2]
This can occur usually following severe head trauma or brain damage. The loss of fusion will lead to diplopia in all positions of gaze without the ability to fuse the images with prisms or on the synoptophore.
It is important to differentiate true loss of fusion from apparent loss which can happen due to several other causes, such as a significant torsional element to the deviation, aniseikonia due to refractive, lens or macular changes, significant anisometropia, image distortion due to macular disease and complete bitemporal hemianopia. Loss of fusion has also been described following unilateral aphakia, but hasn’t been described following pseudophakia.
Fusion can also be lost following a long period of loss of BSV for any reason.
What is “suppression”? [3]
This is defined as a cortical function to remove the awareness of the unwanted visual stimulus. Physiological suppression can be seen in the elimination of physiological diplopia while pathological suppression happens in manifest strabismus and in some latent strabismus patients and some amblyopia patients.
The suppression is a cortical mechanism that develops in response to any of these symptoms:
- Binocular diplopia: in manifest strabismus, the image falls on non-corresponding retinal elements in the fixing and non-fixing eyes.
- Confusion: this is usually a rare symptom that happens due to the fact that in manifest strabismus, the fovea of the fixing eye sees a different image to the one seen by the fovea of the non-fixing eye.
- Incompatible images: due to anisometropia or aniseikonia, where the images on the foveae are of different sizes or shapes. These patients usually have central suppression but can maintain peripheral fusion.
It usually develops early in childhood and very rarely in adults. Suppression can affect one or both eyes and can be intermittent depending on the size and the type of the deviation. It also varies in the size of the suppression zone and its density.
When suppression is detected, it is important to rule out postoperative diplopia risk prior to any surgical intervention. This can be done by assessment and mapping of the suppression scotoma using prisms (going with 20 prism diopters under and over corrections of the deviation angle). If the prism assessment detected the possibility of postoperative diplopia, botulinum toxin can be used to correct the deviation to assess the risk for diplopia in real life.
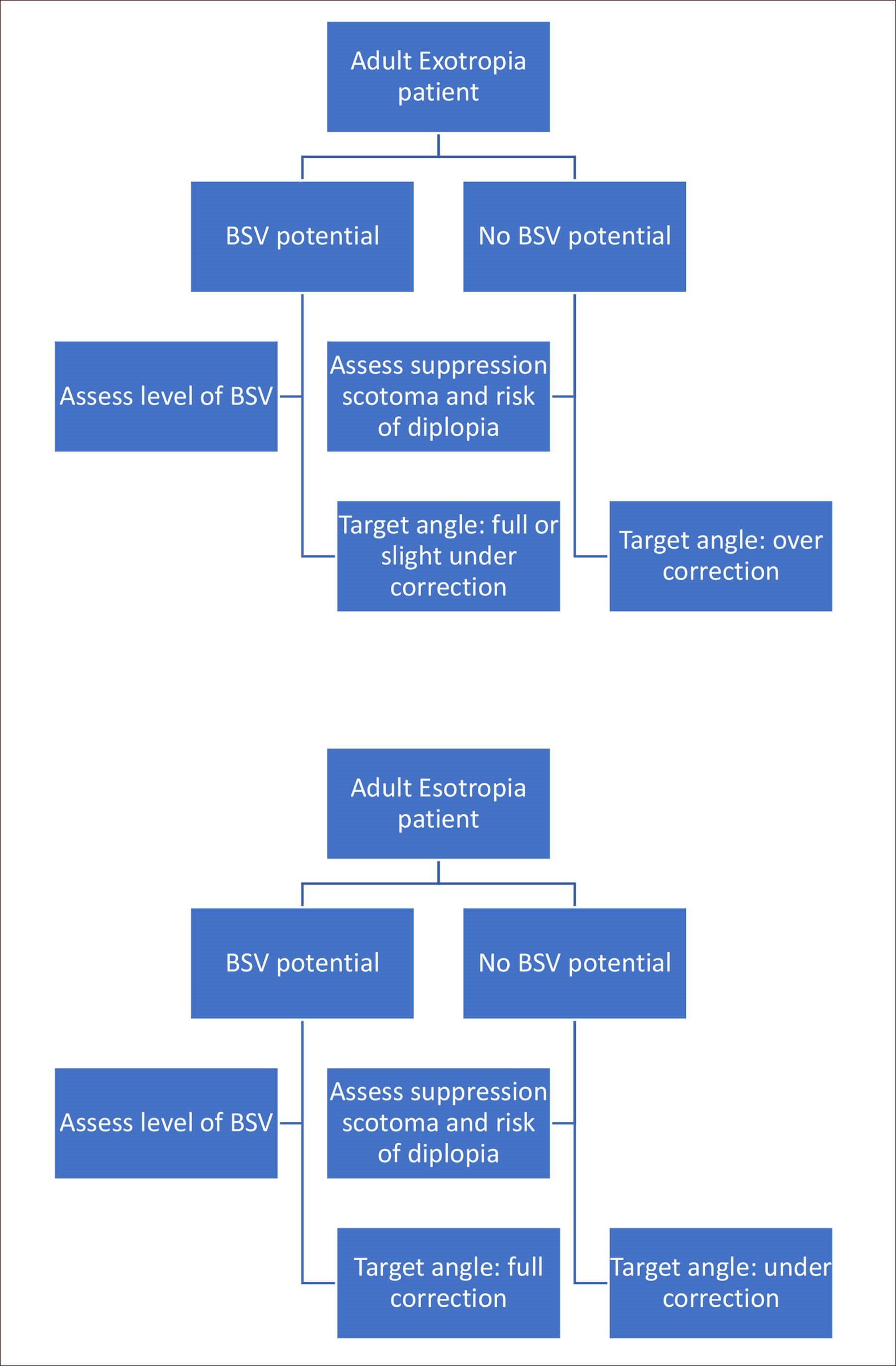
Schematic representation of the influence of BSV on surgical
planning for a manifest strabismus patient.
Investigations to assess BSV [1,3]
It is important in the management of strabismus to investigate the presence or absence of BSV and its grade or in its absence, the presence of suppression zone, its size and density. This is important as it will help understand the aim of any intervention whether it is to achieve / restore BSV or only to improve patients’ appearance.
History: the age of onset on the deviation, the size of the angle and the duration of the manifest strabismus can help predict the presence of BSV and its stability.
Refractive errors: especially the presence of anisometropia.
Visual acuity: doesn’t always help prediction of the presence or absence of BSV. Many patients with amblyopia can have useful BSV although stereopsis might be reduced.
Abnormal head posture: this is usually a response mechanism to help with diplopia and achieve BSV.
Orthoptic assessment: the presence of a latent deviation and some recovery can indicate some control and presence of BSV.
Presence of diplopia: especially with the ability to control it would suggest the presence of BSV.
Type of strabismus: early esotropia patients tend to have poor or absent BSV while exotropia patients would have good BSV potential.
Tests for assessment of BSV [1]
- Bagolini glasses:
a. Pair of plano glasses with striation at 45 degrees in one and 135 degrees in the other.
b. Assess simultaneous perception, sensory fusion or suppression.
c. Minimally dissociating. d. Possible results:
i. Two lines crossing at the spotlight: BSV.
ii. Two lines crossing but not on the spotlight or not crossing: manifest deviation with diplopia.
iii. Missing centre of one line: central suppression.
iv. Missing one line: suppression. - Worth lights:
a. Set of four lights: two green, one red and one white viewed via red (right eye) – green (left eye) goggles.
b. Assess simultaneous perception, sensory fusion or suppression.
c. The red light is seen via the red filter, the green lights are seen via the green filter and the white light is seen via both filters.
d. Possible results:
i. Five lights seen: manifest deviation without suppression.
ii. Four lights seen: BSV.
iii. Three lights seen: right suppression.
iv. Two lights seen: left suppression. - Polaroid four dot test:
a. Assess bifoveal fusion or central suppression at 6m distance.
b. Set of four polarised lights viewed using polarising glasses (two seen with the left eye and three seen with the right eye).
c. Possible results:
i. Five lights seen: diplopia (can happen at closed distance).
ii. Four lights seen: bifoveal fusion.
iii. Three lights seen: left suppression.
iv. Two lights seen: right suppression. - Prism reflex test:
a. Assess the presence of motor fusion and BSV.
b. Fifteen or 20 base out prism diopter is used.
c. Introduction of the base out prism in front of one eye with result in the following movements:
i. The prism will shift the image to the temporal retina causing a corrective inward movement to regain foveal fixation.
ii. Hering’s law will cause an outward movement of the other eye causing diplopia.
iii. This will stimulate convergence and an inward movement of the other eye to regain fusion and resolve diplopia.
d. Removal of the prism will induce reversed compensatory movements to restore BSV.
e. Possible results:
i. All three movements are seen: motor fusion.
ii. Failure to adduct either eye: absence or weak motor fusion. - The four-diopter prism test:
a. Assess bifoveal fusion and presence of normal BSV.
b. Same principles of movement of the previous test but with a four diopter prism.
c. Base out prism is used in suspected micro esotropia and base in prism in suspected micro exotropia.
d. Possible results:
i. All three movements are seen: bifoveal fusion.
ii. No movement behind the prism or no corrective fusion movement: central suppression. - Prism fusion range:
a. Assessment of motor fusion.
b. The ability to maintain BSV with the introduction of base out and in prisms for horizontal vergence and base up and down for vertical vergence.
c. The positive amplitude is measured using base out prisms and negative amplitude is measured with the base in prisms.
d. Normal results:
i. Distance: 15 BO to 6-10 BI.
ii. Near: 35-40 BO to 10-15 BI.
iii. Vertical: 2-3 BU to 2-3 BD. - Synoptophore (major amblyoscope):
a. Assessment of all grades of BSV.
b. Dissociative and artificial environment to assess BSV.
c. Simultaneous perception can be found once superimposition of images is confirmed.
d. Fusion is assessed by moving the tubes while maintaining single image.
e. Torsion can be assessed and measured.
f. In a manifest deviation it is possible to selectively correct various elements of the deviation to guide management plans. - Controlled binocular acuity (CBA):
a. Assessment of control of deviation under accommodative duress.
b. Ensure that the control of exodeviation is not done by manipulating accommodation.
c. Ensure that the relative vergence amplitudes are sufficient for the patient.
d. Best achieved binocular vision while maintaining control of ocular alignment:
i. End point: patient becomes manifest or reports blur or diplopia. - Sbisa bar:
a. Assess the density of suppression or strength of BSV.
b. Seventeen filters from pale pink to dark red presented in front of the fixing or dominant eye.i. Increase the strength of the filter until diplopia is reported or patient becomes manifest.
c. It is used to assess the risk of intractable diplopia if treatment to eliminate suppression is considered.
d. Possible results:
i. Diplopia: fusion is disrupted if the patient has BSV and the density of the filter is a measure of the strength of the BSV.
ii. Diplopia: suppression is disrupted if the patient doesn’t have BSV. The density of the filter is a measure of the density of the suppression.
iii. The light change from red to white suggesting change of fixation and the eye behind the filter is suppressed.
Test for stereopsis [1-3]
Stereopsis is appreciation of relative depth of objects. It is measured by the minimum binocular disparity needed to appreciate depth and stereopsis and recorded in seconds of arc. There are many different tests which have different normal results and some of these tests have monocular clues to aid stereopsis rather than true stereopsis.
- Lang’s two-pencil test:
a. Basic test using two pencils and a cover.
b. Compares responses with both eyes open and when one is covered.
c. Possible results: locating the examiner pencil is better with both eyes open – stereopsis and BSV present while if the responses are similar with one eye covered, likely the deviating eye is suppressed. - TNO test:
a. Random dot stereograms and ref – green glasses.
b. Plates I – II – III to establish if stereopsis is present.
c. Plate IV to test for suppression.
d. Plates V – VI – VII measures stereoacuity from 480 – 15 seconds of arc.
e. No monocular clues.
f. Range from 1980 (screening plates) to 15 seconds of arc. - Wirt test:
a. Images seen by one eye are polarised 90 degrees to the one seen by the other eye.
b. Tested using polarised glasses.
c. Has monocular clues.
d. Range from 3000 for the fly to 40 seconds of arc for the circles. - Randot test:
a. Similar to Wirt test but also have random dots.
b. No monocular clues.
c. Range from 500 to 20 seconds of arc. - Frisby stereoacuity test:
a. Test for near.
b. Three clear plastic plates of different thickness with random shapes printed.
c. Each plate will have four squares of curved random shapes.
d. One square will have a hidden circle printed on the opposite surface. e. Range from 600 to 20 seconds of arc. - Lang stereoacuity test:
a. A combination of random dots and vertical elements.
b. Has two versions: Lang I (1200-550 seconds of arc) and Lang II (600-200 seconds of arc).
c. Used for screening purposes with only three pictures. - Synoptophore (major amblyoscope):
a. Helps determine the potential for BSV if the manifest deviation is corrected.
b. Can assess all elements of strabismus.
c. Can assess all levels of BSV and Braddick slides can assess stereopsis. - Prism adaptation test:
a. Also assess the potential for BSV.
b. Usually used for acquired esotropias.
c. Fully correct the deviation (needs good visual acuity and angle less than 40 prism diopters) and reassess a week later.
d. Possible results:
i. Still straight with BSV potential.
ii. Residual microtropia with possible BSV.
iii. Reconverge to the original angle (eat up the prism) suggests abnormal retinal correspondence.
iv. Reconverge suggestive of suppression.
e. Helps in surgical planning:
i. If there is BSV potential: multiple assessments until a stable angle is found, then maximal angle corrected surgically.
ii. If no BSV potential: surgical correction to the first angle measured. - Botulinum toxin:
a. Can be used to assess potential for BSV prior to surgery.
b. Possible indications:
i. Incomitant strabismus.
ii. Postoperative diplopia risk.
iii. Large angle deviations.
Tests for retinal correspondence (RC) [2,3]
If the objective and subjective angles of deviation measured on the synoptophore are equal, then normal retinal correspondence (NRC) is assumed. If, however, there is a large difference then abnormal retinal correspondence (ARC) should be considered.
The tests used can be based on either of the following principles:
- Assessment of relationship between the fovea of the fixing eye and the retinal area stimulated of the deviating eye.
a. Bagolini glasses.
b. Red filter test: red filter lens in front of the fixing eye and a white light source in front of the other one:
i. Possible outcomes:
1. Two lights: diplopia which could be crossed or uncrossed and NRC if the angle is between the images is similar to the deviation angle.
2. Two lights but the angle is different: diplopia with ARC.3. One light (pink) in the presence of a manifest deviation: ARC.
c. Synoptophore measuring the objective and subjective angles.
d. Worth’s four-dot test (seeing four dots in the presence of a manifest deviation) - Assessment of the visual directions of the two foveae:
a. After image test (Hering Bielschowsky):
i. Using a flash apparatus.
ii. A horizontal bright line is shown to the fixing eye and a vertical one for the other eye.
iii. Patient is asked to describe the after images (should see two lines with a central gap).
iv. Possible results:
1. A cross with coinciding gaps in the centre: NRC.
2. Displaced lights: ARC.
3. Single light: suppression.
b. Cuppers binocular test (foveo-foveal test of Cuppers):
i. Determines whether the foveae have common or different visual directions.
ii. Quantitative analysis of the angle of anomaly.
iii. Patient fixates on the central light of a Maddox scale via a plano mirror.
iv. The visuoscope asterisk is projected by the examiner onto the fovea of the deviating eye.v. The figure on Maddox scale measures the angle of anomaly.
Conclusion
Assessment of adult strabismus patient is a complex process that requires a multidisciplinary approach with the help of our orthoptist colleagues. Detailed history, refraction, orthoptic and ophthalmic examinations are crucial in the assessment of the patient and planning the management options.
Assessment of patient binocular potential is a very important element and will have significant implications on the management plans as well as the long-term prognosis following surgical intervention.
References
1. Ansons AM, Davis H. Diagnosis and management of ocular motility disorders. New Jersey, USA; Wiley Blackwell; 2014:144-69.
2. Stidwill D, Fletcher R. Normal Binocular Vision: Theory, Investigation and Practical Aspects. New Jersey, USA; Wiley Blackwell; 2010:38-71.
3. Bhola R. Binocular Vision. EyeRounds.org. 2006
http://eyerounds.org/tutorials/
Bhola-BinocularVision.htm
Last accessed February 2023.
COMMENTS ARE WELCOME






