History
-
An 80-year-old male had a cataract removed with intraocular lens (IOL) seven years previous. He presented with cloudy vision and it was noted that the IOL was intrinsically opaque. The IOL was replaced and sent for ophthalmic pathology assessment.
-
Figure 1 shows a section of lens under standard light microscopic conditions. The arrows point to the pathology.
-
Figure 2 is a Von Kossa stain.
-
Figure 3 is an Alizarin Red stain.
-
Figure 4 is a transmission electron microscope image of the pathology.
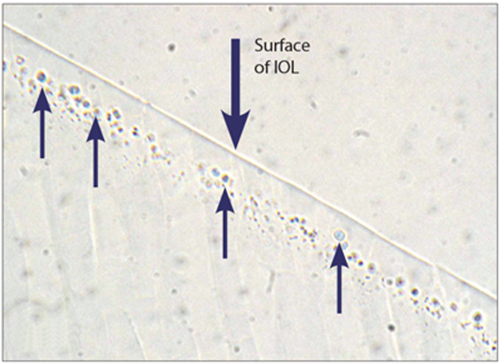
Figure 1.
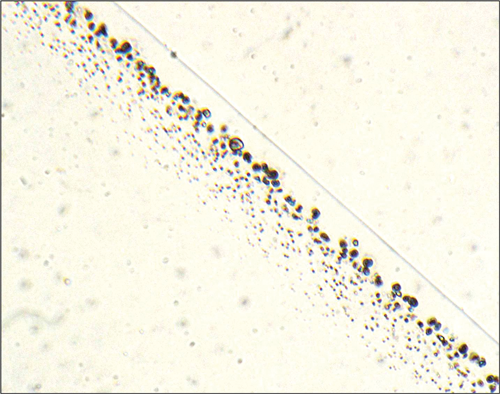
Figure 2.
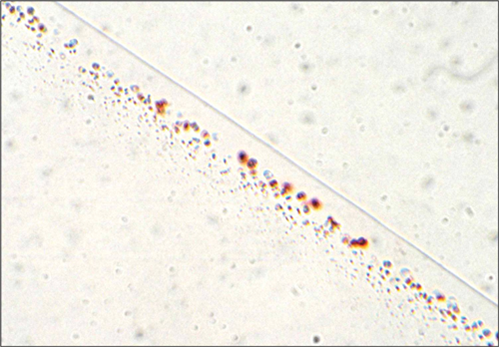
Figure 3.

Figure 4.
Questions
-
Which question was asked first of the ophthalmologist?
-
How was the specimen processed?
-
What is the nature of the pathology shown in Figures 2, 3 and 4?
-
What is the cause of the IOL opacity in this case?
-
How would you classify the causes of IOL opacification?
Answers
1. Which type of IOL it was. In this case, it was a MA60AC IOL (Alcon).
2. The specimen was processed in a conventional manner to paraffin wax and conventional sections cut on a microtome.
3. Figure 1 gives the impression of a sub-surface band of ‘cysts’ (blue arrows) within the optic. These ‘cysts’ are not cysts but comprise phosphate (Von Kossa Figure 2) and calcium (Alizarin red Figure 3).
4. The cause of the opacification is the deposition of calcium phosphate containing hydroxyapatite crystals within the IOL material – this is beautifully seen in Figure 4 (transmission electron microscopic image), which shows a spoke-like configuration of needle type crystals, centred around altered IOL material. No crystals were found in the haptics.
5. The causes of IOL opacification can be found in an excellent review: ‘Post cataract-IOL surgery opacifcation’ (Trivedi RH, et al. Eye 2002;16:217-41). In this review the authors provide the following classification scheme:
1. (A) Anterior capsule opacification (ACO), (B) Silicone oil adherence to IOLs.
(2) On (surface changes on the optical component of IOLs). Calcification on the surface of the Bausch & Lomb Hydroview® IOL.
(3) Within (alteration inside the IOL optic);
(A) Degeneration of ultraviolet absorber material and calcium deposits within the optic of a hydrophilic IOL (manufactured by Medical Developmental Research)
(B) Glistening of the AcrySof® IOL
(C) ‘Snowflake’ or ‘crystalline’ alteration of poly(methyl methacrylate) (PMMA) IOL optic: a syndrome caused by an unexpected late biodegradation of PMMA.
(4) Between (opacification between ‘piggyback’ IOLs). Interlenticular opacification (ILO) of ‘piggyback’ IOLs.
(5) Behind (posterior). Posterior capsule opacification (PCO).
COMMENTS ARE WELCOME





