History
-
A 69-year-old female patient was referred to the uveitis clinic from her local district general hospital with a left posterior uveitis which had been unresponsive to high dose steroids.
-
She had no other previous ophthalmic history nor significant systems review. Her past medical history included hypertension which was controlled by medication.
-
On examination, her corrected visual acuity was 6/12 in the right and hand movements in the left eye. Cornea and anterior segment were clear in both eyes, intraocular pressures were normal, early cataracts, there were no vitreous cells in the right but 3+ vitreous cells in the left eye, both retinae were flat and there were no evident chorioretinal lesions.
-
Work-up and baseline investigations for posterior uveitis were undertaken. The patient was seen again in two weeks. All bloods and anterior chamber tap were negative. The patient’s vision dropped to counting fingers in the right and perception light in the left eye. Fundoscopy revealed bilateral vitreous activity and creamy ill-defined choroidal lesions (Figure 1, black arrows). The patient was referred to the ocular oncology service and left transretinal and vitreal biopsies were sent for ophthalmic pathology assessment.
-
Macroscopic examination revealed: clear, colourless vitreous fluid (1ml undiluted and 4mls diluted); and 2.5mls clear, colourless subretinal fluid.
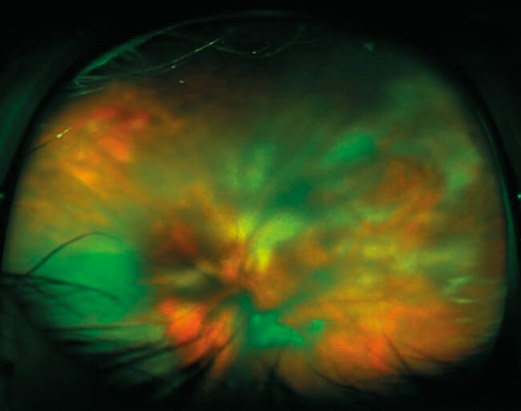
Figure 1.
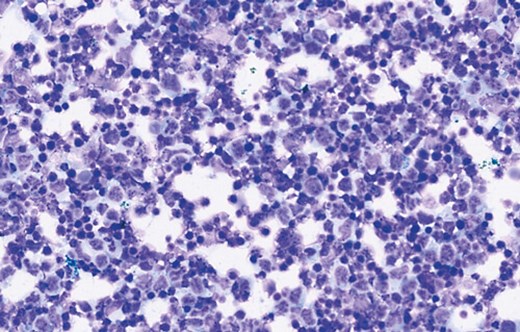
Figure 2.
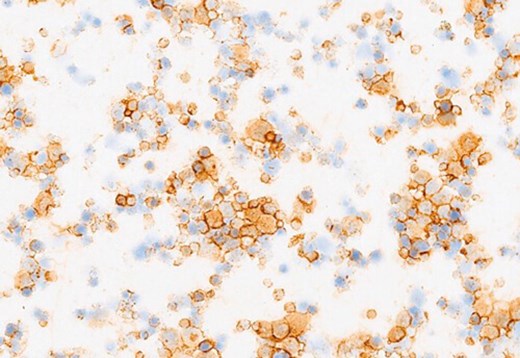
Figure 3a: CD20.
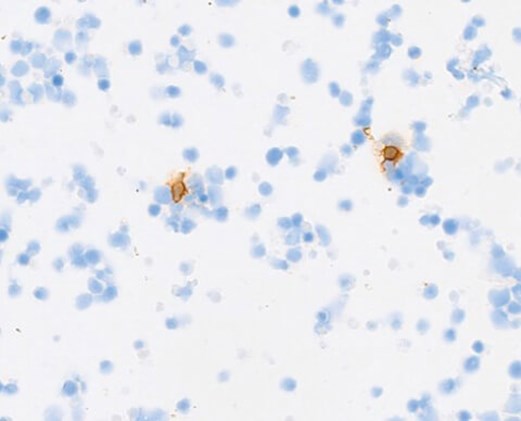
Figure 3b: CD3.
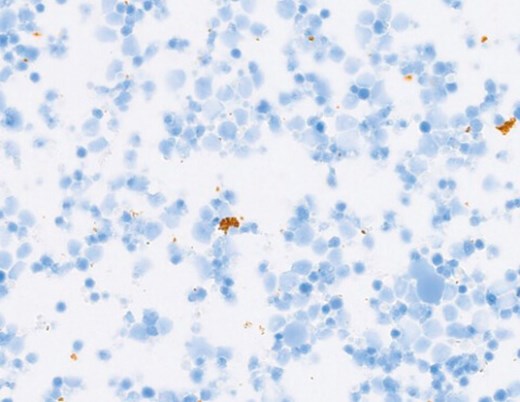
Figure 3c: CD68.
Questions
-
Figure 2 shows a representative May-Grünwald Giemsa (MGG) cytospin of the lesions. How can this be described?
-
What immunohistochemical stains would help?
-
Figures 3a-c demonstrate positive immunostaining for select markers. What is the most likely diagnosis?
Answers
1. The cytospin shows numerous blasts (black arrows) with large atypical nuclei and prominent nucleoli on a lytic background. The appearances are consistent with a high-grade lymphoma. Note: scattered background pigment can be seen as the lymphoma cells disrupt the overlying retinal pigment epithelium (RPE).
2. Immunohistochemistry to confirm lymphoma would include: CD20 (B-cell marker) and CD3 (T-cell markers). CD68 (macrophage marker) to help delineate the subtype of large cells.
3. Representative panels show the neoplastic B-lymphocytes (blasts) staining positively for CD20. There are very occasional reactive T-cells (CD3+) and macrophages (CD68+) seen in the background. The histomorphologic and immunohistochemical features are those of a DIFFUSE LARGE B-CELL LYMPHOMA. Furthermore, immunoglobulin heavy chain (IGH) and immunoglobulin kappa light chain (IGK) gene analysis by polymerase chain reaction (PCR) revealed a monoclonal B-cell population. Approximately 70% of vitreoretinal lymphomas are reported to harbour a MYD88 mutation. Although this was not undertaken in this case, it is increasingly being performed in diagnostic labs (Bonzheim I, et al. High frequency of MYD88 mutations in vitreoretinal B-cell lymphoma: a valuable tool to improve diagnostic yield of vitreous aspirates. Blood 2015;126:76-9). The patient was referred to the haemato-oncology team and received three courses of bilateral intravitreal methotrexate injections. Chorioretinal atrophy was noted, with no new / active chorioretinal lesions, at the last follow-up.
COMMENTS ARE WELCOME




