Acute macular neuroretinopathy (AMN) is a rare condition that typically affects young women and presents with photopsia and paracentral scotomata [1]. We describe a case of severe acute macular neuroretinopathy, following Covid-19 infection.
A 30-year-old woman presented to the urgent eye clinic with a one-day history of ‘black spots’ that started in her left eye and then involved her right eye, a day following Covid-19 infection. She described the spots as “static” and being able to “see through the dots” through her right eye, but “minimally” through her left eye.
Her past medical history was notable for small bowel Crohn’s disease, for which she was on regular adalimumab and a reducing regime of azathioprine. She had a history of raised cholesterol and regular combined oral contraceptive pill use, which she had been well established on. She was a non-smoker, with no history of hypertension.
Her ophthalmological history was notable for left eye amblyopia.
On examination, her best corrected visual acuity was 6/6 in her right eye and 6/37 (in keeping with known amblyopia) in her left eye. Intraocular pressures were 17mmHg and 16mmHg in the right and left eyes respectively. She had evidence of full ocular movements, with no anterior segment abnormalities.
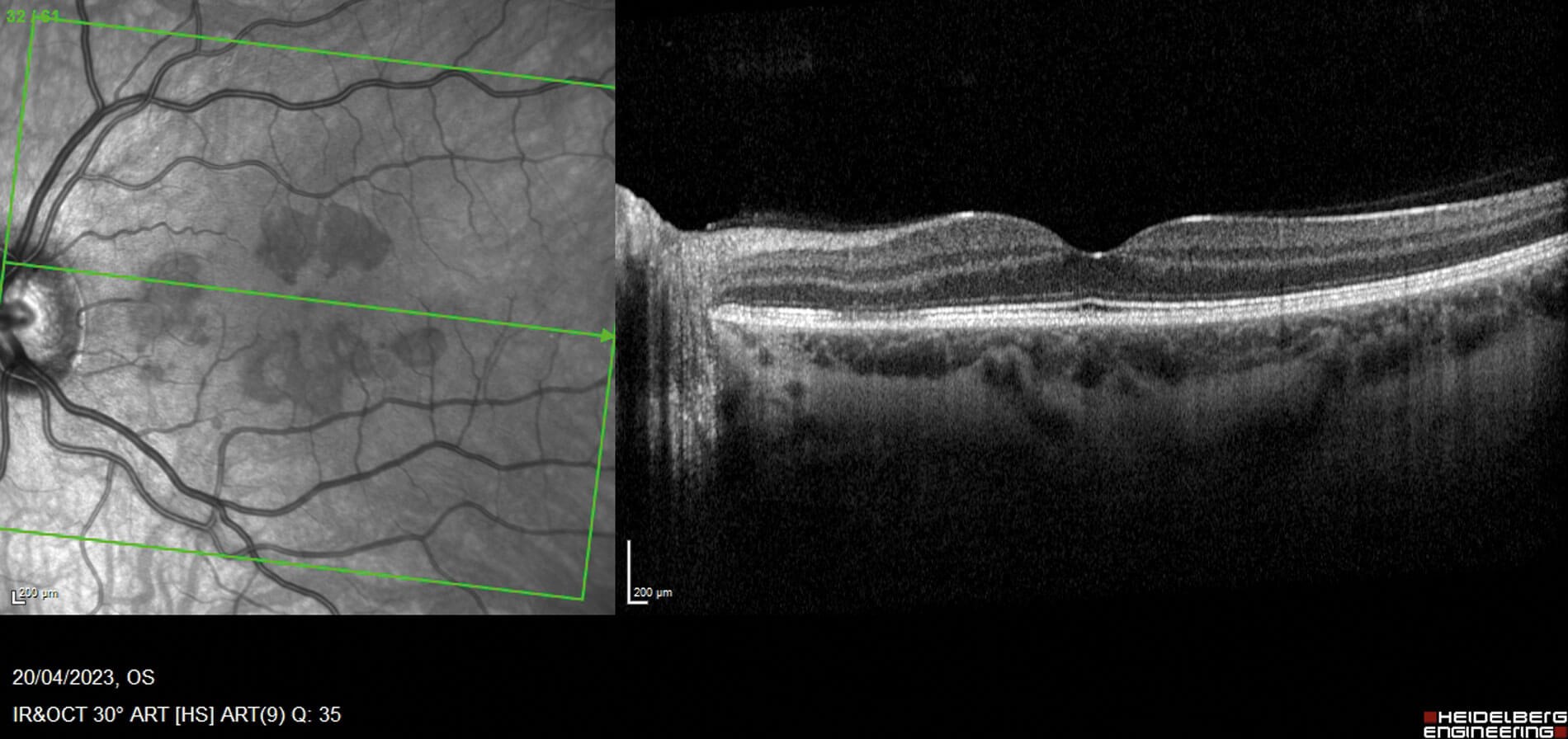
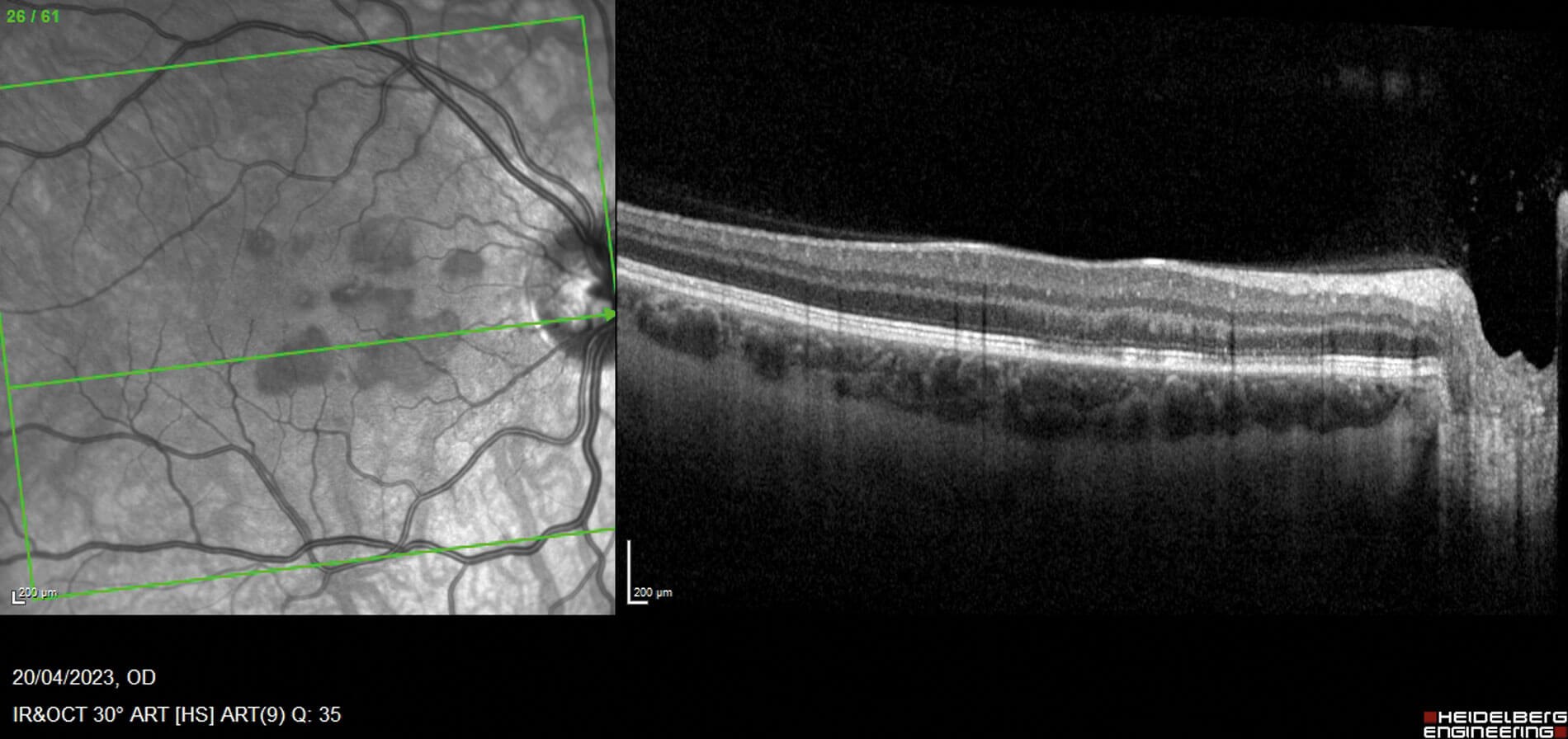
Figures 1a (top) and 1b (bottom): OCT macular view, showing hyper-reflectivity in the outer nuclear layer, with associated focal signal reduction of the inner segment / outer segment junction in the left eye (a) and right eye (b). Near infrared pictures show corresponding areas as mostly petaloid lesions, pointing towards the fovea.
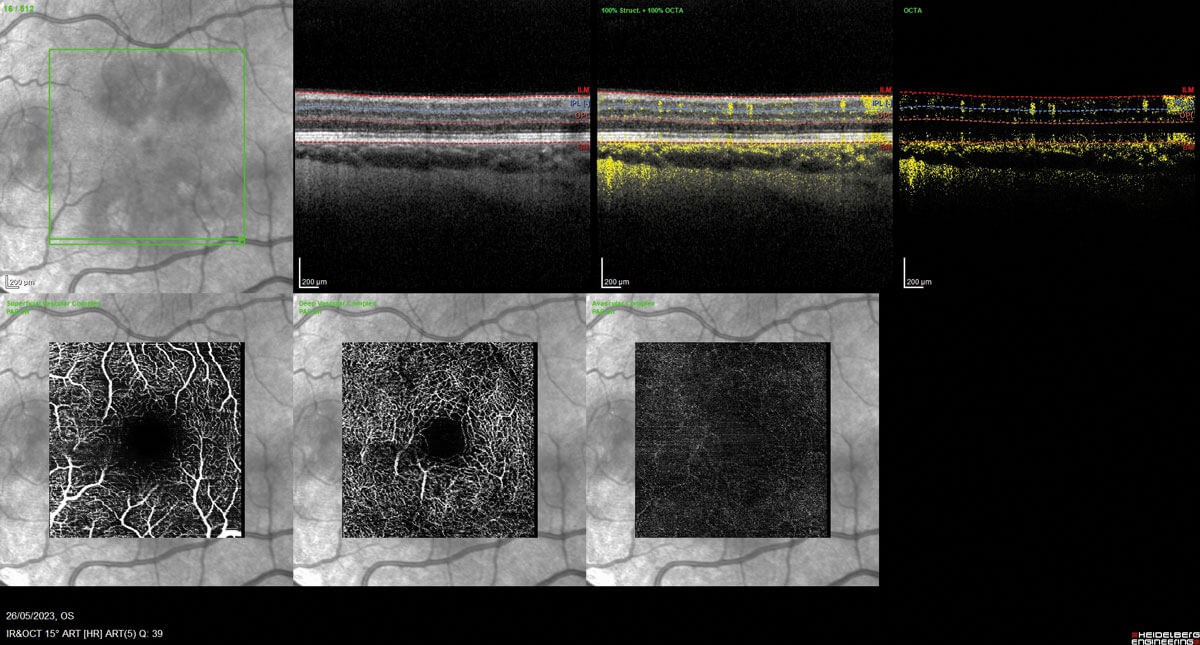
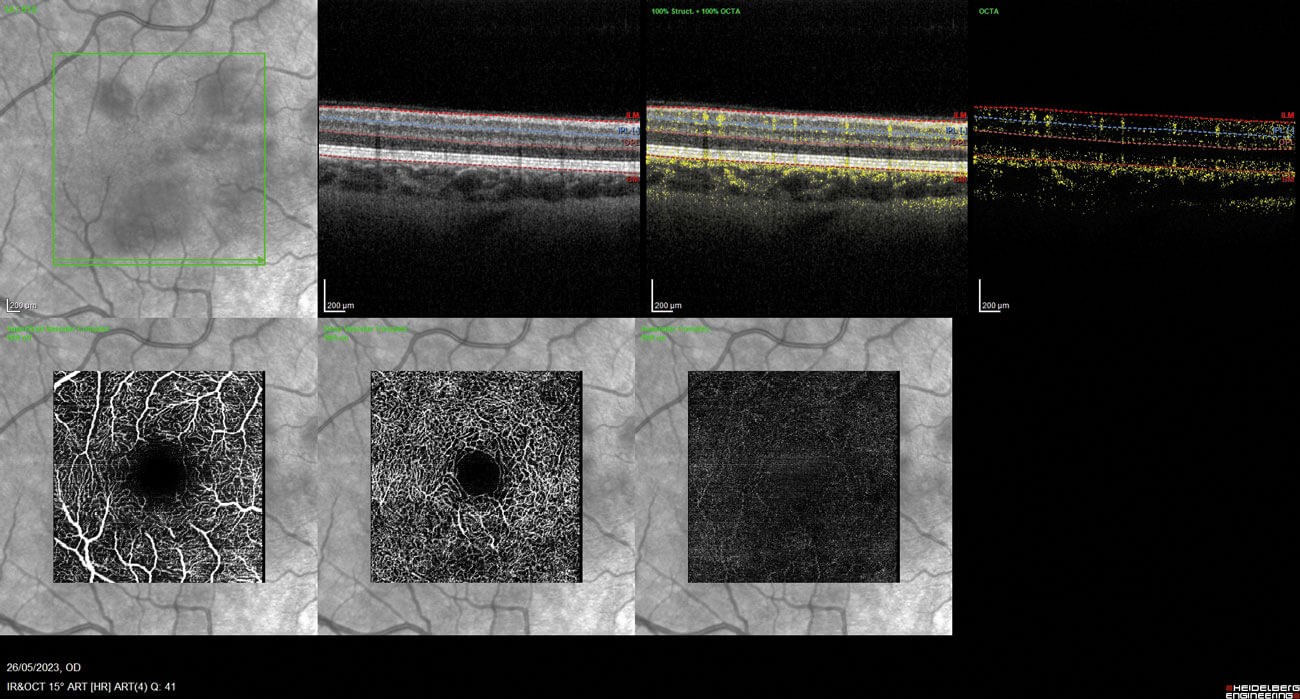
Figures 2a and 2b: OCT angiography left eye (2a - top) and right eye (2b - bottom).
Fundoscopy showed evidence of discrete foveal reflex changes, which on further evaluation with optical coherence tomography (OCT) macular view showed multiple areas of outer retinal disruption (see Figures 1a and 1b). Optical coherence tomography angiography displayed evidence of reduced flow in the deep retinal plexus, consistent with ischaemia (Figures 2a and 2b). These retinal imaging findings correlated with the patient’s subjective visual changes, as noted on their Amsler grid drawings (see Figures 3a and 3b).
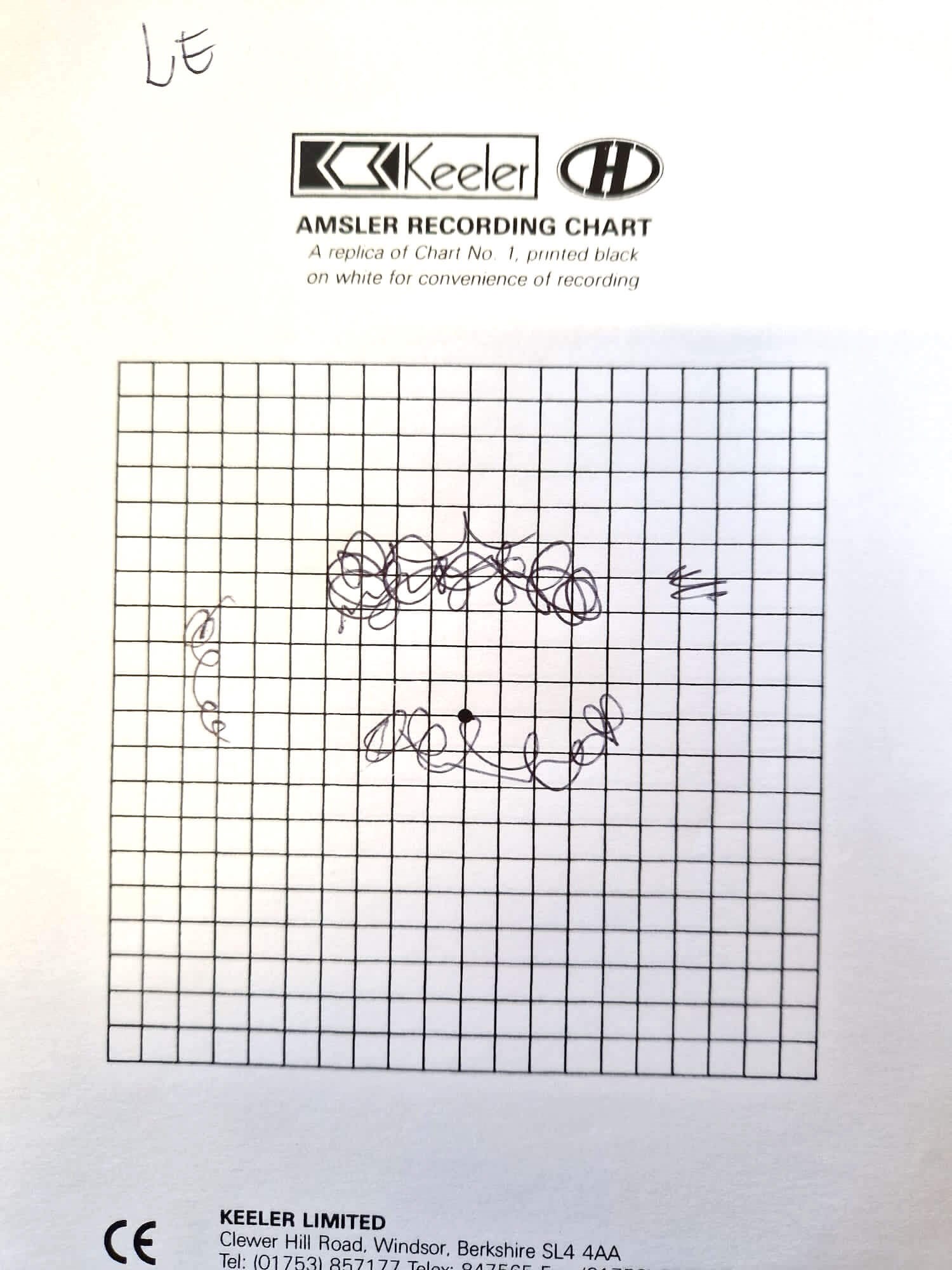
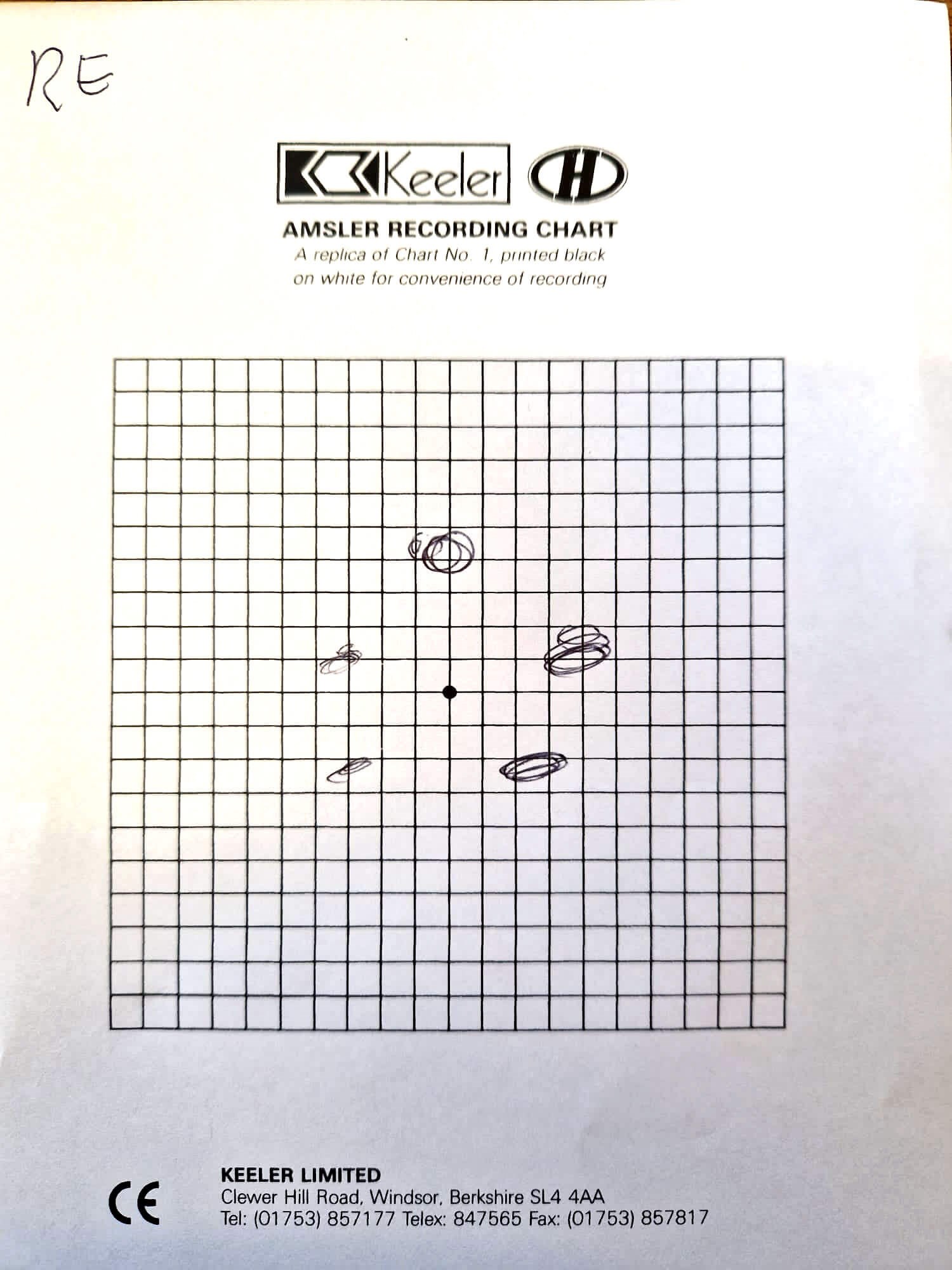
Figure 3a and 3b: Amsler grid drawings, showing deep central scotomas of
left eye (3a - top) and paracentral scotomas of the right eye (3b - bottom).
Her most recent blood tests showed evidence of raised total cholesterol (5.9) and low-density lipoprotein (3.68). HbA1c (glycated haemoglobin) and thyroid function tests were in normal range. Adalimumab levels were in therapeutic range as of April 2023. An autoimmune screen was negative for HLA-B27, HLA A29 and MPO/PR3-ANCA antibodies. The erythrocyte sedimentation rate was 2, with a serum angiotensin-converting enzyme of 31 (normal). In addition, a QuantiFERON test for tuberculosis was negative.
"Acute macular neuroretinopathy a rare condition typically affecting young women"
From the patient’s presentation and findings on examination, differentials for this presentation included conditions such as acute retinal pigment epitheliitis (ARPE), multiple evanescent white dot syndrome (MEWDS), or an autoimmune / bacterial chorioretinitis. Regarding OCT findings of hyper-reflectivity in the retinal layers, paracentral acute middle maculopathy also presents similarly.
However, the following blood tests were not consistent with possible autoimmune or infection-mediated chorioretinitis. Furthermore, the classical appearance of reddish-pigmented, petaloid lesions on fundoscopy and location of lesions in the outer nuclear layer on OCT differentiated this from distinct findings seen in ARPE and MEWDS [2].
This led to the diagnosis of severe acute macular neuroretinopathy, given the extent of the areas affected, with foveal involvement, and impact on her visual acuity.
Discussion
First described by Bos and Deutman in 1975, AMN is a rare condition typically affecting young women. The condition is characterised by visual disturbance, such as photopsia and paracentral scotomas, with respective wedge-like opacities in the macula [3]. It is most commonly associated with a precedent infection, febrile illness or noted oral contraceptive usage. Suggested mechanisms that mediate this condition include micro-thrombi occlusion of deep retinal plexus, secondary to inflammatory states such as acute Covid-19 infection [4].
"There is no current treatment for AMN, but visual prognosis is expected to be good with documentation of partial resolution of scotoma in some cases"
This case was of particular interest due to large scotomas and lesions noted on Amsler grid drawings and OCT. There is no current treatment for AMN, but visual prognosis is expected to be good with documentation of partial resolution of scotoma in some cases [5].
References
1. Bhavsar MD, Lin S, Rahimy E, et al. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv Ophthalmol 2016;61(5):538–65.
2. Sutton DK, Mahajan J, Feldman BH, et al. Acute macular neuroretinopathy. EyeWiki.
https://eyewiki.aao.org/Acute_Macular_Neuroretinopathy
[Link last accessed January 2024]
3. Bos PJ, Deutman AF. Acute macular neuroretinopathy. Am J Ophthalmol 1975;80(4):573–84.
4. Dinh RH, Tsui E, Wieder MS, et al. Acute Macular Neuroretinopathy and Coronavirus Disease 2019. Ophthalmol Retina 2023;7(2):198–200.
5. Turbeville SD, Cowan LD, Gass JD. Acute macular neuroretinopathy: a review of the literature. Surv Ophthalmol 2003;48(1):1–11.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME