The Covid-19 pandemic was the catalyst for a number of paradigm shifts in numerous industries. The demand for proxies that follow social distancing measures created a hotbed for digital solutions and transitioned these to social convention. In the aftermath, the teachings garnered from the pandemic can now be utilised to meet the demands of an increasingly globalised world, where the innate distance is no longer seen as an insurmountable burden. Here we present insights and future recommendations from a virtual ophthalmology conference hosted by Barts and the London Ophthalmology Society for undergraduates in the spring of 2021 during the Covid-19 pandemic.
Planning:
Step 1 – virtual venue viewings
To closely mirror the in-person experience of medical conferences, the conference lead had to identify a platform that could facilitate multiple keynote speakers, small group workshops, oral presentations, poster presentations, vendors, and the networking element that all delegates are able to benefit from.
Further to these challenges, ophthalmology as a specialty has a significant surgical component, so in addition it was important to find means to incorporate virtual ophthalmic suturing workshops into the day’s schedule. Many conferencing platforms were explored including Zoom, Microsoft Teams, Hopin and VFairs. The decision was made to use Hopin as this would most optimally reflect the in-person experience and meet the organisation’s budget.
The virtual venue had to facilitate workshops taking place, with subgroups of delegates cordoned to virtual seminar rooms titled ‘sessions’, while keynote speakers would continue to address the larger audience on the main ‘stage’. This capacity was also employed in facilitating the presentation of oral posters and allowing the assessing committee to ask any specialist questions directly to presenters, before deliberating on final scores in a private room. The assessing committee were ‘accompanied’ by an organiser to ensure no technical issues arose. Poster presentations were available for all delegates to peruse at their leisure in an area titled ‘booths’, in the same way that they would at an in-person conference. The booths also played host to sponsors, and a competition to keep delegates engaged during their break hour. As part of their registration to the conference, delegates were also given the choice to opt-in for networking purposes, by personalising their identification card with their contact details, and could then directly message other delegates via a one-to-one chat. A booth was also made available to all delegates to mimic the social areas of an in-person conference and allow fruitful discussions to be borne by a larger cohort. Due to the unfamiliar nature of the platform to many delegates, email correspondence was sent to delegates prior to the conference day with walkthrough videos on how to utilise the platform to maximise their experience on the day.
Step 2 – virtual suturing course
In addition to the above, 10 delegates were offered the chance to win a free suturing kit funded by the university’s Student Union and attendance to an exclusive online suturing workshop. These were awarded on a first-come, first-serve basis much like suturing workshops at in-person conferences. Kits were distributed to delegates prior to the event day. A small cohort was selected to ensure an appropriate student:teacher ratio that would best benefit delegates.
Step 3 – delivering a virtual curriculum
Two clinical teaching fellows at Moorfields and the deputy lead for Undergraduate Education were invited to lead the sessions on the day. Students received instructions of relevant equipment they would need to make full use of the workshop prior to the event day in addition to the suturing kits provided. This included basic household items such as phone cable wires and preparations of fruits to practise suturing on. The teaching team also created several videos that demonstrated how the surgical knots were made. These were uploaded to YouTube in a password protected manner and used as one of three teaching modalities on the day available to delegates. They were also made accessible to students following the event via a private link to enable further practice as students had their own kits at home.
On the day, the suturing workshop ran via four virtual seminar rooms – a main teaching room in which all teaching was delivered, and three ‘breakout rooms’ with a teacher and three / four students assigned for practice and to facilitate personalised feedback. Delegates and the teaching team navigated back and forth between their respective breakout rooms and the teaching room with each new concept being taught. The session began with a tutorial on suturing materials and equipment to help familiarise all delegates with the different tools in their kits. The teaching programme followed a macro-to-micro approach, in which the students were first taught the techniques involved on a macro level (using cable wires and a bar) followed by teaching on a micro level (by practising the sutures on fruit). Teaching was delivered through a variety of modalities including pre-filmed videos that guided students through the knots, a live demonstration via webcam delivered by the team from a ‘surgeons-view’ angle, as well as individual feedback for each knot in breakout rooms (three to four students to every one teacher) by one of the teaching instructors.
Recommendations for future application
Feedback forms were distributed to participants following the event that addressed 20 domains which broadly fell under the themes of ‘delivery’ (including platform specific features such as breakout rooms, the ability to ask questions, and the suturing kits used), ‘teaching’ (including the range of topics covered, the subject knowledge of the instructors, and the teaching modalities used) and the students’ ‘learnings’ (including how confident they felt in carrying out the different knots taught following the session). The most pertinent findings from this are summarised in Figure 1.
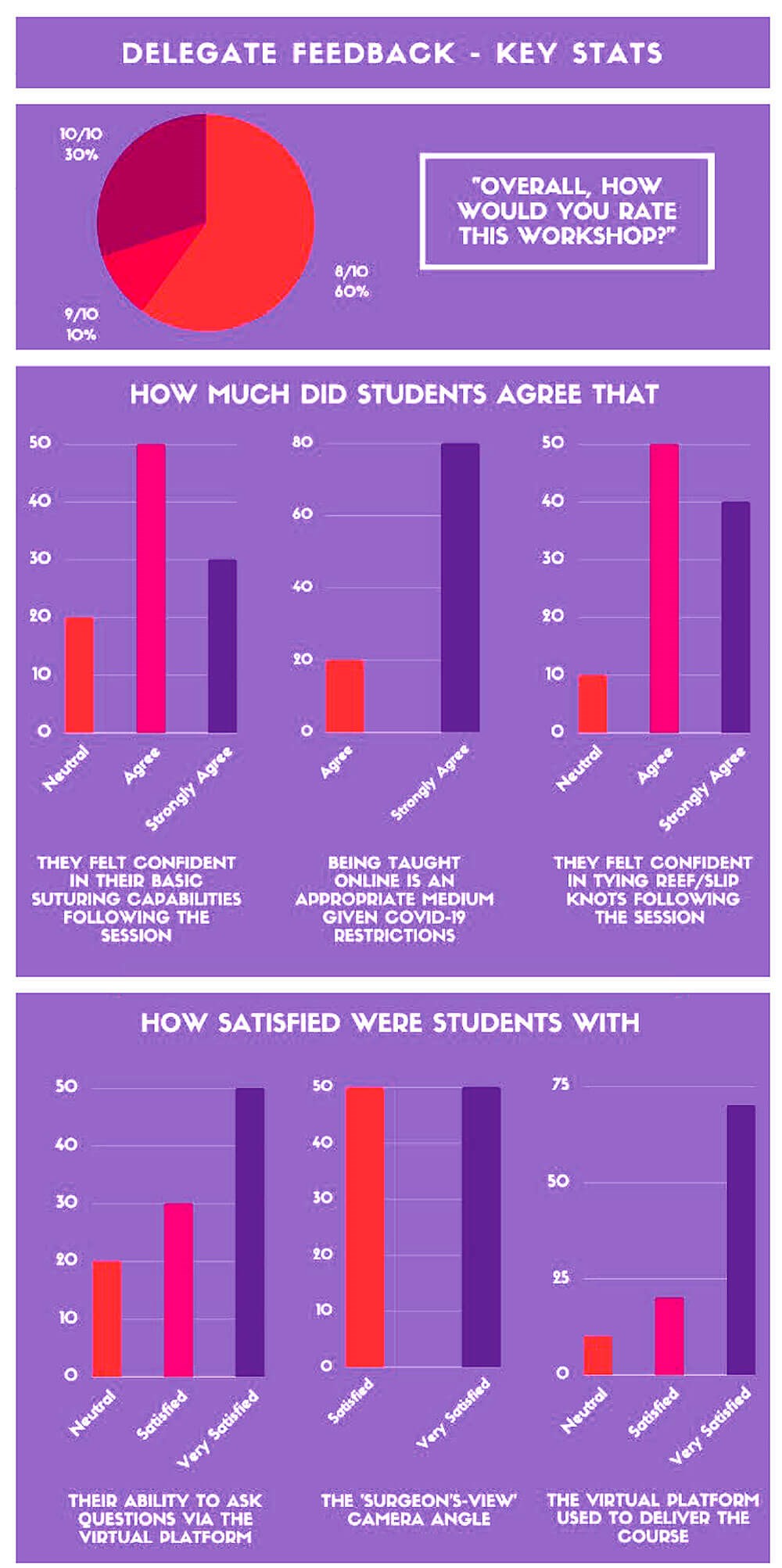
Figure 1: Delegate feedback from vitrual suturing workshop.
Participants were also invited to provide feedback on what they thought went well, and what could be improved. With regards to the former, students felt that the use of breakout rooms and personal feedback due to the small cohort size made for a particularly good teaching experience. The benefits of a macro-to-micro model of teaching in solidifying basic concepts was also highlighted. With regards to the platform, some students felt that moving back and forth between the breakout rooms and the main teaching room took up quite some time. One student lost connection and therefore could not proceed with the workshop.
Overall, 80% of delegates “strongly agreed” that being taught online in this manner was an appropriate medium, given Covid-19 restrictions. Beyond the pandemic, virtual suturing teaching such as what we offered could very well become convention – particularly when running dry labs. Further insights with a larger cohort are required to improve on this modality. An alternative move would be towards ‘hybrid’ conferences where a distinct, developed virtual experience can be offered, alongside an in-person experience, in order to reach wider audiences. Our findings demonstrate that delegates respond positively to this alternative teaching modality.
COMMENTS ARE WELCOME









