Acute angle closure is a true ophthalmic emergency that mandates timely diagnosis and treatment. The priority in initial management is to lower the intraocular pressure in an expeditious matter using medical treatments. The risk of irreversible glaucomatous optic neuropathy is positively related to the duration of symptoms and time taken to ‘break’ the attack [1].
Unfortunately, this serious ophthalmic diagnosis is often missed by the non-ophthalmic practitioner [2,3], potentially exposing patients to a poorer long-term prognosis due to delayed recognition and treatment. This situation is further compounded in settings where ophthalmologists are not on site or operate at a central unit; this can be a particular problem for district general hospitals. Anecdotally, even once the diagnosis is made it can often be difficult to acquire all the necessary topical and systemic medications required to begin treatment out of hours. We believe risk to the patient in acute angle closure can be minimised in these scenarios and propose a relatively simple tool to aid the non-ophthalmic practitioner in the timely management of this condition.
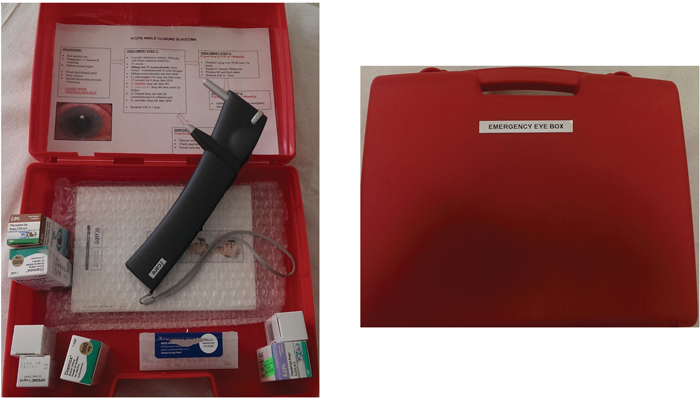
Figure 1: The Emergency Eye Box. Contents: iCare tonometer, tonometer probes, systemic acetazolamide (IV),
g. pilocarpine 2%, g. timolol 0.5%, g. dexamethasone 0.1%, g. travoprost, g. apraclonidine 1%
The emergency eye box
We have developed an emergency eye box at Salisbury District Hospital, for use in the general emergency department to address these concerns (Figure 1). The box contains an iCare tonometer, systemic and topical treatment for use in acute angle closure (IV and oral acetazolamide, topical dexamethasone, pilocarpine 2%, timolol 0.5%, apraclonidine 1% and travoprost), an enclosed guide to diagnosis and an initial treatment algorithm to be started in liaison with the on call team for ophthalmology (Figure 2).

Figure 2: Enclosed guidance to diagnosis and initial treatment algorithm for
AACG to be started in liaison with the on call team for ophthalmology.
The emergency eye box should be used to aid the non-ophthalmic emergency practitioner in the management of patients who present with a painful red eye. The aim is to pick up those patients, with a red eye, who also have a markedly raised intraocular pressure. Further refinement of the diagnosis is made by referring to an example photograph of an eye in angle closure as well as a printed sheet on the inside surface of the box. The latter highlights the key symptoms and signs (haloes around lights, corneal haze and mid-dilated unreactive pupil) in a typical presentation of acute angle closure.
Once the box was assembled, a training session was arranged at the emergency department allowing us to introduce and promote the box, train emergency nurse practitioners and doctors on the use of the iCare tonometer and provide education on the presentation, pathophysiology and acute management of acute angle closure.
We chose the iCare tonometer due to its ease of use, small maintenance requirements and lack of need for recalibration. Although the iCare tonometer has been shown to be less reliable at extremes of intraocular pressure in comparison to Goldmann applanation tonometry [4], this was not deemed to be an issue as the priority was to simply identify an eye with a markedly raised intraocular pressure.
There also needed to be a system to ensure that the medications are topped up once used and therefore liaison with hospital pharmacy was initially required to establish this system. Once the medications are used from the box they are topped up locally from the pharmacy supply within the emergency department, which is then, in turn, replenished by the hospital pharmacy who keep a log of what has been used.
Lastly, the box was secured within a cupboard safeguarded by a number-pad lock mechanism in the ‘minors’ section of the emergency department to ensure the box is not mislaid or contents lost.
Results so far
This box has been in situ for less than a year, but so far, we have seen positive responses from the emergency practitioners who have embraced its use. It has been successful in being able to identify a number of cases of acute angle closure that had presented to the emergency department, allowing their prompt successful treatment. It has also been received well by ophthalmic trainees who have found it useful to treat bed bound patients on the ward who developed acute-angle closure, highlighting its potential versatility beyond the emergency department scenario. The box has also been helpful in being able to triage acute referrals where there would otherwise have been uncertainty about the possibility of acute angle closure; it has enabled the referring practitioner to provide an intraocular pressure reading, which can be a very useful piece of extra information to the ophthalmic practitioner receiving the referral.
In summary, we believe this tool to be a helpful aid in the swift diagnosis and critical initial management of this true eye emergency and thus boost the chances of a favourable prognosis for these patients.
References
1. Andreatta W, Elaroud I, Nightingale P, Nessim M. Long-term outcomes after acute primary angle closure in a White Caucasian population. BMC Ophthalmol 2015;15(1):108.
2. Siriwarden D, Arora A, Fraser S, et al. Misdiagnosis of acute angle closure glaucoma. Age Ageing 1996;25(6):421-3.
3. Marsden J. Ophthalmic trauma in accident and emergency. Accid Emerg Nurs 1996;4(2):54-8.
4. Garcia-Resua C, Gonzalez-Meijome J, Gilino J, Yebra-Pimentel E. Accuracy of the new ICare rebound tonometer vs. other portable tonometers in healthy eyes. Optom Vis Sci 2006;83(2):102-7.
Take home message
-
Acute angle closure is a true ocular emergency but often presents itself first to non-ophthalmic practitioners.
-
A good outcome rests on timely diagnosis and prompt treatment.
-
We believe, and have demonstrated, this can be achieved through provision of a self contained tool and minimal training in its use by emergency department staff.
-
This tool can also be used in the assessment and treatment of non-ambulatory patients suspected of this condition.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME