
The past 25 years have seen remarkable advances in clinical eye care for children in the UK. This has led to both improved outcomes and better patient and family experiences. There have been substantial changes to patient pathways, major advances in diagnostic techniques and treatments, and a more robust evidence base underpinning the delivery of care.
Paediatric ophthalmology is now universally recognised as a specific sub-speciality. Ophthalmic care of children in 2018 is no longer something that general ophthalmologists do as an adjunct to their predominantly adult clinical practice. It is instead delivered in dedicated paediatric ophthalmology clinics by teams with expertise in the care of children. Advances in diagnostic and imaging techniques originally developed for adult patients (such as optical coherence tomography (OCT), wide screen digital imaging (Optos), and modern fluorescein angiography) have expanded the options available for the investigation of children. Readily available genetic testing has changed the way we approach the investigation and management of children with rare and complex eye disease. Application of new diagnostic techniques for deep phenotyping in combination with genomic testing enhances accuracy of diagnosis and prognosis. This now enables the introduction of true ‘personalised’ medicine for children with rare ophthalmic disorders.
Equally importantly, an increased awareness of social and safeguarding issues has improved child protection strategies across paediatric healthcare ensuring clinicians and their teams better protect children from harm.
We believe that these developments in medical and surgical care will ensure that paediatric ophthalmology remains one of the most exciting subspecialities well into the future. In addition, recent regulatory changes have meant that pharmaceutical companies must consider the needs of children as well as adults when seeking a licence for new treatments. In future, clinicians should be thus able to prescribe medication for children with a better evidence base of efficacy and safety. We anticipate that the need to grow and enhance the currently limited evidence base for much paediatric eye care will lead to more research and specifically the establishment of new clinical trials in this area.
Changes to the way we care for children in paediatric ophthalmology
Children in 2018 are rarely seen within a ‘general’ predominantly adult clinic, and are much more likely to be assessed in child-focused dedicated paediatric clinics, with facilities specifically pitched towards children, and by experienced staff with appropriate safeguarding training. This has substantially improved the experience of care for the children and their family. The majority of consultants who regularly deal with children now have a subspeciality interest in paediatric ophthalmology, usually following post-CCT fellowship training.
Paediatric ophthalmology clinics require multidisciplinary expertise. Orthoptists have traditionally played a key part but other allied health professionals (AHPs) such as paediatric optometrists, vision scientists and eye clinic liaison officers (ECLOs) have crucial roles in the delivery of high quality paediatric ophthalmology. AHPs often work independently, both within the hospital setting and in community clinics, and support traditional outpatient clinics by working closely with paediatric ophthalmologists. Clinics are ideally supported by paediatric nurses with the appropriate training and expertise. Examples of current modern practice would be orthoptic / optometry-led clinics in both the community and in hospital. This could include specialised follow-up clinics in, for instance, paediatric cataract, or uveitis led by orthoptists or optometrists, running in parallel with a consultant-led clinic.
All staff dealing with children now receive mandatory safeguarding training. This helps ensure that child protection issues or signs of abuse can be detected and acted upon appropriately.
Advances in imaging and diagnostic tools
Accurate assessment and monitoring of eye disease in children has always been challenging. Young children and children with neurodevelopmental problems can be difficult to examine. They may be anxious, upset or fractious and thus fail to fully cooperate. Physical limitations can also present boundaries when using instruments and techniques that were designed for use in adults. In the past, clinicians frequently resorted to ‘examination under anaesthesia’ (EUA) for a child in whom it was impossible to obtain an IOP measurement or when fundal examination was similarly difficult but very important. The availability of i-Care rebound tonometry, which can be used swiftly, without eye drops, on a child with minimal cooperation [1], has greatly reduced the number of EUAs carried out. This has been particularly beneficial for children with conditions such as glaucoma, aniridia or facial port wine stains, where regular IOP measurement is a crucial part of assessment and monitoring but repeated anaesthesia carries concerns about impact on neurodevelopment.
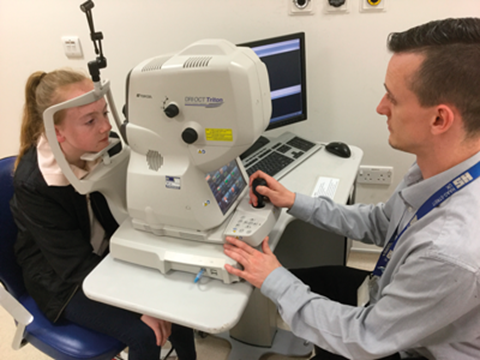
Figure 1: Young child having an OCT carried out in clinic.
OCT has also made a huge impact on diagnosis and assessment in paediatric ophthalmology. An experienced imaging technician can successfully obtain useful OCT images in a cooperative child from the age of three upwards and it has thus become invaluable in the assessment of both anterior and posterior segment paediatric pathology (Figure 1). For instance, OCT imaging of swollen optic discs can help the clinician distinguish between anomalous looking discs due to optic disc drusen as compared to papilloedema. Similarly, OCT is invaluable for retinal assessment and diagnosis (retinal dystrophies, foveal hypoplasia, developmental disorders), as well as macular oedema diagnosis and monitoring in uveitis and other conditions.
The advent of the handheld or microscope mounted OCT has meant that images can now be obtained both in infants and during surgery or examination under anaesthetic. This can be invaluable in the diagnosis and assessment of young children with nystagmus, glaucoma, retinal pathology and the retinal complications of non-accidental injury. OCT angiography is currently seldom used in children but has the potential to be a powerful tool for non-invasive delineation of paediatric retinal vascular and structural diseases such as familial exudative vitreoretinopathy (FEVR), Incontinentia Pigmentii and foveal hypoplasia.
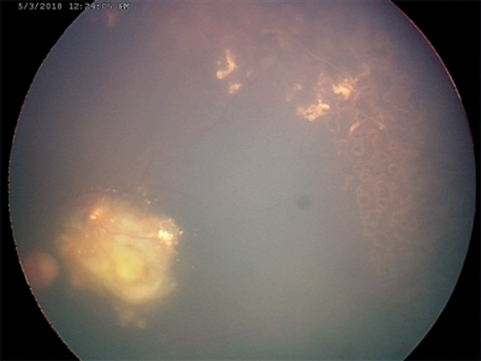
Figure 2a: RetCam image of fundus of child with Coat’s disease following laser treatment.
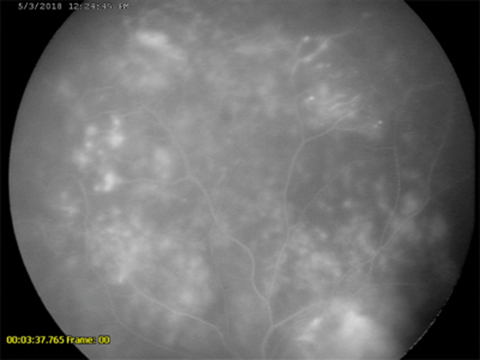
Figure 2b: Flourescein angiography of same patient, taken under general anaesthetic with RetCam.
Advances in digital fundal imaging in children have transformed diagnosis and monitoring of a wide range of children’s eye diseases. RetCam and newer more portable digital fundal imaging devices (such as PanoCam) are now routinely used in infants and young children for the documentation of retinal disease (Figure 2). Digital imaging is particularly important for the diagnosis, monitoring and documentation of retinopathy of prematurity (ROP) [2]. It has significantly enabled trained non-medical users to send images obtained in the neonatal intensive care unit (NICU) to a remote expert for interpretation – true ‘telemedicine’. This principle may be transformative for the delivery of high quality ROP care in the developing world where paediatric ophthalmologists are scarce. Digital documentation of retinal haemorrhages in cases of suspected non-accidental injury is important both clinically and from a medico-legal aspect (Figure 3).
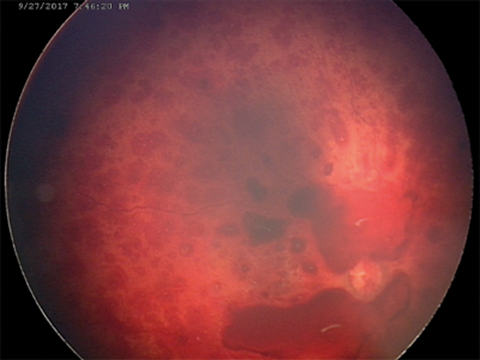
Figure 3: RetCam images of child with suspected non-accidental injury
with bilateral multi-layered retinal haemorraghes.
The images obtained are important evidence for subsequent hearings in both the family and criminal courts. Optos widescreen digital imaging can be carried out from at least four years of age in a cooperative child and provides quickly captured wide angle images (Figure 4). These are excellent for assisting the clinician in diagnosis and monitoring of both paediatric retinal disease, retinoblastoma and posterior uveitis. Fluorescein angiography and the autofluorescence functions of digital imaging systems have similarly assisted accurate diagnosis and delineation of maculopathy, retinal ischaemia and subretinal neovascular membranes in paediatric retinal disease.
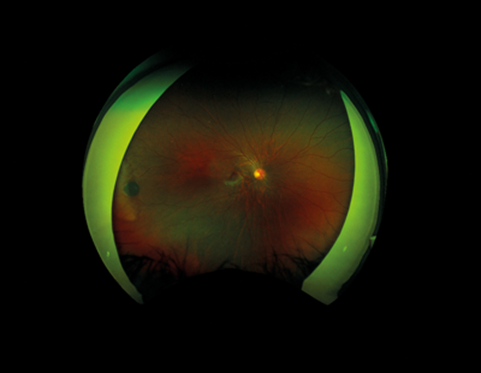
Figure 4: Optos wide field digital imaging in a 10-year-old with a peripheral CHRPE lesion.
Digital imaging equipment for documenting eye movements using ‘eye tracking’ software has become more widely available. These instruments provide detailed information for both the assessment of nystagmus and other neuro-ophthalmic abnormalities affecting saccades and smooth pursuit eye movements. This has allowed more accurate diagnosis and the planning of surgery for nystagmus related abnormal head posture.
Advances in treatment options for children with eye disease
The last quarter of a century has seen many changes to the way we treat ophthalmic disorders in children, both medically and surgically. There have been concurrent changes to care pathways and huge improvements in surgical equipment and techniques.
Advances in our understanding of the natural history of strabismus and the role of refractive error in the aetiology of squints has led to more conservative management and less strabismus surgery being performed on children in the UK [3]. There has consequently been less need for re-operations. Alternative treatment options such as ‘chemodenervation’ of extraocular muscles via botulinum toxin (Botox) have been introduced over the last 30 years for the management of paediatric squint with comparable results to surgery for management of infantile esotropia [4]. Botox is particularly helpful for management of acute esotropia (with or without sixth nerve palsy). This may have also contributed to the reduction in surgery and better outcomes.
Advances in surgical instruments and techniques used in paediatric intraocular surgery have reduced complications and improved surgical outcomes. In paediatric cataract surgery, performance of a posterior capsulotomy and anterior vitrectomy at the time of lensectomy has reduced visual axis re-opacification rates. The use of smaller incisions (23 and 25 gauge), atraumatic surgical technique and rigorous peri and postoperative anti-inflammatory regimes have reduced postoperative inflammation. It is likely that, as in adults, the use of intraocular antibiotics at surgery has reduced the rate of postoperative endophthalmitis. Other major advances include a better understanding of the indications in the management of infantile and childhood glaucoma for different surgical procedures – particularly the increasing role of modern Seton devices (such as Baerveldt and Ahmed tubes) for congenital and aphakic glaucoma.
Babies born prematurely are now not only more likely to survive than 25 years ago, but are also likely to have better structural and visual outcomes. This is as a result of improved screening programs for ROP and a better knowledge of when and how to treat sight-threatening ROP. The ET-ROP study and BEAT-ROP studies have been key in guiding clinicians in when and how to treat ROP with laser or intravitreal anti-VEGF injections [5,6]. The RCOphth guidelines for ROP screening and treatment in 2006 defined optimal screening ages and intervals. These will evolve as the use of anti-VEGF agents becomes more widespread. Surgical management of stage IV ROP has also advanced tremendously in recent years. Minimally invasive endoscopic vitrectomy has improved anatomical outcomes and reduced the need for lensectomy in infants who would previously have faced a dismal outcome.
Anti-VEGF intravitreal injections have also been utilised in other areas of paediatric ophthalmology, such as in Coat’s disease, Best’s disease and in the treatment of subretinal neovascular membranes in inflammatory eye disease.
Visual and structural outcomes for children with uveitis have improved over the last 25 years due to several factors. Better screening of at risk patients, such as those with juvenile idiopathic arthritis (JIA), has allowed earlier diagnosis and intervention for JIA uveitis before complications occur. Better care pathways have indicated early treatment with immunosuppressive drugs, when ocular disease is not controlled topically, with more efficacious immunosuppression options now available such as methotrexate and anti-TNF agents. Multidisciplinary care of children with uveitis, in conjunction with paediatric rheumatologists, has meant that the incidence of visual impairment and blindness has been substantially reduced.
Advances in evidence based medicine for paediatric ophthalmology
Twenty-five years ago there was little robust evidence for most of the interventions and treatments commonly used in paediatric ophthalmology. Complex ethical issues mean recruitment to research studies in children is still difficult, with much progress still to be made. New regulatory requirements for pharmaceutical companies requiring evaluation of medicines in children has resulted in more interest in carrying out clinical trials in paediatric ophthalmology.
There are, for example, current or forthcoming trials into the use of anti-VEGF treatment for ROP, gene therapy for a number of retinal dystrophies and evaluation of low dose atropine in retardation of myopia development. The majority of drugs used for children in the past were ‘off label’ use – as they had not been licensed for use in children. There has recently been an increase in the number of licensed topical treatments for children, giving clinicians greater confidence when prescribing for children.
Evidence provided by several key studies has changed the way in which we treat children with certain eye conditions. The Infant Aphakia Treatment Study was an American randomised prospective study of 114 infants [7]. It has provided outcome data for children with unilateral congenital cataract who underwent surgery under the age of six months, either with or without an intraocular lens. The IOLu2 study in the UK was a prospective cohort study looking at outcomes in children undergoing cataract surgery under the age of two years, both with and without an IOL [8]. The SYCAMORE study was the first multicentre UK prospective randomised controlled trial of the use of Adalimumab (an anti-TNF agent) in children with JIA-associated uveitis [9].
Diagnosis and testing for genetic eye conditions in childhood
Twenty-five years ago, many children with complex ocular disease suffered significant delay in diagnosis, sometimes until late childhood or adulthood, if at all. Precise diagnosis was not possible in many cases, and thus provision of prognosis and accurate genetic counselling was not possible. Advances in high throughput genetic testing (using either multi-gene panels or via whole exome or whole genome sequencing) has meant that genetic testing is now part of routine care across medicine.
This has impacted on investigation of many paediatric ophthalmic conditions, such as retinal dystrophies, paediatric cataract and paediatric glaucoma. Joint genetic / ophthalmology services have been established in major centres to manage access to testing, laboratory services for testing, analysis and interpretation of results, and genetic counselling. New genomic testing techniques now mean that it is possible for a patient with bilateral congenital cataract or inherited retinal dystrophy to receive a rapid, precise diagnosis of the cause, with exclusion of associated syndromic and metabolic causes, thus avoiding unproductive systemic and metabolic investigations [10,11].
Speculation on future developments in paediatric ophthalmology
Paediatric ophthalmologists are the last ‘generalists’. They require a skill set that enables them to interact with, and put at ease, both the child and their family – as well as being able to carry out a thorough and effective examination in often sub-optimal circumstances. It will remain one of the most challenging and rewarding subspecialities in ophthalmology. Great advances continue to be made in diagnosis and management of paediatric eye disease.
Advances in genomics will play a key role, and genetic testing will become much more integrated into clinical care. This will allow rapid, accurate diagnosis and ‘personalised’, targeted management for each child, together with provision of prognosis, potential for treatment and appropriate counselling for the family. Genomic, proteomic and metabolomic translational medicine will enable the introduction of new exciting therapies. Precise molecular diagnosis will be of particular benefit to children in whom gene therapy may be indicated.
The increasing number of clinical trials of medication and treatment for children will ensure that the evidence base will continue to build, so that paediatric ophthalmologists can be sure they are delivering best care for their patients. The results of such research will mean that the range of treatments routinely available for treating eye conditions in children will continue to expand.
Advances in imaging technology will continue and techniques will become increasingly suitable for use in children, and therefore used to assess a wider range of paediatric eye conditions. ‘Big Data’ sets are likely to be analysed, with the help of artificial intelligence techniques, further improving early identification of potential biomarkers of disease and thus indicators for more effective intervention. Telemedicine based on digital imaging is likely to be more widely utilised for a larger range of conditions. The clinical expertise of the paediatric ophthalmologist will, in our opinion, remain important, but the role will evolve and develop alongside these exciting changes.
References
1. Chan WH, Lloyd IC, Symes RJ, et al. Accuracy of intraocular pressure measurement with the icare tonometer in children. Asia Pac J Ophthalmol (Phila) 2015;4(6):357-9.
2. Quinn GE, Ying GS, Daniel E, et al; e-ROP Cooperative Group. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol 2014;132(10):1178-84.
3. Heng SJ, MacEwen CJ. Decrease in the rate of esotropia surgery in the United Kingdom from 2000 to 2010. Br J Ophthalmol 2013;97(5):598-600.
4. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev 2017;3:CD006499.
5. Good WV; Early Treatment for Retinopathy of Prematurity Cooperative Group. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 2004;102:233-48.
6. Mintz-Hittner HA, Kennedy KA, Chuang AZ; BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 2011;364(7):603-15.
7. Lambert SR, Lynn MJ, Hartmann EE, et al; Infant Aphakia Treatment Study Group. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol 2014;132(6):676-82.
8. Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS; British Isles Congenital Cataract Interest Group. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol 2015;99(11):1471-6.
9. Ramanan AV, Dick AD, Jones AP, et al; SYCAMORE Study Group. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med 2017;376(17):1637-46.
10. Gillespie RL, O’Sullivan J, Ashworth J, et al. Personalized diagnosis and management of congenital cataract by next-generation sequencing. Ophthalmology 2014;121(11):2124-37.
11. Musleh M, Hall G, Lloyd IC, et al. Diagnosing the cause of bilateral paediatric cataracts: comparison of standard testing with a next-generation sequencing approach. Eye (Lond) 2016;30(9):1175-81.
TAKE HOME MESSAGE
-
The care of children with eye conditions has been transformed over the last 25 years
-
Introduction of new treatments, improved evidence base for care, and the integration of genetic testing into clinical care are going to lead to vastly improved clinical outcomes and patient experience
-
Paediatric ophthalmology is now one of the most exciting sub-specialities in ophthalmology due to rapid pace of development in both clinical and surgical care
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






