The Art is long and Life is short. So goes the dispiriting tag in Latin and flung from day one and at regular intervals thereafter at idle medical students who, inevitably brainwashed, come by graduation to believe that the only way to be a good doctor is to make the art even longer and to suffer into the bargain. The problem with medical schools is that we are told endlessly by our teachers how much we have to study but what they never tell us, is how.
My insight into techniques of collecting usable information began as uncertain little buds, almost killed on the bough by fear that my teachers couldn’t possibly be wrong. But the buds were saved from an early death by, of all people, the ophthalmologists, in what was effectively a course on how not to learn anything. And in all their recommended textbooks the doctors wore spats, wing collars and pince-nez and looked as if they had just been chatting to Joseph Lister. Their approach to study belonged to the same era.
The magic simplicities of the eye were lost in a flood of ophthalmobabble and lost as well, was the attention of most of my year. It was as if we were being shown by conjurors how to put a rabbit back into the hat. I got 20% in the class examination. You couldn’t in fact get less, because 10% was awarded for recognising an eye and then another 10% for knowing there were generally two.
But this failure to catch the essence of any subject is not limited to ophthalmology. My first golf teacher told me the object of the game was to hit the ball, a point I had already taken on board. Then, instead of giving me two principles I couldn’t forget, he bombarded me with 15 details I couldn’t remember. What followed requires no description.
And how many children, eager with their first steps at the piano, find as adults that they were also their last steps? The teaching system, geared to the concert platform, guarantees that everyone else, the majority that is, end up unable to play anything that anyone wants to hear.
If all that sounds familiar, have courage. The Art need not be long and here is the secret to making it short.
The first thing is not to waste time relearning something you already know like physiology and pathology, and taking as essential new reading all those repetitions of the same old stuff in the slightly different jargon of different specialities.
The eye, despite all attempts to persuade you to the contrary, follows all the old familiar medical rules and the only difference is that half of it is transparent. We all know that as a fact, but it needs to be re-stated because the slight physiological variations found in the eye and not elsewhere in the body, exist because of this clarity.
The clear tissues require blood substitutes that are also transparent.
Again, obvious but I don’t recall reading that in any of the recommended texts when I was preparing for the Fellowship examination.
The second thing is to hold your knowledge in a fixed framework which, incidentally, can apply to any clinical speciality. It is much easier to hold facts that are by nature diffuse within a structure designed to be rigid. This diagnostic structure is easy to fashion because you know its components already; they are four in number:
- Physiology
- Pathology
- Essential symptoms
- Essential landmarks of examination.
There is a little list that goes with each of these sections and each must be memorised to be retrievable without hesitation.
If all this appears simplistic, be patient and be assured that memorising each section is the key to using what you already know to discovering that you already know more.
Disease is the disturbance of the physiology of any organ by any of the well established pathological processes.
- Patients can then describe what they are experiencing within a fixed range of symptoms, although what they say is rarely within a fixed range of words. Their very understandable terror doe not make for precision. So when patients begin with the statement, “to let you understand, doctor,” you can be sure you will not do anything of the sort.
- You must listen but you must also edit, directing their natural volubility into a useful format with firm sympathy.
- The doctor, then armed with the relevant story, travels along an unchanging sequence of stations in search of appearances that will explain what has happened or is happening or what has not happened.
- Once an explanation is to hand, treatment consists of reversing what has happened according to a brief system of management, to be described later and itself also rigidly framed – clinical medicine in a nutshell and another small sequence to be committed to the memory level of instant recall.
Physiology
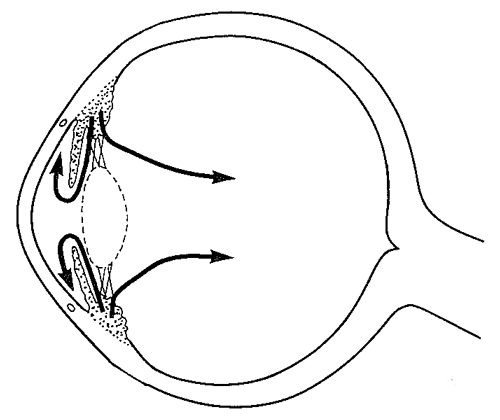
I will not insult you by going through ocular physiology but the flow of aqueous merits a comment. It is the one activity of the eye not found elsewhere. Most non-ophthalmologists never give it a second thought and if they do, it will almost certainly be wrong. They will imagine it is there to cause glaucoma and not realise that that word is used in at least six different ways without any warning that the meaning has been changed.
To understand aqueous is to understand the eye.
Whatever the ocular complaint, the first question must be, has something affected the aqueous flow?
Every part of the eye produces its own symptoms of malfunction, but not so the aqueous circulation. The intraocular pressure can rise to spectacular levels and we will not know that unless we measure it as a routine just as we do with the blood pressure.
I remember making this statement in a textbook only to read in a sneering review:
“The author says we must always ‘think aqueous’. I have to confess I have no idea what he means.” Evidently the art of making ophthalmology incomprehensible was not confined to my medical school.
As for the other transparent tissues, the cornea remains clear partly because of its inner structure, the endothelium and by grace of the alliance of the external eye – lids, tears and conjunctiva.
The lens loses its focussing flexibility with age and its main response to insult is to lose its clarity.
All would rather give up their special quality in order to survive which is why, for example, a cornea, ravaged by infection will allow forbidden blood vessels to invade its increasingly opaque structure, bringing sustenance and continued existence – at a price.
Figure 1: Obvious disturbance to the outer eye can produce less obvious
disturbance to the inner eye. Whatever happens to the eye, ‘think aqueous’.
Pathology
A discipline we have all been drilled in and another of those subjects where the quality of the textbooks tends to be measured in kilograms. Such heavy reading is clearly mandatory for specialists upon whose decisions the fate of frightened people is decided. For the rest of us, we need only use the principles which we already know and modify them slightly in relation to the physiology of the clear tissues.
All parts of the body can be damaged by something out of the pathological canon but the list of potential causation is the same, no matter what part is affected:

In the next article, I want to show you how basic principles, using inflammation as an example, can be confidently applied to the eye, but that must come after we have formed a routine for examining the eye and have recovered from the revelation of how easy it is.
Symptoms
With the proviso that you must elicit a history rather than be swept aside by it, what patients tell you must be your guide to what bit of the eye is affected and how.
Complaints come under five headings.
1. Vision
The eye is a sensory organ so the prime symptoms must relate to its prime function which is to see. Although visual stimuli are perceived by the retina, its behaviour is not all of a piece. It splits into:
Central, i.e. the ability to make out detail (macula).
Field, i.e. everything except the centre, and remember that when people say left eye, they often mean left side disturbance in the binocular field, a distinction about which questioning might not produce an immediate answer.
The assumption commonly held is that central vision is the only kind of vision and the quality of an eye is popularly based on that, an eye being dismissed as useless if it has only field vision. Well none of us would like to lose either field or macula but, if one has to lose one, then the field must win every time.
With an intact macula but no field, one can read a book if one can find the book but one cannot navigate around a room without help. With no field vision, one is effectively blind. With only field vision one might not read or drive but one can do just about everything else.
Central visual problems will be described as:
- Distortion
- Actual loss More general complaints will be of:

2. Double vision
Here is another area rich in careless language. People most often say ‘double’ when they mean simply blurred.
You must ask the question – does the patient mean actually two images or merely one image blurred?
Next must be established if the doubling occurs with:
- both eyes open?
- one eye open?
If they actually do mean two, as often as not, the doubling affects one eye only because of some opacity in the clear media, usually the lens, splitting the image.
Genuine binocular doubling is by far the least common.
I remember asking a Fellowship candidate how he would manage a 60-year-old man who was complaining of double vision? He took me at once into the higher flights of extraocular muscle surgery when I just wanted him to establish what sort of double vision he would be dealing with.
History first and then what to recommend following examination.
His response unfortunately carries also an indictment of the examination system which creates its own atmosphere of terror when any question appears to demand the most complicated answer possible.
Once, in a MRCP examination not that long ago, a candidate who volunteered endocrinology as a special interest was asked how he would recognise a patient with pituitary deficiency were he to see her walking along the street. Without hesitation, the answer was, “Atrophied breasts and absent pubic hair.”
Alas, complex teaching will without doubt produce complex answers but not, unfortunately, clinical common sense. As someone said, “the trouble with common sense is that it is not common.”
3. Watering, with or without discharge
– self-evident.
4. Pain
– to be evaluated as pain anywhere.
5. Change in appearance
When people say their eyes seem different, they do not mean the actual eyeballs, they almost always mean the lids and lashes and perhaps the conjunctiva if it is red. From our side, we do not require to read up what the face should look like. We see them around us every day.
Examination
The essence of eye examination is very simple and inevitably made incomprehensible. A few years ago, a drug company, trying to promote its general practitioner range of remedies for the external eye, produced a leaflet listing 27 varying observations that, correctly made, would lead to the confident prescription of one of its patent cures. Now, no drug company of any consequence would put its name to such a document without first seeking advice from an oculist. I am certain they did just that and I am surprised that they were given only 27 ‘signs’.
This approach belongs to the ‘Guess and Hope’ school of ophthalmology. The technique is that you guess what’s wrong, hope you’re right and take a handful from the 27 ’signs’ just in case someone asks you for an explanation.
The magic phrase heard over and over again is – “What do you make of that fundus?”
The proper answer is: “Nothing until I have heard what the patient has to say and then gone through the ocular equivalent of Observation, Palpation, Percussion, Auscultation.”
You frequently hear it from physicians who would quickly slap down their residents if they dared so to use the stethoscope out of sequence. Yet they preen themselves on picking up retinal obscurities invisible to their colleagues and, it has to be admitted, frequently invisible to themselves and without examining the eye first which of course, nobody taught them to do. And they claim their discoveries in a sunlit ward with a dying battery and the pupil undilated.
Now, nobody would dream of commenting definitively on the inside of the eye before dilating the pupil and indeed before examining the eye. Otherwise, it would be like sweeping the floor with a toothbrush in search of a pin that might not be there and in fact, might not be a pin or like deciding the colour of the wallpaper in a darkened room.
In a well known atlas of fundal appearances, I came across a photograph of a patch of blood shaped like the map of Australia lying in front of the retina. The caption beneath read ‘Myeloid leukaemia’. The implication was clear; a haemorrhage shaped like New Zealand would have indicated ‘Lymphatic leukaemia’.
This is manifest nonsense. All you could tell from either appearance was the presence of a pre-retinal bleed, yet such a statement in a recommended text shows the pervasive influence of the Guess and Hope school.
Why do we not come clean and admit that the direct ophthalmoscope, despite its constant appearance in TV medical soaps is a very limited instrument? For a start, it magnifies and cannot, even in the best of hands, reveal in their entirety those lovely coloured illustrations that textbooks so love. All it can show is little circles of the same illustrations and in ‘difficult’ eyes, like those of high myopes, it may reveal nothing at all. I have not used one since I was a registrar.
So with the ophthalmoscope relegated to the last bit of the examination technique, this is a good moment to define precisely what comes first. And definitions involve those words we use so carelessly.
When you examine the eye you do not look at signs, you look for them. What you actually look at is a sequence of specific stations, stopping points, if you like, around the eye and at each one you record what you find – normal or abnormal.
There are only seven examination stops, not 27, and they never change. In fact, if you roll central vision for Distance and Near into one, there are only six.
What you pick up at each of these halts can now be called signs. You do not decide what is wrong in advance, bending the findings to prove your conviction.
You make your six stops and with your findings, positive and negative, you will know what the ophthalmoscope is going to tell you. I conducted my entire practice following this system.
1. Central vision
It is customary to measure for distance first, then for near, but sometimes it is possible only to do it for near which, in fact, is a more accurate measure of macular function. And never scorn the pinhole.

Figure 2: Every bundle of rays from every point is reduced to one ray and each one of them is in focus. The ray through the macula is the vital clinical one. If the central vision improves with a pinhole, it can improve with glasses.
2. Field
In a subject where tradition has so often taken the place of reason, the clouds of traditional nonsense reach their thickest with the so called ‘confrontation field’. The given theory is that you compare your field with that of the patient, the untested assumption of course, being that yours is normal. Why should this be required? I cannot think of any other examination in any other discipline of medicine that calls for such a comparison. If consulted by a patient with a sore foot, would you feel obliged to take off your shoe?
Then, in addition to its shaky theoretical foundation, its practice seems designed to elicit no information because the version foisted on novices mixes what it can do well with something that it can’t. I have watched in despair during the fellowship examination as candidates try in vain to duplicate what they imagine the examiner wants, winking one eye half shut and squatting like a Sumo wrestler to bring their eyes level with those of their patient. Then they hold up one or two or three fingers, sometimes a pen or a red dot in search of a scotoma, any scotoma – every manoeuvre half way between their eyes and the patient’s. Apart from being completely ludicrous, nothing is discovered, neither outer rim nor inner defect. The temporal crescent cannot be tested for half way between patient and doctor. Each could have pituitary enlargement and neither be aware of it.

Figure 3: The disc with the pinhole should be held about one inch (2.5cm) before the eye. Leaning on the cheek keeps it steady. Multiple pinholes do not place such a premium on steadiness. And usually one wil be found by the patient. The pinhole can be used for near vision as well. The capacity to make out the smallest print, despite a poor performance for distance, indicates an intact macula. No improvement with a pinhole means the problem is not a refractive error.
The idea that you can pick up a scotoma without being aware of what scotoma you suspect is equally doomed to failure. How many of us could find the blind spot if we didn’t know precisely where it was? The hand movement field is meant to pick up hand movements at the outer edges of the field, not gaps within it. It is very good at doing that without ridiculous bodily contortions. And if any defect is found, then that is the time to produce a field analyser, not before. And remember, the machine can only produce a chart of the field. The analyser is you.
In truth, no amount of bogus theorising can disguise the fact that you can’t compare two fields in their entirety, so why try to compare any of them? After all, medicine is full of things we have to know, why not the field as well?
If confrontation is still demanded because that is the way things have always been done, then there is only one exact position to compare the temporal crescents and that is cheek to cheek when the testing hand would be in the perfect position but alas, seen by no-one. It is time the whole charade was consigned to where it belongs along with the spats, the wing collars and the pince-nez.
We all know the shape of the monocular field is like a recumbent pear so why not just pick up its contours, remembering that its longer temporal edge lies almost behind the lateral orbital margin? When all is said and done, this is part of the cranial nerve assessment, already learned in neurospeak so there is no need to duplicate it in ophthalmospeak.
3. Cornea
4. Pupil
5. Anterior chamber
Each of these is one of the six stopping points but with a simple torch, preferably one with a concentrated beam, examination of all three can be seamlessly and swiftly carried out in sequence.
We all know the normal arrangement of eyelids, eyelashes and conjunctiva and these together with any redness will be observed en passant.
- The cornea can be stained if necessary.
- The pupil reactions are part of the cranial nerve routine.
- The gap between the iris and cornea can determine if the eye might be vulnerable to angle closure, another absurdly simple test. Nevertheless, examination candidates have frequently either never been made aware of it or somehow make a hash of it. A beam from the same torch shone across the iris plane will, in the safe eye, illuminate the entire iris. In the potentially vulnerable eye, the iris remote from the torch will be in shadow.
All three features can be looked at in less time than it takes to write them down.
Five stopping places and but one to go.
6. Intraocular pressure
Of course formal measurement is done with a tonometer but if one is not to hand, the fingers can be very informative. The eye turned downwards will take the upper tarsal plate out of the way and so allow palpation of the globe through the thinnest part of the upper lid. The secret is to keep one finger static in order to let the moving finger show the degree of fluctuation.
So those are the six stations. The ritual has been completed. The direct ophthalmoscope may now be flourished but you already know all you need to know.
To illustrate my message, let me give you a rather sad example of every rule of history and examination being broken by a very senior consultant, with tragic consequences. He referred to me a patient, whose retina had been detached for some months, accompanying his referral with the airy comment, “You won’t be able to do anything, old boy.”
Well of course he got that bit right but what he didn’t tell me was that the lady had been complaining repeatedly of visual loss for several months. He ascribed the loss to cataract and her repeated complaints to verbosity and indeed, told her she talked too much. He couldn’t see the detachment through the cataract with his direct ophthalmoscope for which no-one could blame him, but he could have picked up the gross field defect with his hands if he had gone through the ritual which he hadn’t. And his direct ophthalmoscope had not managed to get far enough out to the periphery to find a large horseshoe tear near the lower temporal ora in the other eye.
So there you have it. I worked out the idea for the other specialities as a medical student but could not believe in it until long after graduation. It does save needless effort and leaves no uneasy feeling that you might have missed something because your framework is firm, complete and remembered at brainstem level.
 Figure 4: A dense cataract might stop the peripheral retina from picking up hand movements in the visual field. It would need to be exceedingly dense to prevent awareness of light in the four quadrants.
Figure 4: A dense cataract might stop the peripheral retina from picking up hand movements in the visual field. It would need to be exceedingly dense to prevent awareness of light in the four quadrants.

Figure 5: The outer limits of the visual field picked up with hand movements.
State of cortex irrelevant

Figure 6: In-flow defect. Light presented to the healthy eye (left) constricts both pupils.
Light presented to the affected eye (right) constricts neither.

Figure 7: The back of an extended hand, like the iris of a deep anterior chamber, can be illuminated.
That of a flexed hand, like the iris of a shallow chamber, cannot.

Figure 8: Using the ophthalmoscope as a torch to determine
the depth of the anterior chamber - the eclipse test.

Figure 9: Eclipse test negative - the anterior chamber is deep and none of the iris in shadow.
The pupil may be dilated with impunity.

Figure 10: Eclipse test positive - the iris surface remote from the beam is in shadow.
Angle closure possible. Pupil not to be dilated by topical or systemic medications.

Figure 11: Not everyone has access to a tonometer. The hands lean on the forehead, while the index or middle fingers are held firmly together pulp to nail and firmly on the eye above the lateral end of the tarsal plate. A slight movement of one finger sets up a shimmer of fluctuation that is sensed by the other finger. This technique may record ‘hard’ by mistake but never ‘soft’ by mistake.

Figure 12: Normal fundus - African with choroidal markings obscured by pigment retina.
The disc shows physiological cupping that might be graded 0.3.
TAKE HOME MESSAGE
-
The eye is half transparent and requires clear blood substitutes with delivery mechanisms which happen to be made up of commonplace tissues, the physiology of which you already know.
-
Aqueous is the key difference.
-
pathology principles apply to the eyeball and the external eye.
-
Symptoms are limited.
-
The ophthalmic ritual has six stopping points.
-
The secret is to know the above sections and sequence by heart so that each bit of information you collect has a place where it belongs which you know by practised instinct.
-
Record what you find and what you do not find.
-
You might then even see something with the direct ophthalmoscope, which is thus the seventh stopping point but one not nearly so important as the other six.
Acknowledgement
The images were kindly reproduced with the permission of the publisher from: Chawla HB: Ophthalmology. Churchill Livingston; 1993.
Declaration of Competing Interests: None declared.
COMMENTS ARE WELCOME