Since the early 19th century, physicians and surgeons have been working together in eye clinics and hospitals to bring about the best outcome for the patients.
From the early Babylonian age, important advances in ophthalmic knowledge arose in a stuttered matter, as development of anatomic and pathologic knowledge occurred slowly. The term “ophthalmology” refers to the branch of medicine and surgery which deals with the diagnosis and treatment of eye disorders. During and beyond the Middle Ages, this was considered to be “the domain of itinerant quacks and charlatans” and the practice was the domain of the oculist.
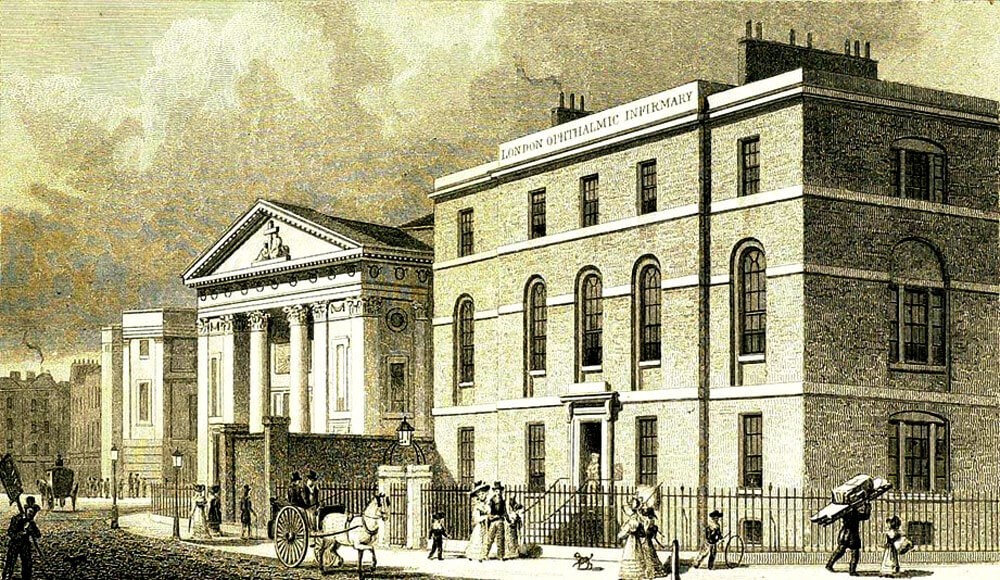
London Ophthalmic Infirmary at Finsbury (Moorfields Eye Hospital). An antique line engraving
by R Acon after Thomas H Shepherd. Published in 1829. Credit: Motco Enterprises Limited.
It was the early 19th century which saw the transition from the “oculist” to the “ophthalmologist”, as the practise of ophthalmic care became more formalised. The year 1804 saw the opening of the London Ophthalmic Infirmary (later known as Moorfields Eye Hospital). Here, staff at any one time consisted of a surgeon and physician, working in tandem to manage ophthalmic cases with an integrative approach [1]. Surgical technique in ophthalmology progressed rapidly and specialist surgical training eventually predominated in the later part of the 19th and early 20th centuries. The role of the ophthalmic physician gradually faded.
However, a renaissance took place in the early 20th century, prompted by ophthalmologists such as Rayner Batten who described “the need of ophthalmic physicians for the advancement of ophthalmology” thus:
“[...] ophthalmic physicians who do their own ophthalmic work and have to live, so to speak, with their own ophthalmic failures and to study ophthalmic cases from a physician’s point of view and with a physician’s experience.” – Rayner Batten, Western Eye Hospital, 1919 [2].
As surgical techniques and outcomes improved, so too did understanding of disease. There was greater awareness of the possibility and importance of working in conjunction with other physicians to optimise the care of patients with ophthalmic disease secondary to underlying systemic disease [3].
“[...] I have ventured to say that a considerable part of the field of clinical ophthalmology requires not the art and craft of the surgeon, but the diagnostic and therapeutic methods of the physician.” - Dr C O Hawthorne, 1919.
Nevertheless, it still took a few decades before this new specialty was formalised, and 1995 saw the establishment of a training programme, with the purpose for medical ophthalmologists (or ophthalmic physicians) borne from the statements of Rayner Batten and Hawthorne:
“[…] skilled in ophthalmic medical diagnosis, in relating systemic medical disease to ophthalmic conditions, in assessing the general medical status of patients who have primary ophthalmological disease, and in prescribing the most appropriate drug therapies and monitoring schedules for treatment of medical sight threatening diseases.” – Royal College of Physicians, 1995 [4].
Medical ophthalmologists (also known as ophthalmic physicians) are doctors who diagnose and treat medical eye conditions which are related to systemic diseases [5]. At its core is the tenet that each patient case presents individually, and the reasons why a condition has manifested in the eye and the body can have many factors. When eye inflammation is the first sign of a body condition, it is crucial that the whole patient is investigated and treated, not just the eye. Treatment incorporates the overall health and wellbeing of the patient and a focus in managing the drivers for disease. The United Kingdom is unique in being the only country in the world which provides specialised training in this specialty.
"In the joint ophthalmic clinic or service, an ophthalmic physician (or medical ophthalmologist) works alongside surgical colleagues in a myriad of ophthalmic subspecialties to ensure that patients are managed from a holistic perspective, uncovering clues which can help diagnose and treat complex patients, whose care might often involve many other specialties"
In the current era, there are many systemic diseases which can affect the eye, and approaching cases as a team can be invaluable, in order to bring about the best outcomes for patients [6]. Examples of diseases include uveitis, scleritis, thyroid eye disease, lung diseases, strokes, brain inflammation, pituitary diseases, vasculitis, rheumatoid conditions, infections, cancers, bowel problems, skin and mucous membrane problems, vascular diseases such as high blood pressure and diabetes, genetic diseases and all the complications relating to these conditions.
In the joint ophthalmic clinic or service, an ophthalmic physician works alongside surgical colleagues in a myriad of ophthalmic subspecialties to ensure that patients are managed from a holistic perspective, uncovering clues which can help diagnose and treat complex patients, whose care might often involve many other specialties.
On 22 March 2023, the Medical Ophthalmology Society UK (MOSUK) meeting will take place, and will cover two such examples. In the morning, there will be an Orbital Inflammation Symposium, covering a range of orbital disease processes which might benefit from integrative care. This includes diseases for which we are only just building a knowledge base. In the afternoon, we will have an annual guest lecture covering Mucous Membrane Pemphigoid.
TAKE HOME MESSAGES
-
There are numerous diseases which straddle the eye and systemic disease, and a holistic, multi-faceted approach is invaluable.
-
Ophthalmic physicians and surgeons can work together for the benefit of the patient.
Further Reading List
-
Joint Royal Colleges of Physicians Training Board (JRCTB):
https://www.jrcptb.org.uk/specialties/
medical-ophthalmology -
Physician Higher Specialty Training Recruitment (NHS):
https://www.st3recruitment.org.uk/
specialties/medical-ophthalmology -
Health Careers – Medical Ophthalmology (NHS)
https://www.healthcareers.nhs.uk/explore-roles/doctors/
roles-doctors/medicine/medical-ophthalmology -
Royal College of Physicians – Specialty Spotlight
https://www.rcplondon.ac.uk/education-practice/
advice/specialty-spotlight-medical-ophthalmology -
Gully CM, Williams G, Olson J. A career in medical ophthalmology. BMJ 2008.
http://careers.bmj.com/careers/advice/
A_career_in_medical_ophthalmology
References
1. Tracher E. The history & traditions of the Moorfields Eye Hospital: one hundred years of ophthalmic discovery & development: Collins, E. Treacher (Edward Treacher), 1862-1932.
https://archive.org/details/b29978038
Last accessed November 2022.
2. Batten RD. The need of ophthalmic physicians for the advancement of ophthalmology. Proc R Soc Med 1920;13(Sect Ophthalmol):11-7.
3. Hawthorne CO. Discussion on Mr. Rayner D. Batten’s paper, “The need of ophthalmic physicians for the advancement of ophthalmology”. Proc R Soc Med 1920;13(Sect Ophthalmol):18-27.
4. Dick AD, Forrester JV. The ophthalmic physician: an indulgence or a necessity? Br J Ophthalmol 1996;80(9):782-3.
5. Sacks JG. Eye disorders: looking at the eye for clues to systemic disease. Postgrad Med 1976;59(3):181-4.
6. Whitcup SM. The eye in systemic disease. Arch Ophthalmol 1991;109(4):478-9.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






